Caries
Synonyms in a broader sense
Carie, tooth rot
English: Decay
introduction
Tooth decay is the most common disease in the world.
It is particularly common in countries where sugar cane is grown, such as South America, Cuba or Mauritius, because the population likes to chew sugar cane because of its sweetness.

What is tooth decay?

The tooth decay, also called tooth decay, is a chemically parasitic Process. Organic acids and bacteria produced by bacteria work together directly and lead to the destruction of the hard tooth substance. The tooth decay destroys the enamel and the dentin, called dentin (see also Anatomy tooth), progressively without the possibility of the body's own regeneration, as there is no blood supply in this area. The bacteria responsible for the formation of acids are those that absorb sugar and generate acid through their metabolism. The main germ is Streptococcus mutanswhich, however, is not present in the oral cavity from birth, but is only transmitted through intimate contact with the mother, for example through kissing. So tooth decay is an infectious disease.
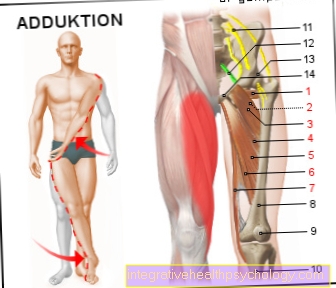
Figure tooth decay

Tooth decay
chemical parasitic process
- Tooth enamel -
Enamelum - Dentin (= dentine) -
Dentinum - Tooth pulp in the tooth cavity -
Pulp dentis in Cavitas dentis - Gums -
Gingiva - Cement -
Cementum - Alveolar bone
(tooth-bearing part
the jawbone) -
Pars alveolaris
(Alveolar process) - Nerve fibers and blood vessels
Stage of the disease:
Descaling process (A + B + C)
Minerals dissolve from the
Tooth enamel -
(no toothache)
Progressive tooth decay (D)
Caries reaches the dentin -
(occasional throbbing pain)
Very deep caries defects (E + F)
that reach the pulp -
(severe, stabbing toothache)
the increasing destruction
of nerve fibers can become a
Cause blood poisoning
You can find an overview of all Dr-Gumpert images at: medical illustrations
How does tooth decay develop?

By consuming food (see also nutrition), which in most cases also contain sugar, albeit often hidden, the bacteria are constantly stimulated to produce acid. However, caries will not always develop straight away, as the saliva with its calcium content is able to repair the first beginnings of decalcification. Only when the acid attack is stronger than that Remineralization is, it comes to the formation of caries.
The enamel is first decalcified, which is noticeable by a white discoloration. At this stage, when the top layer of enamel is still intact, fluoride can still stop the process. However, if the top layer has already been broken through, the progress of the destruction can no longer be stopped.
More about the stages of caries development at: How does tooth decay develop?
The carious dissolution of the tooth enamel continues and reaches the dentine, i.e. the dentin, which is softer than the enamel. This process takes some time. Since the dentin is not as resistant as the tooth enamel, the caries in the dentin proceeds faster but inexorably and undermines the enamel. This is reflected in a dark discoloration.
The undermined enamel becomes so thin that it collapses. Now, at the latest, the extent of the destruction can be seen. X-rays can confirm the findings. As Caries profunda is called the deeper caries. Fine canals run through the dentin in which there are nerve fibers that extend into the pulp. That is the reason why pain occurs now, especially when it comes to sweet things, as the bacteria produce acid, but also when it comes to temperature stimuli.
If nothing is done, the destruction of the tooth continues and reaches the pulp, the tooth pulp with its blood and nerve supply. After severe pain, the pulp perishes and the tooth can ultimately be lost.
In younger people, tooth decay is the most common reason for the loss of teeth, in the elderly it is due to diseases of the gums.
The different stages of caries formation
Caries can be divided into four different stages.
- The first stage describes the initial lesion or the Caries initial. In this development phase, only the enamel has been decalcified or demineralized and no break in the surface can be felt. This stage can therefore still be reversed and controlled through targeted fluoridation. All other stages are irreversible and must be treated with measures such as filling therapy.
- In the second phase, there is a break in enamel, which only affects the top layer of the hard tooth substance.
