Clostridium difficile
What is Clostridium Difficile?
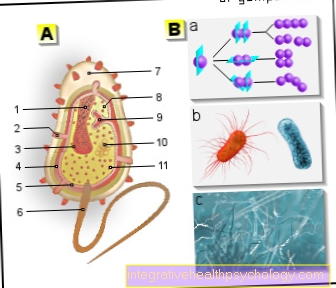
Clostridium difficile is a rod-shaped gram-positive bacterium. As with all clostridia, they are anaerobic bacteria, i.e. bacteria that cannot tolerate or need oxygen. They are spore images and can thus survive for a long time.
Many people carry this germ in their intestines without getting sick. However, if Clostridium difficile reproduces too much, it can cause severe intestinal inflammation and blood poisoning. Certain antibiotics can defeat Clostridium difficile. There is a relatively high level of infection with the bacterium in hospitals because it is very contagious.

Causes of the Disease
For a clostridial disease to occur, the bacterium must first be present in the body. Some people, especially young children, carry Clostridium difficile permanently in their intestines without becoming ill.
However, Clostridium Difficile is also highly contagious when in contact with body fluids. The bacterium or its spores can easily spread through entire hospital wards via the hands of hospital staff, which is why it is assumed that around 40 percent of the population is infected.
For the pure colonization with the germ there must then come an internal cause for the disease to break out. One cause is long antibiotic therapy. Clostridia are very resistant to many antibiotics.
The normal intestinal flora is destroyed by the antibiotic and the clostridia can multiply more easily. The clostridia multiply so much that disease occurs. The bacteria produce a poison, which then causes inflammation of the intestines with severe diarrhea.
Other causes of a disease outbreak include immunosuppression, old age, chemotherapy or radiation therapy, pre-existing chronic intestinal inflammation, and immune system disorders.
Also read this article: Infectious diarrheal diseases
Does Clostridium difficile occur in a healthy gut?
Clostridium difficile can also colonize a healthy intestine without an outbreak of disease.
About five percent of all people carry the bacterium. Small children in particular are often carriers of Clostridium difficile.
Hospital patients are even carriers of the germ in 40 percent of cases, as the risk of infection by hospital staff is significantly increased and spores have also been found in the air in intensive care units.
Detection of Clostridium difficile in the stool is therefore not necessarily pathological.
diagnosis
Since clostridia are also found in a healthy intestine, a stool sample with the detection of clostridia is not suitable for diagnosis. A clostridial diagnosis is often a clinical diagnosis.
The combination of long-term antibiotic use, severe bloody, foul-smelling diarrhea, abdominal pain and fever together with the stool test result in the diagnosis of clostridial-induced diarrhea.
In the laboratory, leukocytosis, i.e. an increase in white blood cells, is often noticed.
These symptoms tell me that I am sick
In order to have an increased risk of the disease at all, one must have received long-term antibiotic therapy beforehand. This is often the case with ENT patients, people with pneumonia, and those with artificial joint inflammation. If bloody diarrhea and cramp-like abdominal pain persist after a few weeks of antibiotic therapy, a doctor should be consulted.
A high fever is also typical during the illness. The diarrhea has a characteristic foul odor and high frequency. Due to the high water loss, those affected feel limp and the skin can get wrinkled. In severe cases, consciousness can also be impaired.
The course of a severe infection can be very rapid, so that there are only a few hours between a slight discomfort and intensive care.
Toxin A
For Clostridium difficile to be able to trigger a disease at all, the bacterium must produce toxins. Strains that cannot do this are considered non-pathogenic, i.e. harmless. Not all bacterial strains produce the same toxins and therefore there are some cases where Toxin A is not produced.
Toxin A, an enterotoxin, is considered the less important toxin for clostridial-induced diarrhea. Enterotoxins are proteins that are released by the bacteria and are toxic to the intestinal cells. Toxin A can make holes in the cell wall and thus either kill the intestinal cells directly or provide a gateway for other toxins.
Toxin A also has a chemotactic effect on certain immune cells, the so-called neutrophils. This means that the poison affects the movement of immune cells. Toxin A works by changing the cytoskeleton of the cells and can thus also change their shape.
Toxin A does not normally occur alone, but is accompanied by toxin B. The host's likelihood of illness increases if the immune system does not respond adequately to toxin A. Most adults have antibodies against toxin A, as contact with the pathogen often took place in infancy.
Toxin B
Toxin B is the second toxin produced by Clostridium difficile. It is a cytotoxin. In some people, only toxin B is present, which is why it is assumed that toxin B is the more important factor in Clostridium difficile disease.
Toxin B also attacks the cytoskeleton, which gives the intestinal cells their shape. The laboratory tests for clostridial infection are particularly specialized for toxin B, as this is more common than toxin A.
incubation period
Since Clostridium difficile can also be detected in healthy people and only becomes active after certain environmental influences have occurred, no maximum incubation time can be specified.
Some people carry Clostridium difficile in their intestines for their entire life without ever falling ill. However, after the initial infection, the bacterium must first multiply sufficiently to trigger an illness.
Treatment / therapy
The first step in treatment for clostridial infection should be to try to remove the trigger. This means that all antibiotics should be stopped whenever possible. Furthermore, due to the diarrhea, care must be taken to ensure an adequate supply of fluids.
All drugs that inhibit bowel movement should be avoided. These include the opioids and the over-the-counter anti-diarrheal medicine Imodium. These can hide the condition and make it worse.
The first choice for a first infection is metronidazole, an antibiotic that works well against clostridia. Vancomycin should be used directly in pregnant women and children.
In severe infections, vancomycin is also used directly or coupled with metronidazole. Vancomycin can also be given directly into the intestine in severe cases. In the case of recurring infections, a stool transplant can be considered, as a healthy microbiome can displace the clostridia.
Surgical therapy may be necessary for complications such as the toxic megacolon, but this is associated with high complication rates.
Read more on the topic: Stool transplant
Duration / forecast
Mild to moderate clostridial-induced diarrhea can last a few days to weeks.
However, a severe course with complications can mean weeks to months in hospital and intensive care units.
The disease is approximately seven percent fatal, which can be attributed to the currently widespread more dangerous strains. The likelihood of a fatal outcome increases with age. After a previous infection, new illnesses are relatively common.
Course of disease
The course of a clostridial infection is very rapid. Those affected first notice abdominal pain and slimy, foul-smelling diarrhea, which start very suddenly. Severe courses can develop within a few hours to days.
Intestinal obstruction occurs and in some cases serious complications, such as the toxic megacolon and blood poisoning. The healing usually takes longer than the development, as the normal intestinal flora must first be rebuilt.
Read: Toxic megacolon
How contagious is the disease?
Clostridia are among the spore-forming bacteria. These spores are very environmentally resistant and can linger on surfaces in hospitals for long periods of time and infect people.
It is transmitted fecal-orally, which means that the spores from the intestine reach the mouth via the hands. The risk of infection by medical staff is therefore very high, especially in hospitals and nursing homes. In some intensive care units, spores have even been detected in the air.





.jpg)