HIV infection
definition
The human immunodeficiency virus (HIV) can be transmitted through the blood, through sexual intercourse, or from mother to child. Acute HIV infection leads to flu-like symptoms. In the further course the immune system is destroyed and opportunistic illnesses can occur. These diseases are infections that have no effect on healthy people.
Nowadays the virus can be well controlled by antiviral therapy. The disease is not curable yet, but the patients can lead a symptom-free life. The prognosis has improved significantly in recent years.
Also read our article: Sexually transmitted diseases (STDs)

The epidemiology
Despite a decline in the rate of newly infected people (Roman Koch Institute, 2011), the issue of HIV and AIDS remains a major issue in the population. In Germany around 70,000 people are currently infected, around two thirds of whom are male. A higher number of unreported cases can be assumed.
Over 30 million people are affected worldwide, and around three million die every year as a result of the infection. Although a large part - around 20 million - is concentrated on the African continent, AIDS remains a numerically important issue in Western Europe. The number of newly infected people reached their peak so far in the early 1980s, when no one knew about the virus and its transmission.
Nevertheless, the rate of sick people in the population is increasing (Prevalence), which is also due to the better and longer survival of the patients. There is a connection between the risk of the disease and belonging to certain groups. The prevalence of the disease among homosexual men is still particularly high. Other risk groups are, for example, users of i.v. Drugs administered, people from countries in which a large proportion of the population is affected, and patients who are dependent on frequent transfusions, for example because of haemophilia. The latter is currently hardly a risk, as blood donations are examined and selected accordingly in this country.
Find out all about the topic here: AIDS
The HI virus
The human immunodeficiency virus (HI virus) is one of the retroviruses - the virus consists of RNA strands and must first transcribe its RNA into DNA during replication. This knowledge is used for therapeutic purposes. Various drugs can inhibit replication and prevent the disease from progressing.
There are two known subtypes of the HI virus. Humans and some monkey species are the reservoirs of the virus. They attack the immune system and weaken the immune system. As a result, opportunistic infections can occur - this type of infection is symptom-free in healthy people, as their immune system can fight the respective pathogens. In immunosuppressed people, however, reactivation of herpes viruses, pneumonia and numerous other diseases can occur.
Find out more about the topic here: The HI virus.
What is HIV 1 and HIV 2?
These are subtypes of the HI virus. Both subtypes can lead to immunodeficiency in the event of an infection and, in advanced stages, trigger AIDS.
The HIV virus 1 triggers the infection in most cases and is spread all over the world. The HI virus 2 is mainly restricted to the African continent and only makes up a small percentage of HIV infections.
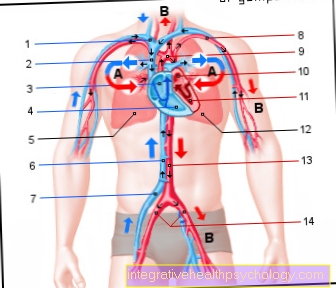
The transfer
The transmission takes place via body fluids of an infected person in direct contact with their own. However, this requires a high concentration of the virus. This applies to blood, semen, vaginal and brain fluids.
This explains the most important transmission routes. HIV is transmitted through both homosexual and heterosexual intercourse. Direct contact of infected material with blood is particularly dangerous. Even minor, barely visible injuries to the skin or mucous membranes are sufficient.
In addition, contaminated blood donations can lead to transmission. Also at risk are drug addicts who can become infected by sharing syringes, for example. The virus can also be passed on from an infected mother to her child during the birth process or subsequent breastfeeding (see below).
Can HIV be transmitted orally?
The HIV virus cannot be transmitted through saliva. It is transmitted through contaminated blood or through sexual intercourse.
The probability that HIV is transmitted through oral sex is very low, as a large amount of secretions containing HIV must be ingested. The oral mucosa is usually very stable so that no infection occurs this way.
Can HIV be transmitted through kissing?
This question can be answered with a resounding no. HIV cannot be transmitted through saliva. The virus is only found in the blood or body fluids, such as semen. As a result, it can only be transmitted through infected blood products or through sexual intercourse. Infected blood products can be transfusions or infected blood collection equipment. Drug users in particular are affected by the use of infected cutlery.