- If the caries spreads further, it reaches the dentin and is in the third caries stage. This stage is called an enamel or dentin lesion Caries profunda designated. As soon as the dentin has been reached by the caries, it progresses much faster because the dentin is less hard and can be more easily penetrated.
- The last stage is when the pulp is reached. The caries has now completely penetrated through the enamel and dentin and affects the pulp. The nerve and blood vessels are metabolized by the bacteria and thereby die.
At this stage, filling therapy alone cannot save the tooth. The tooth must be provided with a root canal treatment beforehand in order to completely rid the pulp of bacteria and to close the root canals with a root filling. The tooth can then be restored with filling therapy and, at best, a crown to restore its complete stability.
How are the holes caused by tooth decay?
The bacteria metabolize low molecular weight sugars into acids, which are a waste product of the microorganisms and damage the tooth substance. The acids demineralise the enamel and break down the hard tooth substance, causing a break in the surface. This opening hole is the entry gate for further bacteria and their acids, which expand further and further into the depths.
As a result, the typical means of caries diagnosis for the dentist is careful scanning of the tooth surfaces with the probe. In the case of caries, a break in the surface can be felt with the probe and the probe remains stuck there. Due to the tendency to spread into the depths, the typical caries holes known in the vernacular arise.
Caries bacteria
Well over three hundred different types of bacteria exist in the healthy oral flora of the oral cavity, of which only two types belong to the caries bacteria. These bacteria can metabolize the sugar in food, which is absorbed as a substrate, into acids (especially lactic acid) and damage the tooth permanently. These bacteria include primarily Streptococcus mutans and lactobacilli.
The main caries bacterium is Streptococcus mutans, which settles in the plaque. Streptococcus mutans forms glucan molecules from the sucrose ingested with food, which it can use to adhere to smooth surfaces such as tooth enamel.
Caries bacteria can be transmitted from person to person through saliva. The bacteria can be detected by microbial saliva tests. Both the type and number of bacteria can be determined. A high number of Streptococcus mutans and lactobacilli speak for a high risk of caries, a low number for a low one.
But only if the bacteria can utilize leftover food will caries develop, which means that an infection with Streptococcus mutans will not turn into caries with excellent oral hygiene.
Recognize tooth decay
The problem with tooth decay is usually that it is hardly noticeable at first. Affected patients usually only see a dentist if they already have a toothache. In these cases, however, the caries is very advanced and requires more extensive therapy. For this reason, it is advisable to go to a so-called preventive check-up twice a year.
Read more at: How do you recognize tooth decay?
The dental check-up is a health insurance service and all costs are borne in full by both private and statutory insurance. In addition, bonus points can be collected with regular participation in a dental preventive program. These bonus points can significantly reduce the patient's own share of those who have to be fitted with a dental prosthesis (for example a crown or bridge).
In addition, it is quite easy for the dentist to recognize any tooth decay at an early stage and treat it in a simple manner. If tooth decay is suspected, the check-up is usually followed by an X-ray examination. The X-ray image helps to recognize how deep the carious defect has already penetrated the tooth substance. In addition, it is advisable to carry out an X-ray check at regular intervals even with existing fillings. This helps to identify at an early stage whether new caries has formed under the filling material or whether there are inflammatory processes in the area of the tooth root tip.
Furthermore, so-called caries detectors are often used in dental practice. These are substances that can be applied to the tooth and change color in the event of tooth decay. People who want to check the condition of their teeth at regular intervals can look out for the following characteristics of tooth decay. In order to detect tooth decay at an early stage, it should be ensured that the teeth:
-
show whitish discoloration
-
show brown spots
-
have sticky spots
How can you recognize tooth decay yourself?
For the layperson, tooth decay is usually only recognizable in the later stages, when the lesion already affects a large part of the tooth. Tooth decay can be of different colors. An initial demineralization of the tooth enamel can be seen as a white discoloration, which corresponds to a decalcification. This demineralization is the preliminary stage of caries in which the surface is still intact and the development of caries can still be stopped by targeted fluoridation measures.
