The orbital hernia
Definition - What is an orbital fracture?
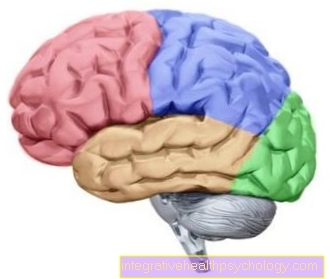
An orbital fracture is also called Orbital fracture designated. An orbital fracture describes a fracture of the bone parts of the skull bones that form the eye socket. The eye socket is made up of parts of several bones. These include: The frontal bone (the frontal bone), the tear bone (the lacrimal bone), the upper jaw (the maxilla), The cheekbone (the os zygomaticum), the ethmoid (the ethmoid bone), the palate at (the palatine bone) and the sphenoid bone (the sphenoid bone).
An orbital rupture is almost always caused by external force. As a rule, these are blunt acts of violence such as one Punch or the shot of one Soccer ball.
The broken bones pinch the eyeball as well as the eye muscles connected to it and the optic nerve. As a result, in addition to bleeding and pain, double vision, restricted mobility of the eyeball and significant visual disturbances are observed. If the nerves are also damaged, this can lead to sensory disturbances and paralysis in the corresponding muscle groups. As the size of the bruise increases, the symptoms also increase as the space in the eye socket continues to decrease.

Detecting an eye socket rupture
What are the symptoms of an orbital rupture?
With a classic orbital hernia there are some typical symptoms. In detail, however, these can vary greatly from patient to patient. Often, increased intraocular pressure occurs, which, if left untreated, can damage the optic nerve of the affected eye. The increased intraocular pressure is caused on the one hand by the squeezing and the possibly pushed together eye socket, on the other hand by bleeding into the surrounding tissue (i.e. a Hematoma), which increases in size and competes with the eyeball for space in the eye socket.
This effect can possibly be intensified if the patient tries to move the eye in a certain direction. The hematoma (bruise) not only spreads within the eye socket, but is also clearly visible to the outside and is often very painful. Due to its characteristic appearance, which is caused by the bone structures and blood vessels involved, it is also called a so-called "Monocle Hematoma". This spreads over the entire upper and lower eyelid and can swell so much that it is no longer possible to open the eyes without using the fingers.
More information can be found here: Bruise in the eye
A wide variety of sensory disorders and muscle paralysis can also occur on the affected half of the face. Which failures occur depends entirely on which nerves and tissue structures were trapped between the bone edges of the orbital fracture. Often the Facial nerve damaged, causing numbness of the upper lip and cheeks.
If the eye socket bones have shifted within the framework of the orbital fracture, it can happen that the eyeball is either "pushed out" of the eye socket, so to speak, or "slides into" it deeper. This symptom is called Exophthalmos (Eye comes further out of the cave) or Enophthalmos (Eye sinks further into the cave). Vision is often impaired as a result, as the eye can no longer be moved fully in all directions.
In addition, it can cause injuries inside the eye, such as bleeding, retinal detachment or tears in the tissue.
Find out more about the topic here: Retinal detachment
If a patient complains of decreased vision, it is a warning sign that structures inside the eye or the optic nerve have been damaged by the orbital hernia. This must then be examined more closely by the ophthalmologist (Fundus examination).
The assessment is sometimes made more difficult by the swelling of the eyelids, which in some cases makes it impossible to see from the outside.
How is an orbital hernia diagnosed?
First of all, the attending ophthalmologist will ask the patient to describe the course of the accident as precisely as possible, as this provides the first important clues for any injuries and possible complications. The patient's condition must also be precisely inquired about in order to be able to localize jokes and classify the symptoms. Typical questions from the ophthalmologist would be, for example "How did the accident unfold?", "Are you in pain?", "Do you have the feeling that your face feels different than before?", "Do you see double vision?"'.
Once these preliminary questions have been resolved, the doctor will begin examining the head and eye socket. He will pay particular attention to the formation of a blue spot (i.e. a Hematoma), sunken or protruding eyeball (also as Enophthalmos respectively Exophthalmos and swelling in and around the eye socket.
A careful palpation of the bone provides an initial indication of how many bones are involved and whether it is a simple or complicated orbital fracture. If the eye socket has completely ruptured and the floor of the eye socket is no longer intact, the orbital rupture is also called a "blow-out fracture". In addition to the symptoms already described, the eyeball can sink into the now deepened eye socket, which is also called a Enophthalmos.
Another important part of the examination is the functional test. This includes testing the eye function itself (the double vision already mentioned), the function of the nerves in and around the eye (Do some places feel different to others? Can all muscles be moved? Are there paralyzes?).
It is also important to watch out for accompanying symptoms such as a runny nose (blood or cerebrospinal fluid could leak if the orbital fracture is severe.
Depending on the extent of the injury, doctors from other specialties may have to be called in to assess the fracture more precisely. After the detailed questioning and examination of the patient, imaging methods are used last. The most informative in this case are: the X-ray image, a computed tomography image (CT for short), and a magnetic resonance image (MRI for short). Here, the course of the fracture edge, the bones and structures involved are assessed and any bone splinters are searched for. It can also be used to assess whether tissue parts are trapped in the hernia.