In addition, HIV can be transmitted from mother to child during labor or while breastfeeding. Besides these risk factors, no other transmission routes are known. So kissing is safe.
What are conductors?
A conductor is understood to be a carrier. Various conductors are known to cause HIV infection. This includes infected blood products, such as needles to collect blood. Drug users in particular use these needles and become infected with HIV. For this reason, sterile needles should always be used. If you work a lot with blood in general, it is advisable to wear gloves as blood can also cause other infections.
In addition to infected blood products, humans can also be carriers. The HIV disease can spread in the body and occurs mainly in the blood, sperm and vaginal secretions of humans. For this reason, it is particularly important to adhere to hygienic measures and not to have unprotected sexual intercourse. If you observe these points, the risk can be reduced significantly.
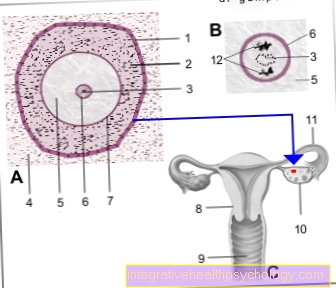
HIV and pregnancy
Although it is a health insurance service, many women do not take HIV tests during pregnancy. However, an existing, possibly not yet symptomatic HIV infection in the mother can be transmitted to newborns.
The overall probability of transmission is around 20%. The virus can be passed on both through the actual birth process and through the subsequent breastfeeding. It is therefore recommended that HIV-positive mothers refrain from breastfeeding. In addition, if the test is positive before or during pregnancy, measures are taken to minimize the risk of infection for the newborn. The birth should be done by caesarean section, as contact of the child's blood with the mother's blood can be avoided. Thanks to the mother cake barrier, the unborn child is usually not infected yet. Therefore, no invasive examinations, such as Amniotic fluid test can be performed.
The mother and the newborn should also receive antiretroviral therapy (see below). Contrary to public opinion, there are also safe options for HIV-positive women and men who want to have children without simultaneously infecting their partner. This includes, for example, artificial insemination of women who tested positive.
How high is the risk of infection?
The risk of an HIV infection is low - the virus cannot be transmitted in everyday life. However, there are a few risk factors that make an infection more likely. This includes unprotected sex with someone who is HIV positive. The risk of infection is increased, especially in homosexual men, as the intestinal mucosa is particularly sensitive and the viruses can more easily penetrate the bloodstream.
Another risk factor is handling infected blood products. Infected blood products can be blood collection needles that drug users use. These people are also at higher risk of becoming infected than the rest of the population. But not only needles, but also blood transfusions are a source of danger. However, the guidelines in Germany are very strict, so that the likelihood of being infected with HIV is extremely low.
Another risk group are people who work in the medical field. Blood must be taken from the patient as part of laboratory tests. It is quite possible that you will prick yourself with a needle after taking blood from a patient (a so-called needle stick injury). Post-exposure prophylaxis can be taken if the patient has a known HIV infection. Post-exposure prophylaxis consists of antiviral therapy that is highly likely to prevent the virus from being transmitted. It should be taken as soon as possible. If possible within the first 24 hours.
In summary, it can be said that the risk of HIV transmission is low. By following certain measures, such as the use of condoms or the use of sterile needles, the risk can be further reduced. However, if an accident does occur and an infection is feared, a doctor should be consulted immediately to take post-exposure prophylaxis.
The symptoms of HIV infection
The HIV disease proceeds in several stages.For this reason, the symptoms differ in the respective stages and make it possible to assess the course of the disease.
Symptoms in the first stage:
This is an acute HIV infection. The symptoms are usually non-specific and resemble flu. Fever, fatigue, skin rashes, abdominal pain, diarrhea and swelling of the lymph nodes may occur. In this phase, virus replication is particularly high and thus the risk of infection.
After one to two weeks, the symptoms subside and a symptom-free latency phase follows. The immune system can fight the virus to some extent.