If there is an initial tooth decay with surface collapse, it can take on a yellowish to brownish color. It is usually very small and barely visible to the person concerned in the mirror. Since this carious lesion grows deeper, the hole often does not become larger, but rather a point-like, discolored opening port that only spreads deeper like a balloon. Patients often notice black, punctiform discoloration, especially in hard-to-clean areas such as fissures. These so-called “black spots” are usually inactive caries areas that show no tendency to spread, provided they are regularly and specifically fluoridated. These black spots have around 80% of the population.
The dentist does not notice the inactive caries getting caught when touching the probe, the black spots are hard to probe. Nonetheless, these areas should be checked regularly so that the inactive carious form does not change into an active form and spread further down.
Furthermore, caries lesions in the interdental space are invisible both to the person concerned and to the dentist through sole inspection. In this case, the dentist can only detect the caries through X-ray diagnostics. In general, it is very difficult for those affected to recognize tooth decay, as the disease can take on so many different forms and is difficult to recognize without special diagnostics. Therefore, a six-monthly check at the dentist should not be dispensed with.
Learn more at: How can you recognize tooth decay?
Occur
The frequency of tooth decay can vary from person to person. There are people who rarely or never develop tooth decay and others who have more frequent caries defects. Why this is so is not entirely clear; it is assumed that genetic influences are responsible for these differences.
Tooth decay is particularly common when the flow of saliva is too low. This is the case, for example, after x-ray irradiation in the head area.
Certain areas of the teeth are particularly prone to the onset of carious events. These are the spaces between the teeth, the tooth surfaces and the tooth necks. This is where dental plaque can collect particularly well and is more difficult to remove. Detecting caries can be particularly difficult in the interdental spaces, as the first signs can be hidden by the gums. Misaligned teeth (dentition anomalies) also promote the occurrence of caries.
But any area that is difficult to access for daily oral care also has a higher risk of tooth decay. The molars and wisdom teeth are often affected by tooth decay because of their location.
Read more about this under: Caries on the wisdom tooth
Caries between the teeth
The interdental space represents a dirt niche, which means that caries accumulates here, as the area is difficult to access for the patient. The toothbrush does not reach the narrow spaces between the teeth with its bristles and therefore these spaces have to be cleaned with additional aids such as dental floss or interdental brushes.
Since this cleaning method is one of the least popular and is not used by a large part of the population, food residues can remain in this space for a longer period of time. The microorganisms then have a free path to use this food residue as a substrate and to multiply - as a degradation product, caries results from the acid production.
In most cases, both adjacent teeth are affected by the caries. Furthermore, this caries can usually spread unnoticed and unhindered, since it is clinically invisible to the dentist. The caries in the interdental space can only be detected by x-ray diagnostics and without this remains hidden. It is therefore important to remove any remaining food residues in the interdental spaces as early as possible in order to give the bacteria no chance to form caries in these crevices.
Regular fluoridation in the interdental spaces can also provide lasting protection against the development of caries.
Tooth decay of milk teeth
Milk teeth are much more porous than permanent teeth and are therefore less well protected against caries. This is because the mineral content of the enamel of the milk teeth is much lower, which is why a caries lesion spreads at a faster rate. Furthermore, the relationships between the layer thicknesses of the milk teeth are different. The enamel layer is much thinner, the dentin layer is thicker than in a permanent tooth. The tooth pulp, the pulp, is also much larger and can therefore be reached more quickly and easily than with a permanent tooth.
Therefore, there is also a greater risk that the dentist will encounter the pulp while removing caries than with permanent teeth. In this case, a root canal treatment of the milk tooth is necessary in order to guarantee the placeholder function of the tooth for as long as possible. Another problem is poor oral hygiene in many children. Due to restricted motor and mental abilities (especially in small children) they brush their teeth much worse and plaque can attack the teeth more easily.
Furthermore, a poor diet with lots of sweetened drinks and foods increases the risk of tooth decay.
Caries under a filling
If a tooth is affected by caries, it is treated with a filling therapy. Filling materials are variable. After this filling therapy, the destroyed carious tissue is removed and replaced with filling materials.
It is quite possible that caries will reappear under the filling at the edges of the tooth structure. This tooth decay is called secondary caries. This secondary caries occurs much more often under plastic fillings than with amalgam fillings. This is because amalgam has a bactericidal effect that protects the filling edges from tooth decay. Plastic does not have any bactericidal effect, which increases the frequency of secondary caries.
