Inflammation in the bone
introduction
The human bones are made up of one outer compact shell (Compacta) and an inner porous Cancellous bonewhich contains the bone marrow.
During a isolated inflammation of the external Compacta as Osteitis If the bone marrow is involved, one speaks of a Osteomyelitis. In everyday life, the terms mentioned are often used synonymously.
Inflammation in the bone is a serious condition, often with general symptoms like fever and weakness goes hand in hand and mostly one antibiotic treatment makes necessary.
Treatment is often lengthy, with the chances of recovery depending on the pathogen, the spread of the inflammation and any complications.

Symptoms
The symptoms of inflammation in the bone are first of all Cardinal symptoms of any inflammation.
These include in addition to one Redness and swelling also Pain and Functional restrictions, such as decreased mobility in the joint.
The symptoms mentioned can also appear individually, and the order in which they appear is also variable.
It can also lead to systemic symptoms such as Fever and fatigue come. In the blood can increased levels of inflammation how Leukocytes or CRP be detected.
A distinction is made more acute (i.e. more limited in time) from chronic course.
A chronic course is common in patients with impaired immune system (e.g. with immunosuppressive medication or diseases such as diabetes) and multi-resistant germs observed.
The multi-resistant germs are resistant to several groups of antibiotics and often arise and spread in hospitals.
Inflammation in the bone can become a complication Abscesses and fistulas (Connecting corridors). In some cases it can by destroying the bone tissue too Broken bones come.
causes
An inflammation in the bone can arise locally and thus be limited to a section of bone.
This occurs primarily through open bone fractures, which means that the bone has direct contact with the environment and bacteria, so that it can Osteitis or osteomyelitis can occur.
Also through medical measures such as operations on bones, the introduction of foreign material such as screws or plates, or taking samples (biopsy) local inflammation in the bone can occur.
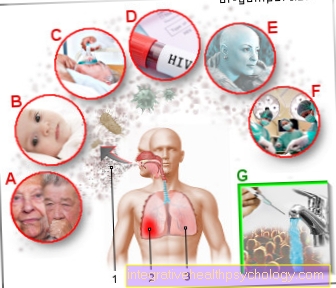
Bacterial pathogens such as streptococci or staphylococci are the most common causes of inflammation in the bones; viruses, parasites and fungi are less common.
In addition to an injury or medical measure, there is also blood poisoning (sepsis) with the spread of the pathogen throughout the body as a cause of bone inflammation. It is not uncommon for several bones to be affected by the inflammation and the course can be severe.
You might also be interested in this topic:
- Inflammation of the bone skin on the coccyx
- This is how long periosteum inflammation lasts
therapy
The therapy depends on the spread of the inflammation and the causative agent.
If several bones and the surrounding soft tissue are affected or if a multi-resistant germ is present, the prognosis deteriorates and more aggressive therapeutic measures are necessary.
If the bone inflammation is bacterial, as is usually the case, the cause can be treated causally with antibiotics. The antibiotics can be administered in tablet form or as an infusion to reach the site of action. Optimally, the antibiotic therapy is targeted after identification of the causative bacterium.
If bone or soft tissue has died off (necrosis), surgical peeling may be necessary to prevent spread and further damage.
During such an operation, the affected area can also be rinsed with antibacterial and sterilizing solutions and a drain can be placed to drain pus.
In addition, sponges soaked in antibiotics can be used, which dissolve themselves and do not have to be removed. In this way, high concentrations of the antibiotic can be achieved on site. As a result, further operations may be necessary to maintain the stability of the bone and thus the mobility of the patient. Read more on the subject at: Osteonecrosis
Read more on the subject below
- Hyperbaric oxygen therapy
- Osteomyelitis therapy
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- Lumedis - orthopedic surgeons
Kaiserstrasse 14
60311 Frankfurt am Main
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see Lumedis - Orthopedists.
diagnosis
The diagnosis of inflammation in the bones can be made clinically, using laboratory methods and using imaging.