Second stage symptoms:
The immune system is now weakened and can no longer fight the pathogen efficiently. As a result, virus replication increases again. Fever (> 38.5), weight loss and night sweats can occur. The lymph nodes can swell and a feeling of fatigue can develop. Chronic diarrhea, i.e. diarrhea that lasts for more than a month, can also be the symptom of a progressive HIV infection. In addition to these unspecific symptoms, individual organs can also be affected. This can affect the heart or the nerves (so-called HIV-associated peripheral polyneuropathy). There is also a reduction in white blood cells (so-called neutropenia). This leads to a weak immune system, which increases the risk of infections. In the context of this, a fungal attack can occur in the nasopharynx or in the genital area.
Third stage symptoms:
The third stage is no longer referred to as HIV infection but as AIDS disease. At this stage, the infection has progressed to the point of developing diseases that define AIDS. These are diseases such as Pneumocystis jirovecii pneumonia, fungal infection of the esophagus, cytomegaly infections, cerebral toxoplasmosis or HIV encephalitis. Cancers such as Kaposi's sarcoma or non-Hodgkin lymphoma can also occur.
Find out all about the topic here: The symptoms of HIV
The rash in HIV
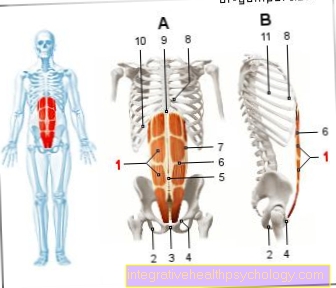
The rash is usually an early stage symptom. It usually occurs on the trunk - i.e. mainly in the chest, stomach area and on the back. The rash manifests itself as reddening and small, blotchy nodules. After the acute infection has subsided, the rash will usually go away.
The rash may reappear later. A very specific rash can occur, especially when the varicella zoster virus reactivates. This virus causes chickenpox in healthy patients and persists in ganglion cells for life. Due to a weakened immune system, this virus can now replicate again and cause shingles (lat. Herpes zoster). This results in a painful rash that is localized only on one side of the body and occurs in a special segment. Shingles occurs in the second stage of HIV infection and is an indication of increasing immunosuppression.
Lymph node swelling in HIV
Lymph node swelling is a non-specific symptom, as the lymph nodes act as a filter station and produce part of the lymphocytes. Lymphocytes belong to the white blood cells and are important for the immune system. Various diseases can trigger lymphadenopathy, i.e. swelling of the lymph nodes - these are usually harmless diseases.
An acute HIV infection also activates the immune system and leads to increased lymphocyte production. Lymphadenopathy results. The lymph nodes can swell again and enlarge again as the disease progresses. In the second stage of HIV infection, generalized swelling of the lymph nodes usually occurs, which does not go away. However, the lymph nodes can only swell locally. The immune defect can cause further infections that only lead to local swelling. An example of this is reactivation of tuberculosis - it usually only affects the lymph nodes in the neck area.
In addition to infections, cancer can also lead to swelling of the lymph nodes and should therefore be clarified by a doctor, especially if the HIV infection has existed for a long time. If the HIV infection has reached the AIDS stage, non-Hodgkin lymphomas (malignant tumor of the lymph node) occur more frequently.
Find out more about the topic here: The lymph node swelling.
The changes on the tongue in HIV
Changes in the tongue can occur as part of an HIV infection. White coatings that can be stripped off are possible. The cause for this is a fungal attack, the candidiasis. The fungus is found on the oral mucosa of everyone. However, it is kept in check by an intact immune system. With an immunodeficiency there is an increased multiplication of the fungus. At an advanced stage, the esophagus can develop fungal infections, which is an AIDS-defining disease.
Oral hairy leukoplakia can also occur on the tongue. This disease is caused by the reactivation of the Epstein-Barr virus. White deposits appear on the tongue that cannot be removed. Most of the time, the changes occur on the side of the tongue.
Read more about the topic here: Candidiasis.
The cough in HIV
Coughing is a very unspecific disease symptom and can be triggered by numerous diseases. A cough can also occur as part of an HIV infection. Usually this cough is very persistent and has no apparent cause.
Furthermore, pneumonia (so-called Pneumocystis jirovecii pneumonia) can develop in the advanced stage of the HIV infection. In this case, additional symptoms such as shortness of breath appear.