It is particularly important to thoroughly clean teeth that have been filled with a filling, especially the spaces between the teeth. If bacteria can adhere to the edge of the filling, it is often easy for them to reach the intact tooth beneath the filling and lead to secondary caries. Progressive secondary caries can be a reason why a filling breaks out or is lost. The caries softens the hard tooth substance under the filling and thus loosens the bond between the filling and enamel or dentine, so that the filling can loosen.
Secondary caries can be caused by poor oral hygiene, but incomplete removal of caries can leave behind bacteria that can cause caries to develop under the filling. A very old plastic filling may also have become leaky, as the edges of the filling discolour after a certain time and are not as durable as amalgam, for example. Therefore, the edges of plastic fillings in particular should be checked regularly and replaced after a few years.
Tooth decay under the crown
A crown protects the tooth from further loss of hard tooth substance, especially if the tooth is already weakened by carious lesions. As with secondary caries under a filling, caries can also form under a crown. The reasons for the development of secondary caries are similar. After a while, the cement that holds a crown in place may wash out and open a crack.
If this gap is not noticed and accordingly carefully cleaned, bacteria can get into this groove under the crown and weaken the healthy tooth structure through caries. If there is also poor oral hygiene, the bacteria can use the leftover food as a substrate and metabolize it.
Since the enamel layer was almost completely removed by the preparation for the crown, the tooth is hardly protected if the microorganisms get under the crown. The caries then usually progresses quickly and can quickly infect the pulp and nerves.
Furthermore, a treatment error or a mistake by the dental technician can also be the reason for a leaky crown. If the marginal seal of the crown is only slightly too large, it represents an entry portal for caries which will promptly cause secondary caries. The tricky thing about it is that the caries remains radiologically invisible, as the crown completely absorbs the X-rays and does not guarantee any insight into the interior. Therefore, even the dentist usually notices very late that secondary caries has formed under the crown, for example on a leaky edge.
The cervical caries

Dental neck caries is not located on the occlusal surface like most caries, but, as the name suggests, in the area of the tooth neck. This can, as physiologically intended, be closely covered by the gums, or be exposed due to external influences, such as excessive brushing of the teeth or a gum disease. If it is exposed, bacteria can easily get to it.
The tooth neck represents the transition from the tooth crown to the tooth root. The tooth crown is covered with tooth enamel and merges into tooth cement at the tooth neck, which covers the dentin in the area of the root. The enamel is very hard and the real protection against tooth decay. However, this is no longer present in the area of the tooth neck, so that the dentin can be attacked by bacteria without hindrance. It is very easy for them in this area, as they attach directly to the softer dentin and can reach the tooth pulp relatively quickly, from there it is only a short jump to the root canal.
The main cause of caries in the tooth neck area is exposed tooth necks. The causes of exposed tooth necks are different. The main reason is usually periodontitis.
But nicotine consumption can also contribute to this.
Exposed tooth necks can also catch people who regularly brush their teeth, but exert too much pressure with the toothbrush, which may be too hard, and also use toothpaste with strong abrasive particles. This puts a lot of stress on the gums, causing the small fibers of tissue to travel and the gums to retreat.
The way for bacteria on the tooth neck is clear.
The best precaution against dental caries is not to give the bacteria any possibility of causing tooth decay.
Since the main cause is exposed tooth necks, one should prevent periodontal disease or gingivitis.
The most important thing is good and adequate oral hygiene. Brush your teeth at least twice a day with a toothpaste containing fluoride, with a toothbrush that is not too hard and with little contact pressure. Perform the movements in a circular motion away from the gums towards the crown of the tooth at an angle of 45 °.
Electric toothbrushes remove plaque even more reliably and easily. Tongue scrapers, mouthwashes and dental floss, for the hard-to-reach spaces between the teeth, are to be used in addition. It is also very important to keep the check-up appointments, at least twice a year, at the dentist.
Professional teeth cleaning can also be carried out during such a visit.