Treating an orbital fracture
How is an orbital hernia treated?
If the orbital fracture is a simple fracture without bone splinters, trapped structures or complications, surgery does not necessarily have to be performed. On the contrary, according to the current state of knowledge, the operation is even controversial. The risks and the effort involved in such an operation should not be underestimated, and doctors must ask themselves whether they are worth the potential benefits and success. In some cases there is a spontaneous improvement of the orbital hernia within the first four weeks. Therefore, a doctor never decides alone if there is an orbital fracture, but always consults colleagues from other disciplines, such as ophthalmology, ENT, trauma surgery, oral and maxillofacial surgery and radiology.
Surgery should be performed if at least one of the following criteria is met:
- Enophthalmus (a sunken eyeball) of over 2mm
- Double vision
- pinched eye muscles
- if more than 50 percent of the orbital floor is broken
- if a patient complains of severe sensory disturbances or symptoms of paralysis
If a decision is then made on a surgical procedure, it must be determined how the eye socket is to be reconstructed. It can be between plastic and metallic material be chosen to reconnect the bones of the eye socket. Surgery must be done immediately, and in some cases it is advisable to wait a few days and even up to two weeks for the swelling to subside before operating.
If the doctors decide against an operation because there are no complications and it is a simple orbital fracture, the orbital fracture will be treated conservatively. This means that the patient is prescribed decongestant medication, usually cortisone-containing preparations. Antibiotics are given to prevent infection. Pain relievers are prescribed as needed by the patient. Regular check-ups with the attending physician should be carried out in order to assess the healing process and possibly to initiate a change in the therapy if the success does not occur as desired.
When is an operation necessary?
Surgical treatment of an orbital fracture is indicated if it is not a simple fracture of the orbital which will heal spontaneously and promptly even without surgical intervention. If the patient complains of double vision, if the eyeball has sunk more than 2mm into the eye socket, the eye muscles are pinched (i.e. the eye is no longer fully movable in all directions), if more than 50 percent of the floor of the eye socket is broken or if the patient is severely paralyzed and describes sensory disturbances on the affected half of the face, an operation should be performed.
Even if it is a complicated orbital fracture, i.e. if the bones are splintered or other structures in addition to the eye socket are injured, such as the upper jaw, the Zygomatic bone, the Tear ducts or the Sinuses. In some cases it may be advisable not to decide whether or not to have an operation straight away, but to wait a few days (up to two weeks). Over time, the hemorrhage can heal and the swelling can subside, so that the extent of the orbital fracture and the possible complications can be better assessed. Even the operation itself is easier to carry out and more promising in a swollen state.
How is an orbital hernia operated?
If the orbital hernia is to be treated surgically, the procedure takes place in several steps. First of all, the course of the breakline must be assessed and any displacement of the individual parts recognized. In particular, attention should be paid to the very thin walls of the eye socket, as these break very quickly as part of an eye socket injury and can then lead to complications.
In a second step, the trapped tissue is removed from the hernia and returned to its original location. Here the surgeon must pay particular attention to fine structures such as smaller muscles, blood vessels and nerves so that they are not damaged or, in the case of existing damage, can be repaired.
In the next step, smaller fragments of bone are removed from the wound and the larger bone parts are put back together and connected to one another. It is up to the surgeon to decide whether plastic or metal is used. Depending on the extent of the orbital fracture and the accompanying injuries, different numbers and sizes of connecting pieces may be required here. These usually remain on the bones even after the operation, since subsequent removal is associated with considerable effort and risks.
The goal of the intervention is always that Eliminate tissue damage, all Structures as far as possible reconstruct and for one stable eye socket as well as the surrounding bone.
Preventing an orbital rupture
What are the causes of an orbital rupture?
In the majority of cases, a rupture of the eye socket occurs as a result of direct external force. The most dangerous thing is the punctual occurrence of blunt or even pointed force on the eye socket itself, its edge or the surrounding areas. This can be a Punch be a shot with one Soccer or with a smaller one Tennis ball or Golf ball. Also in the context of Car accidents or other accidents in which the head area is injured, an orbital rupture can occur.
Statistically, one third of orbital fractures are caused by traffic accidents and another third by punches. Another fifteen percent result from industrial accidents and the remaining ten percent arise from sports accidents.
The acutely increased pressure in the eye socket, which is caused by the squeezing of the eyeball from the outside, leads to either partial or complete rupture of the eye socket bones. In particular, the bone of the orbital floor is only a few millimeters thick and accordingly prone to breakage.
Read also: Orbital floor fracture
Furthermore, the orbital fractures can be classified according to where the fracture is exactly and which bones were all injured. A rough distinction is made between orbital roof and orbital floor fractures. It is important where the violence hit the head, as different structures are involved. Furthermore, a distinction is made between simple and complex fractions.
- In the case of a simple break, a clear break line runs through the affected bone or bones.
- In the case of a complicated break, the edge is not straight, but there are splintered parts in the break area, which lead to an additional risk to the eye.