Basically, a cough without an identifiable cause and persistence should be clarified by a doctor. Serious illnesses such as HIV infection could be hidden behind it.
Diarrhea in HIV
Diarrhea is a common symptom of HIV infection. This is a relatively unspecific symptom that can also occur with other diseases.
In the context of an acute infection, diarrhea can occur, which disappears after one to two weeks. The immune system can keep the HIV virus in check for a certain period of time, and the acute phase is followed by a latency phase that is asymptomatic. However, there is an increasing immune deficiency, which manifests itself in various diseases or symptoms. In the second stage, there is usually chronic diarrhea that cannot be explained by any other disease.
Kaposi's sarcoma in HIV
Kaposi's sarcoma is an AIDS-defining disease - it only occurs in the advanced stages of an HIV infection.
The cancer is caused by the human herpes virus 8 (HHV-8). Pink-brown spots or lumps appear on the skin, mucous membrane and in the intestines. Most often, the sarcoma is on the skin of the arms and legs. It usually does not trigger any further symptoms - there is no pain or itching. In some cases, Kaposi's sarcoma can also affect lymph nodes and lead to a build-up of fluid (known as lymphedema).
Therapy consists of treating HIV infection. When the immune system improves, Kaposi's sarcoma disappears. If HIV treatment has not yet been initiated, this is recommended. If drug therapy is used, it should be changed.
You can find more information on our main page Kaposi's sarcoma.
Dia diagnostics
The HIV test
HIV testing is carried out in a two-stage scheme - first a search test is carried out, which is confirmed by a confirmation test. The search test is an immunological procedure - a so-called ELISA test. Specific antibodies can bind the antigen in the virus envelope. This binding can be measured enzymatically or by fluorescence.
If the ELISA test is positive, a Western blot test is carried out for confirmation. Performing this test is a bit more complex. Some HIV proteins are transferred to a special membrane. The patient's blood is then added - if antibodies against HIV are present, they bind to the proteins in the membrane. In addition, a Western blot also allows the distinction between HIV 1 and HIV 2.
A positive ELISA and Western blot test make it possible to diagnose HIV infection. If the ELISA test turns out positive, but this cannot be confirmed by a Western blot procedure, a PCR is carried out. A PCR (polymerase chain reaction) duplicates the RNA of the viruses and can detect very precisely whether there is an HIV infection and how high the concentration of the virus is. Since this procedure is very expensive, it is only used for imprecise questions.
Find out all about the topic here: The HIV test.
An HIV test is that safe
To make a diagnosis of HIV infection, more than one HIV test should always be done. Usually an ELISA and a Western blot method are used for this purpose. You can detect an HIV infection with a very high probability.
However, there is a diagnostic loophole - in the first few weeks of the infection, the body has not yet made antibodies against the HIV virus. Without these antibodies, however, the test will be negative. For this reason, if there is a strong suspicion of HIV infection, the test should be repeated after a few weeks. An infection is positive after 12 weeks at the latest, so that a repetition should be aimed for during this period.
If the results are unclear, a PCR can be carried out in addition to the ELISA and Western blot procedure. This is a very precise detection method that can provide a reliable result.
The quick test
The quick test can also be carried out independently at home by laypeople. Like the other methods, the test detects antibodies against HIV. However, it must be taken into account that an HIV infection can only be ruled out 12 weeks after exposure, as the body needs time before it can produce the antibodies.
To do this, blood must first be drawn. This can be taken from the fingertip or the earlobe. Then you put the blood in the rapid test and wait about 15 - 30 minutes. If this test is positive, you should see a doctor who should do another HIV test to confirm the result. If the result is negative, it is recommended to repeat it after a few weeks in order to gain security. If in doubt, it is also advisable to see a doctor.
Read more about the topic here: The HIV rapid test.
The therapy
There is still no cure for an HIV infection. Yet it is not an immediate death sentence. The ever-improving drugs maintain and significantly improve the quality of life. These are summarized under the term antiretroviral therapy, i.e. a treatment that is aimed specifically against the special behavior of this type of virus.