Typical clinical symptoms are redness, swelling, and severe pain as well Lymph node swelling in the affected area. Usually there is a functional impairment as well as fever and fatigue. Also fistula- and Abscess formation are possible.
At a Blood test are inflammation parameters such as ESR (sedimentation rate) or the White blood cell count elevated.
Imaging procedures how roentgen, MRI and CT can show how far the inflammation has spread and how badly the bone has been damaged.
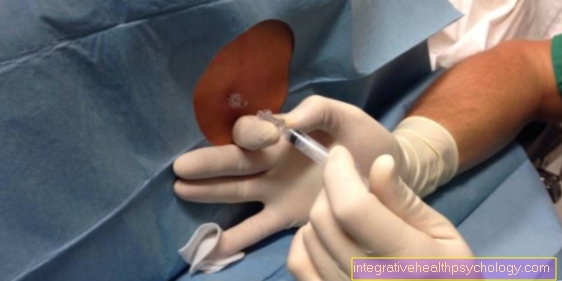
Finally, a biopsy, i.e. a tissue removal, exclude further differential diagnoses (e.g. bone tumor).
Inflammation of the bone in the jaw
Inflammation of the bone in the jaw is not uncommon and can be common start from the tooth system (odontogenic infection). Infections in the mouth or the paranasal sinuses can spread to the bones. Common causative agents of bone inflammation in the jaw are Staphylococcus aureus and Streptococci. In general, the lower jaw is affected many times more often than the upper jaw because its blood supply is less organized.
Infections such as tooth decay, Inflammation of the periodontium (Periodontal disease), one purulent Sinus infections or those caused by a fracture of the upper or lower jaw can spread to the jawbone and trigger an inflammation there. Furthermore you can Cysts and abscesses be the cause of jawbone inflammation in the oral cavity.
A Spread of bacteria from the oral cavity over wounds down to the bone Pulling a tooth (Tooth extraction) happen. Also one Transmission of bacteria through the bloodstream up to the jawbone can in rare cases be the cause of an inflammation in the jawbone.
If the severity of the inflammation allows, an attempt should first be made to deal with the inflammation Antibiotics to manage. The therapy should be here for at least three to four weeks be carried out consistently.
If the drug treatment is unsuccessful, the inflammation must operational be cleared out. It may be necessary to remove individual teeth. In the extreme case, the affected jawbone is removed and a graft used in its place.
The primary goal of therapy, however, is to preserve the bone and its function.
Diagnosis of jaw inflammation
The diagnosis An inflammation in the jawbone can often be discovered by the attending physician clinical picture put.
Next Redness and swelling it also sometimes occurs in the affected jaw area severe pain. It is not uncommon for Fistulas (Connecting corridors) or Abscesses. Sometimes the swelling can already be seen from the outside as a “thick cheek”. Also one Swelling of nearby lymph nodes in the neck area (please refer: Lymph node swelling in the neck) is conceivable. Sometimes those affected complain about strong bad breath. Furthermore, it can lead to fever and an increase in inflammatory parameters such as Sedimentation rate (ESR) or the White blood cell count come in the blood.
A X-ray of the jaw can ultimately provide information about the presence and progression of the inflammation in the bone. Often, however, there is an inflammation of the jawbone in the X-ray to see late, whereas in more elaborate processes like that CT, MRI, or a bone scintigraphy can be seen much earlier.
However, a reliable diagnosis can only be made by a Tissue sample (biopsy). The most important differential diagnosis, a Bone tumor in the jaw, be excluded. A distinction is also made between an acute and a chronic form, which, if left untreated, can persist for months and years.
Inflammation of the bone in the ear
Middle ear infections or ear canal infections can work on adjacent bones like that Temporal bone reach over and trigger bone inflammation there.
In the External otitis maligna (a severe form of ear canal inflammation) develops severe inflammation of the external ear canalthat on bone and Brain nerves overlaps. The causative agent is often called a bacterium Pseudomonaswhich mainly affects patients with weak immune systems (such as diabetics).
In addition to severe pain, it can cause Discharge of secretions come out of the ear. In addition, the patients develop a strong feeling of illness Fever and increased levels of inflammation in the blood.