Read a lot more information on this topic at: Cervical caries
therapy
Effective caries therapy can only be guaranteed if the treating dentist makes a correct assessment of the depth of caries and the condition of the affected tooth. Various diagnostic options are available to the dentist for this purpose. In some cases special solutions, so-called caries detectors, can help to show carious defects on the tooth. These solutions stain the defect after they are applied to the dry tooth.
In addition, a suitable imaging procedure can be carried out before the start of caries therapy. In dentistry, two different procedures are usually used for this. If several teeth in different quadrants show carious areas, an X-ray overview (orthopantomogram; OPG) can be made. If there is only one tooth caries, a so-called tooth film should be recorded. This enables an exact assessment of the caries depth. Since the patient is always exposed to radiation when taking X-rays, imaging procedures should only be carried out in special cases. The treatment of small carious defects can usually be carried out without any problems.
As soon as a caries has been identified as such and the extent of the defect has been determined, the actual treatment can begin. The therapy in the presence of a caries depends mainly on the exact localization and the respective caries stage. In this context, a distinction must be made between different types of caries.
The so-called initial caries is considered a preliminary stage of real caries. These are decalcification processes in the area of the tooth enamel, which show up as small white spots on the tooth surface. This form of caries is usually treated by applying a substance containing fluoride. In this way, the attacked enamel can be remineralized and hardened. In addition, toothpastes containing fluoride can help protect the affected tooth from further damage.
When using toothpaste containing fluoride, however, it is essential to follow the instructions of the treating dentist. An overdose can lead to unsightly fluoride deposits on the tooth surface within a very short time. In the case of caries that is not only limited to the tooth enamel but also affects the deeper dentin, the
Rule of a much more extensive therapy. Fluoridation of the tooth surface can no longer stop the spread of carious defects in the presence of such dentine caries. When treating this form of caries, the treating dentist must remove the carious tooth substance along with a minimal amount of healthy tooth. This is the only way to prevent possible new caries formation under the filling material (so-called secondary caries). The tooth must then be completely drained and filled with a filling material. The choice of the most suitable filling material depends on both the condition of the tooth and the patient's wishes.
When treating caries, a distinction is made between rigid and plastic filling materials. Rigid filling materials are usually only used for more extensive carious defects. They have to be made outside of the oral cavity in a dental laboratory and then inserted into the tooth. For this reason, the rigid filling materials are significantly more expensive than the plastic ones. In terms of stability, however, the advantage is clearly on the part of the rigid filling materials. The group of plastic filling materials mainly includes composites (plastics) and amalgam. After preparation and drying of the tooth, these substances can be introduced directly into the cavity, shaped and cured there. In contrast to the rigid materials, they are particularly suitable for treating small caries.
In the meantime, plastics are mainly used in the treatment of caries. The reason for this is the fact that amalgam fillings are said to have health-endangering properties. A dental filling made of amalgam seems to be much more durable than a plastic filling. The treatment of tooth decay is basically carried out by both statutory and private insurance companies. However, both the production of a plastic filling and the therapy with a rigid filling material require an additional payment from the patient. The only exceptions to this are anterior fillings and fillings in patients who are not allowed to be supplied with amalgam (for example, in the case of intolerance, allergies or kidney dysfunction). In these cases, at least the costs for a plastic filling are fully borne by the health insurance companies. Patients with a so-called caries profunda (deep caries), in which more than 2/3 of the dentin are affected, require much more extensive therapy.
In the case of affected patients, in addition to placing the filling, it is also important to protect the tooth nerve (pulp). For this reason, the usual tooth filling must always be preceded by a so-called underfilling. A drug containing calcium hydroxide, which is supposed to stimulate the formation of new dentin, is introduced into the depth of the cavity. A so-called penetrating caries (caries penetrans), on the other hand, already extends through the dentine into the pulp.
If inflammatory processes develop in the affected tooth, the pulp and the nerve fibers in it must be removed. With this extensive caries therapy, the roots of the tooth are cut with small hand drills (see also: Toothache after drilling) and then thoroughly disinfected (Root canal preparation). In addition, in most cases an antibacterial drug has to be introduced into the tooth and left there for a few days. This form of caries therapy can then be completed by filling the root canals (root canal filling). Depending on the severity of the inflammatory processes, the prognosis can vary significantly. It can be assumed that the large number of treated teeth will require further therapy after a while. If the patient experiences pain again after the end of the root canal treatment, a so-called root tip resection usually has to be performed. If this attempt at therapy remains unsuccessful, the affected tooth must be removed from the jaw.