There are now a number of different active ingredients that attack different parts of the life cycle of a virus. For example, the penetration of viruses into the T cell can be suppressed in this way. Usually at least three different active ingredients are combined. One then speaks of the so-called highly active antiretroviral therapy (HAIR). With the help of this form of therapy, a normal life expectancy is now possible if treatment is started in good time.
However, the highly effective drugs cause many side effects. Depending on the active ingredient, metabolic disorders, for example, in the area of the nerves or blood formation can occur. Since the medication must be taken permanently, it is important to weigh the side effects against the effectiveness in order to find an optimal individual therapy. The effectiveness is checked regularly. The number of T cells, but also the amount of viruses in the blood, play a role here.
For more information, see: The therapy of AIDS.
These drugs are used for HIV
An HIV infection should always be treated, otherwise the immune system will be destroyed. There are numerous different drugs available that inhibit virus replication and have a beneficial effect on the course of the disease.
There are five important classes of substances in HIV therapy:
-
Nucleosidic reverse transcriptase inhibitors (e.g. lamivudine, abacavir, emtricitabine)
-
Nucleotide reverse transcriptase inhibitors (e.g. tenefovir)
-
Non-nucleoside reverse transcriptase inhibitors (e.g. efavirenz, nevirapine, etravirine)
-
Protease inhibitors (e.g. darunavir, atazanir, lopinavir)
-
Integrase inhibitors (e.g. raltegravir, elvitegravir, dolutegravir)
In order to achieve optimal therapy success, the different substance classes are combined. Common combination options are the use of 2 nucleosidic or nucleotide reverse transcriptase inhibitors and 1 integrase inhibitor. Another alternative is the combination of 2 nucleoside or nucleotide reverse transcriptase inhibitors and one non-nucleoside reverse transcriptase inhibitor. It is also possible to take 2 nucleosidic or nucleotide reverse transcriptase inhibitors and 1 protease inhibitor.
Some of these preparations are available in fixed combinations so that a patient does not have to take many different tablets and do not lose track of things.
The therapy can be varied individually and can also be changed in the course. Regular intake is important for the patient, as inconsistent intake can lead to the development of resistance. This means that the viruses develop a mechanism and the drugs can no longer work. This can have a very unfavorable effect on the course of a patient's disease. In addition, HIV therapy must be continued for a lifetime. Fortunately, HIV patients have a normal life expectancy with well-controlled treatment.
Which doctor treats HIV?
Since HIV treatment is quite complex, you should consult a doctor who specializes in HIV, who can better assess the course of the disease and who is well acquainted with the therapy options. As a rule, these are doctors who have completed their specialist studies in infectious diseases and who have focused on patients with HIV.
The German Aidshilfe has a directory with a list of specialized HIV doctors - so you can find a practice near you. Alternatively, some clinics have HIV outpatient clinics that you can visit.
These could be signs of HIV infection
The signs of HIV infection are very variable and depend on the stage of the disease. In the initial stage, flu-like symptoms such as fever, sore throat, fatigue and swelling of the lymph nodes can occur. Nausea, diarrhea, or rashes are also possible signs. In this phase the viral load is particularly high - the body actively fights the virus and can keep it under control for the time being. The so-called latency stage follows. In this phase there are hardly any complaints. However, the immune system cannot control the virus forever and over time the virus multiplies and destroys immune cells in our body, causing an immune deficiency. Because of this immune deficiency, various other diseases develop, which express themselves differently.
The second stage can include weight loss, a slightly elevated temperature, and chronic diarrhea. In addition, the oral mucous membrane can have a whitish coating, which indicates a fungal infection (so-called oral thrush). This fungus can also affect the mucous membrane in the genital area and cause genital thrush. In addition, laboratory parameters can be changed during a blood test. The hemoglobin, i.e. the red blood cells and some immune cells, are severely reduced. If these symptom complexes occur, a more detailed investigation should be carried out. Because the earlier an HIV infection is treated, the fewer serious complications there are.
In the third stage, the signs are very variable - the immune system is severely weakened and the AIDS stage is reached. Pneumonia, such as Pneumocystis jirovecii pneumonia, or fungal infection of the esophagus are signs of the latter stage. These diseases even define the AIDS stage. At this stage at the latest, a more detailed diagnosis should be carried out. Drug treatment for HIV should also be initiated. Most of these diseases go away when the immune system is restored.