More information is available here: Injuries to the eye
Course of an orbital rupture
How long is the healing time after an eye socket rupture?
The healing of an orbital hernia depends to a large extent on its severity and extent, on the accompanying injuries as well as the type and timing of the selected therapy. If it is a simple and complication-free orbital hernia, there is no need to operate and the chances are good that the hernia will occur within the next four weeks healed on its own. However, the symptoms do not suddenly go away; it is a protracted and gradual healing process, which is why patients have to be very patient and careful during this time.
However, if there is a moderate to severe orbital fracture, a surgical procedure is necessary. If this allows the bone parts to be put back together well and little damage has been caused to the surrounding tissue, then the coming Weeks and months a healing will occur.
In a number of cases, little or no consequential damage remains. If major measures were necessary during the operation, such as putting on a splint, it must then be decided whether and when it should be removed. These measures are taken to avoid relapse and to achieve the best possible result for the patient. If structures such as the cranial nerves or the optic nerve have been damaged by the orbital hernia, unfortunately in most cases the damage is irreparable and cannot be repaired. This results in various sequelae with which the person concerned has to learn to live. Mostly these are sensory disturbances or paralysis in the injured half of the face. Visual disturbances caused by damage to the tendon nerves are also no longer curable and sometimes lead to serious impairments.
What complications can occur with a hernia?
An orbital rupture rarely occurs alone. This means that usually not only the eye socket itself is affected, but also the surrounding structures such as nerves, blood vessels etc. have been damaged. Most often there is a combined fracture. Then either in addition to the eye socket that is Zygomatic bone, the nose or the upper jaw Broken. The most common combination is the fracture of the zygomatic bone.
All structures in this area can be damaged by the orbital fracture. These include the lacrimal duct system, cranial nerves running here (such as the Facial nerve) as well as the eye and its nerves, muscles and vessels. The resulting monocle hematoma can also lead to impairments.
The range of injuries that take place inside the eyeball is wide:
- This can damage the cornea
- Foreign bodies can get into the eye
Also read: Foreign bodies in the eye - first aid
- Bleeding can build up in the eye and cause discomfort
- The lens can be damaged or slip out of its holding device
- The iris can become pinched
- The vitreous humor and macula can also bleed in or cracks can occur here
- The retina can peel off
- The optic nerve can be pinched between the break lines or, in the worst case, even tear off
If left untreated, these complaints can lead to impaired vision or even blindness.
What are the risks of eye surgery?
The risks of an orbital hernia operation are largely identical to the usual risks associated with any operation. Bleeding and infection can occur. There may be pain and swelling in the affected area after the operation. The result may not correspond to the desired condition, so that a second intervention is necessary.
There may be complications during the operation, for example from the anesthesia or if the orbital hernia is more severe than initially assumed by the imaging tests. During the operation in the area of the eye socket, the most serious possible complication is damage to the eye nerve, the so-called Optic nerve. This would lead to an impairment of the eyesight or even to its complete loss, which would also be irreparable.
If the eye nerves have already been damaged as a result of the accident, the chances of recovery are difficult to assess in advance of the operation. Occasionally, small fragments of bone have bored into the nerve and thus permanently damaged it. The eye muscles can also be affected in this way.
Another source of risk with this procedure is bleeding-related complications. Either caused by the orbital hernia itself or after the operation, bleeding into the tissue can lead to severe swelling. This is so dangerous because the space in the eye socket is very limited and even moderate swelling can be enough to push aside other structures such as the eyeball or the optic nerve and thus damage them. It is therefore important to give sufficient decongestant medication and to regularly check the healing process.
Further questions about an orbital hernia
Orbital fracture combined with a cheekbone fracture
If the orbital fracture is in combination with a fracture of the zygomatic bone, it is usually a complicated orbital fracture with accompanying injuries, which must be treated surgically. An intervention is necessary, in particular if fragments of bone have become detached from the cheekbone or the bone edges have shifted against each other. The aim of the operation is then to join the cheekbones back together as seamlessly as possible and to remove bone fragments, as these could otherwise lead to complications and inflammation. A large number of different bone plates and screws are available to the surgeon in order to achieve an optimal result. In some cases, the body's own cartilage tissue is removed from another location in order to be reinserted in the area of the cheekbone fracture, which means that the use of foreign material can be avoided.
The operation itself is of course carried out under general anesthesia and is carried out as part of the procedure on the eye socket in order to avoid an additional operation. In the case of very severe fractures of the zygomatic bone with severe damage to the surrounding structures, a tamponade may be inserted.This is a kind of cotton ball that ensures that leaking blood is caught and the tissue structures and bone cavities such as the nose and paranasal sinuses are kept free. Tamponades have to be removed after a certain amount of time, but no further intervention is necessary. Whether the inserted bone plates and screws are removed after the healing process is complete depends on the type of procedure and the material used and is decided by the attending surgeon.
Here you can find more information on the topic: Zygomatic fracture - symptoms, therapy and prognosis
Recommendations from our editorial team
- Eye muscle paralysis
- Eye surgery
- Bruised eyeball
- Pain in the eye
- Eye socket infection