Read more on the topic: Remove tooth decay and treat tooth decay
Can you cure tooth decay?
No disease is as widespread as caries or tooth decay in the world.Almost everyone in the population has or has already had a carious lesion that had to be treated with painful filling therapy. But can tooth decay also be cured differently?
If caries has not yet broken through and damaged the surface in the initial stage, the initial demineralization can be reversed by fluoridation. In this case, no filling therapy is necessary. As soon as there is damage to the surface (i.e. a hole) caused by caries, fluoridation is no longer sufficient and the tissue destroyed by caries must be removed mechanically.
With innovative lasers such as the E-YAG laser, many want to avoid the unpopular drill, which is not possible in particularly deep cases, since the laser cannot remove all of the caries here. Therefore, in the majority of cases, only conventional restorative therapy brings the desired success.
Can you laser caries?
Laser caries is a new method of targeted removal of caries. The so-called is used Erbium Yag laser, which emits light of a wavelength that is absorbed by the moisture of the tooth. The water expands in such a way that micro-explosions occur, which remove the soft caries tissue through the generation of energy.
During treatment, the patient wears hearing protection because the application generates relatively loud impacts.
However, the E-Yag lasers cannot replace the drill nowadays because they do not work efficiently enough for deep caries. The cost of such a treatment is around fifty to two hundred and fifty euros per carious tooth. In addition, there is no scientific evidence whatsoever for caries removal with laser, which is why the laser has not yet been able to replace the mechanical drill.
Home remedies for tooth decay
In general, home remedies can relieve the pain symptoms of tooth decay, but they cannot stop or even reverse tooth decay.
Chewing on clove and turmeric has proven itself to alleviate the symptoms. Clove extract has been a proven active ingredient in dentistry for thousands of years, and its calming effect is known.
In addition, normal household salt is said to curb caries activity, which, however, is highly doubtful due to the lack of scientific evidence.
If there is irreversible damage to the hard tooth substance due to caries (i.e. a deep hole that extends into the dentin), no home remedy can replace the treatment with filling therapy. In general, the use of remedies at home should be discussed with the attending dentist in order not to impair the therapeutic measures against tooth decay.
Is tooth decay contagious?
While it is common knowledge that diseases caused by viral or bacterial pathogens are contagious. However, most people are not aware that this also applies to tooth decay. Tooth decay is one Dental disease, by bacterial pathogens is caused. According to the World Health Organization (WHO for short), tooth decay is actually the most common infectious disease at all. It is believed that around 95 percent of the world's population is affected. All humans are initially born without the bacteria that cause caries. However, since this disease is contagious, the bacterial pathogens must first get into the oral cavity. The relevant pathogens are usually transmitted in early childhood. Especially the sharing of cutlery
or cleaning a pacifier with the mother's saliva is one of the most common transmission routes. After the transfer, the settle caries-causing bacteria within the Oral cavity of the child, multiply and persist there for years. It can be assumed that there is a direct relationship between the rate of caries and age at the time of infection. The earlier the infectious bacteria are transmitted, the higher the rate later caries rate be. Studies have shown that of the children who became infected early in life, approximately 89 percent developed tooth decay before they were five. Caries is therefore a widespread infectious disease that is highly contagious.
Symptoms
The symptoms of tooth decay cannot be clearly assigned to a pattern, but rather depend on the stage due to their long duration of action.
At the beginning, the patient doesn't even know that he is suffering from it, because pain does not occur at first. Food intake can be followed up in the usual way, without noticing anything with very cold or hot drinks. On the other hand, it is visible, namely in the form of small white dots. If these are discovered by chance, for example during the regular check-ups by a dentist, there is a very good chance of having them treated without further effort and in a very gentle way so that the next stage can be prevented.
