Functions of the pancreas
introduction
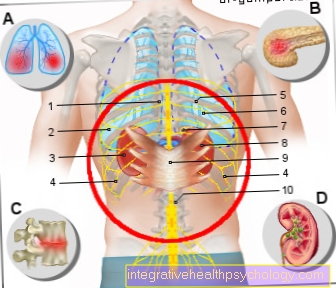
The pancreas is located behind the peritoneum (retroperitoneal) in the upper abdomen. The pancreas has two parts, a so-called exocrine (= emitting to the outside) and an endocrine (= emitting to the inside). The exocrine part of the pancreas, a digestive juice that is released into the duodenum. , The endocrine part produces the hormones insulin and glucagon and releases them into the blood. They are important for regulating blood sugar levels.
Read more about this at:
- Function of the pancreas
- Anatomy and diseases of the pancreas

Function of digestion
The pancreas is built up in lobules. The exocrine part of the pancreas, which forms the main body of the organ, is a purely serous gland, which means that it produces a very liquid secretion. In this proportion, about 1.5 liters of pancreas are formed daily. This is an enzyme-rich, basic digestive juice that is released into the duodenum. Secretion is regulated by digestive processes, with the rate of secretion increasing sharply after ingestion of food. The enzymes for breaking down fat (lipases), protein (proteases) and carbohydrate digestion contained in the pancreas make an important contribution to the digestion of food and ensure that nutrients can be efficiently absorbed from the intestine into the blood.
In addition to the main part of water, the pancreas consists of over 20 different proteins; these are inactive precursors of digestive enzymes (zymogens) and active digestive enzymes. Particularly aggressive proteases such asTrypsin or chymotrypsin are secreted as an inactive precursor to protect the pancreas from self-digestion and are only activated in the duodenum. Other proteases (e.g. α-amylase), lipase and enzymes for nucleic acid digestion are released directly into the pancreas as active enzymes. Another important component of pancreatic juice are protective and regulatory proteins. In addition to digestive enzymes, the pancreas consists of bicarbonate, which neutralizes the acidic stomach contents and leads to a slightly alkaline pH value of 8.1 in the duodenum. The increase in the bicarbonate concentration in the small intestine is important because, on the one hand, it facilitates the micelle formation of fats and, on the other hand, various digestive enzymes are inactive in an acidic environment and only work at basic values.
You can find everything on the topic here: Pancreatic enzymes
Various protective mechanisms prevent the pancreas from being digested and thus destroyed by the pancreatic juice formed: some particularly dangerous proteases are secreted as inactive zymogens and only activated in the duodenum. In addition, a number of protective enzyme inhibitors are released at the same time as the digestive enzymes, and special proteases break down enzymes that have been activated too early.
You might also be interested in: Task of enzymes in the human body
Exocrine Part Hormones
The most important digestive enzymes found in the pancreas can be divided into three large groups. Proteolytic enzymes (protein-splitting enzymes), some of which are secreted as zymogens, carbohydrate-splitting enzymes and lipolytic enzymes (fat-splitting enzymes).
The most important representatives of proteases include trypsin (ogen), chymotrypsin, (pro) elastases and carboxypeptidases. These enzymes break down proteins at different peptide bonds into smaller peptides. α-Amylase is one of the carbohydrate-splitting enzymes and hydrolyzes glycosidic bonds. In order to break down fats contained in food in the duodenum and to be able to digest them, in addition to bile from the liver, various lipases (fat-splitting enzymes) are required. Pancreas contains carboxyl ester lipase, pancreatic lipase and (pro) phospholipase A2, which attack and break down ester bonds in fats.
Tasks in blood sugar regulation
The endocrine parts of the pancreas (islets of Langerhans) lie in small groups of cells between the densely packed exocrine glands. About a million of these islets of Langerhans occur in humans and are particularly common in the tail part of the pancreas. Islets of Langerhans can be seen microscopically as bright areas surrounded by numerous blood vessels (insulo-acinar portal vascular system). There are four types of cells in the endocrine tissue: the centrally located β-cells, which make up 80% of the islets and produce insulin, the glucagon-producing α-cells (20%), somatostatin-producing δ-cells (8%) and PP- Cells that make pancreatic polypeptide (2%).
Insulin and glucagon play a central role in regulating blood sugar levels. Insulin is the only hormone that can lower blood sugar levels. In addition, insulin stimulates fat build-up. An acute increase in blood glucose concentration after consuming food rich in carbohydrates leads to the release of insulin into the blood. The free insulin docks to insulin receptors on cells and thus leads to the uptake of glucose into the cell. The main target tissues are the liver, skeletal muscles and adipose tissue. As a result, the blood sugar level drops and the cells have energy in the form of glucose available.
Glucagon acts as an antagonist to insulin. The main task of glucagon is to increase the blood sugar level by stimulating the formation of new glucose (gluconeogenesis) and the breakdown of glycogen into glucose in the liver.
A meal rich in carbohydrates leads to the release of insulin and at the same time to the inhibition of glucagon, whereas protein-rich foods promote the secretion of both insulin and glucagon. The precise interaction of both hormones is made possible by their antagonistic (opposing) effect and determined by their concentration ratio to each other. This means that blood sugar can be kept constant and large fluctuations (hyperglycaemia or hypoglycaemia) can be avoided.
You can also read about this:
- Pancreatic hormones
- Blood sugar
Endocrine hormones
Insulin is a peptide hormone that is synthesized as a prohormone in the β cells of the endocrine pancreas. Because of its short half-life, insulin is secreted in a pulsatile manner every 10-20 minutes. An acute increase in the glucose concentration in the blood is the strongest stimulus for the secretion of insulin and leads to the rapid removal of the glucose from the blood by the glucose being introduced into the target cells. Other important effects of insulin are, in addition to the increased uptake of glucose in the cells, the uptake of free fatty acids and amino acids. In addition, insulin prevents the breakdown of adipose tissue (lipolysis) and inhibits the secretion of glucagon.
The antagonist of insulin, glucagon, is also formed as a prohormone in the α cells and secreted when required. In addition to protein-rich food, the strongest secretion stimulus is insufficient blood sugar (hypoglycaemia). In addition to increasing the blood glucose concentration, glucagon promotes lipolysis.
δ cells produce somatostatin (SIH, GHIRH), a short peptide hormone that is also secreted by the hypothalamus. Rising blood sugar levels stimulate the release of SIH, which, among other things, inhibits insulin and glucagon secretion. In addition, somatostatin inhibits numerous other hormones and acts as a universal inhibitor.
Pancreatic polypeptide is formed in the PP cells, secreted after protein-rich meals and has an appetite-suppressing and inhibiting effect on the secretion of the exocrine pancreas.