This article might also interest you: The symptoms of AIDS.
How is the disease progressing?
The course of the disease depends on the time of diagnosis. HIV infection discovered at an early stage has only marginally damaged the immune system. A well-adjusted therapy enables the body to regenerate and strengthen the immune system.
However, if the HIV infection is discovered too late, the immune system can be impaired to such an extent that other opportunistic infections can occur. These infections are diseases that have no effect on healthy people. The immune system can fight these pathogens without any problems. However, the situation is different with HIV-infected people - these opportunistic pathogens can trigger diseases that lead to serious complications. For example, lymphomas (malignant tumors of the lymphatic system) can develop. In addition to HIV treatment, these require additional therapy. Furthermore, it can lead to a wasting syndrome. This describes chronic fatigue and weight loss that cannot be explained by other causes. Memory can also deteriorate as the virus damages the nervous system.In this way, HIV-associated dementia can develop that does not resolve any longer.
An early diagnosis and initiation of therapy thus determine the course of the disease significantly. Patients who were diagnosed with HIV infection at an early stage and who consistently take their medication have a very good prognosis. Their life expectancy is the same as the life expectancy of the population.
HIV and depression - what is the connection?
Depression is a common disease that accompanies HIV infection. About 40% of HIV-infected patients suffer from depression in the course of their illness. The cause of this is the psychological stress caused by the infection. Those affected think too much about their illness and become pessimistic. It can also lead to social isolation as HIV infection is still characterized by many stigmas. The increasing isolation and the burden of HIV infection often lead to the development of depression.
In turn, depression can have a negative impact on HIV disease, as therapy can be neglected. The virus can multiply and sometimes develop resistance to the drugs, making them ineffective. For this reason, depression should not be neglected.
Signs of depression are depressed mood, listlessness and fatigue. In addition, sleep disorders, increased or decreased appetite and concentration disorders can occur. If these symptom complexes are present, one should consult a family doctor or a psychiatrist. You can make a definitive diagnosis and initiate therapy. In addition to drug therapy, psychotherapy can also help overcome fears.
Adequate therapy for depression leads to an improvement in wellbeing and also influences the course of an HIV infection.
Find out more about the topic here: The Depression.
Stand: Is there a cure in prospect?
A cure for HIV has not yet been possible. However, hope has not died out as there was a patient in 2007 who could be cured. In 2019, two more cases of patients who may have been cured were presented at an international AIDS conference. However, one must first observe these patients before one can make a definitive statement about a cure.
The patient who could be cured had blood cancer and required a stem cell transplant. The special thing about this stem cell transplant was (in addition to the appropriate molecular structures of the tissue for the recipient) a mutation of the CCR5 protein. This protein is required by the virus to enter the immune cell. In the event of a mutation, the virus can no longer enter the cell and dies. Scientists are researching this mechanism and trying to use it for new therapeutic approaches. The first scientific studies on this topic have already been published. Perhaps the researchers will be able to cure HIV in the near future.
The legal aspect
After the confirmed diagnosis and the start of therapy, it is unfortunately far from over for those affected. Many moral and even legal problems arise in daily life. For example, you should be careful about who you give this information to. HIV does not have to be reported, so that the attending physician is subject to absolute confidentiality. Only in exceptional cases, for example if the doctor has justified suspicion that the patient is having unprotected sexual intercourse with an uninformed partner, may it be deviated from.
But even relatives and friends who have been taken into trust can be sued for damages if passed on carelessly. However, someone who knows that they have been infected with HIV is obliged to protect their sexual partner from infection with a condom.
The illness may be concealed and even denied during job interviews, as long as the illness does not negatively affect the job. This does not apply to occupational groups with a risk of transmission, such as surgeons and other specialists. However, the HIV infection can also have a restrictive effect on pilots, for example, as it makes entering certain tropical regions difficult and dangerous. Colleagues in the workplace are usually not at risk, as they cannot be infected through saliva. Exceptions are again employees in clinics and laboratories, where sharp objects are used a lot.
AIDS sufferers with severely impaired performance can be classified as severely disabled and receive appropriate benefits.