Over time, these whitish discolorations become more and more visible and the patient also feels the first symptoms. Pain occurs periodically, so it disappears for a period of time, but it also returns. The phases of non-occurrence become less frequent until the pain becomes permanent.
Eating and drinking turns out to be more unpleasant from time to time. Especially hot or cold drinks, sweet and sticky foods or acidic fruit drive pain to the face when consumed and there is no longer any talk of enjoyment. You grasp the spot from the outside with your hand and are happy when nothing touches this spot anymore. The tooth decay can spread to the surrounding tissue, making the pain even worse.
Another symptom is a foul smell from your mouth.
Tooth decay pain
The tricky thing about the development of caries is that pain only occurs at a very advanced stage. Before that, the tooth is almost asymptomatic, which means that those affected do not even notice the carious lesion.
The first phase, in which the caries is still reversible, is not even noticed by the patient and is more likely to be detected by chance at the dental check-up. Usually pain is only felt when the caries reaches the dentin through the enamel. There are small channels in the dentin that are connected to the pulp through which the bacteria can quickly reach the pulp. The nerves within the pulp react to the stimulus created by the bacteria and the patient feels pain.
These pains are exacerbated for a short time by particularly sugary foods; particularly cold drinks and foods can also lead to the symptoms. The pain has a pulling, stabbing character, but only for a short time and on special occasions such as eating.
Can you see tooth decay in the X-ray?
X-rays are a diagnostic tool for dentists to identify tooth decay. Especially in the places that are not visible from the outside, such as B. on the tooth surfaces between the teeth, the dentist can detect caries with the help of bitewing recordings.
Caries can be seen on the X-ray as a dark spot in the tooth crown or at the root that stands out from the rest of the tooth. However, an initially developing caries can hardly be recognized in an X-ray image; this can only be recognized in radiation diagnostics when the enamel surface has collapsed.
Therefore, regular x-rays based on the general examination every two years make sense in order to detect the development of caries at an early stage and to treat it in a targeted manner, because even the dentist cannot always optimally examine and assess all tooth surfaces.
prophylaxis
The bacteria responsible for the development of caries accumulate in the plaque that forms between the tooth and the gumline. It is therefore important for prophylaxis to remove this plaque with a toothbrush, toothpaste and dental floss. Because the saying goes: "A clean tooth does not get sick."
However, since fluorides strengthen the resistance of the enamel to acid attacks, toothpastes or rinsing solutions containing fluoride should always be used. Fluorides also increase the remineralizing effect of saliva.
Another way would be to avoid sugar altogether, but this is certainly not possible either. One promising measure is the use of xylitol instead of sugar, which is particularly common in Scandinavia. Xylitol can from Streptococcus mutans are not ingested and processed, and this ultimately leads to "starvation" of this germ, which is responsible for caries. But xylitol is expensive and therefore not to be used in all foods. At present it is mainly a component of chewing gum.
For adolescents whose posterior teeth have not yet been affected by caries, sealing the particularly endangered tooth surfaces is recommended. The dimples are filled with plastic and thus protected against acid attacks. This prophylactic measure has proven itself very well and under the name Fissure sealing known.
What is a caries detector?
A caries detector is a solution that the dentist uses to check whether the existing carious lesion has been completely removed and the edges of the cavity are free of caries. The detector is a liquid made up of a solvent and a dye. The solvent can penetrate dead and bacteria-infected dentin and the dye visibly discolors these areas. The caries detector cannot penetrate healthy or demineralized tooth structure, so only the carious areas are colored.
The practitioner can now check for himself whether the carious areas have been completely removed and to what extent he still needs to remove caries. As a result, the caries detector can be used to distinguish necrotic tissue from healthy tissue, which can not only serve as a control during treatment, but is also used as a diagnostic aid.
In most cases, the caries detector consists of the solvent propylene glycol and the dye erythrosine.
Summary
Caries is an infectious disease that is widespread worldwide. Organic acids and bacteria are the triggering cause of the destruction of the hard tooth structure. The bacteria in the dental plaque process the sugar into aggressive organic acids. The therapy consists in the total removal of the infected tissue and subsequent filling with suitable materials. Prophylaxis includes the removal of plaque through carefully performed oral hygiene, for which the necessary instruments are available.