The doctor (usually an ENT doctor) receives initial information from a Reflection of the ear canal with a special device. The extent of the inflammation can be assessed with CT or MRT imaging, but only a sample can provide clear information, which can also rule out malignant degeneration.
If antibiotic therapy does not work, the inflamed tissue must be surgically removed and, if necessary, a Bone graft can be used.
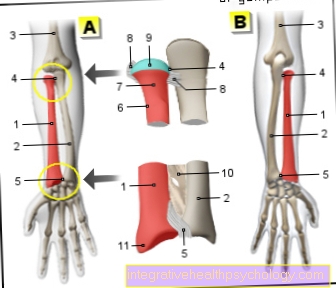
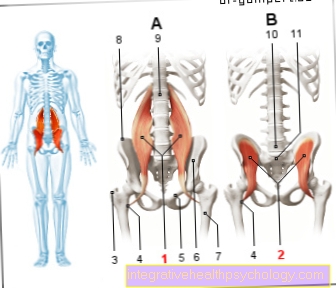
Inflammation of the bone in the leg
An inflammation in the bone in the area of the leg can be washed in via the bloodstream in the form of circulating bacteria (endogenous) or from outside (exogenous) enter the bones from the environment.
This can be done by Skin and soft tissue infections which spread to the bone.
Also through open fractures In the lower extremity, bacteria can get into the bones and cause inflammation. Finally, pathogens can get through Operations and foreign material used like plates or screws or Sampling get into the bone on the leg.
Symptoms can i.a. swelling, pain, and redness in the affected leg, and a general feeling of illness and fever.
The doctor provides the diagnosis on the one hand from the clinical picture of his patient, as well as from increased inflammation parameters in the blood and imaging procedures such as X-rays, CT, MRI or Scintigraphy procedure.
In some cases it is necessary to have a sample in order to examine them microscopically. So can the most important differential diagnosis, a Tumor of the bone, be excluded.
Once the doctor has made the diagnosis, it should be with one Antibiotic therapy to be started. If this does not reduce the inflammation, it must be surgically removed.
Is the bone inflammation infected foreign material like screws or nails in the body, so this must in any case surgically removed to allow healing.
If not adequately treated, the inflammation can become chronic and persist for months to years and lead to the gradual destruction of the bone tissue.
Inflammation of the bone in the knee
Inflammation of the bone in the leg can also affect the joint area of the knee. The pathogens can either be washed into the joint bones via the bloodstream or enter the bone through an external injury.
The inflammation in the bone manifests itself symptomatically as swelling, overheating, redness and pain over the affected knee joint. Mobility can also be restricted.
Here, too, a distinction is made between an acute and chronic form.
Differentiation from inflammatory degenerative diseases of the knee joint such as arthritis is sometimes difficult.
An examination of the inflammation levels in the blood, as well as imaging procedures such as CT or MRI, can provide information about possible inflammation.
If the doctor has made the diagnosis of inflammation of the bone, therapy in the form of antibiotics should be started immediately. If the desired success cannot be achieved with drug therapy, surgical removal of the inflammation must be considered.
In any case, the course of therapy should be closely monitored, otherwise the progressive destruction of bones and joints threatens. Loss of movement and chronic pain can result.
Read more on the subject at:
- Inflammation in the knee.
- Periosteum inflammation on the knee
Inflammation of the bone in the foot
Inflammation of the bones in the foot can have different causes. One possibility is that a non-healing wound on the foot becomes infected and penetrates inward until the bone is infected. On the other hand, bacteria from the environment can come into direct contact with the bone and bone marrow through open bone fractures and thus trigger inflammation in the bones of the foot. Inflammation of the bones in the foot occurs more rarely due to bacteria carried forward in the blood, which can penetrate through blood vessels into the bones and infect them there.
Inflammation of the foot bones becomes symptomatic through local reddening, pain and functional restrictions. For example, movement in the joints can be restricted.
Systemic symptoms such as fever and fatigue can also occur.
If an inflammation of the bones in the foot is suspected, the doctor initiates immediate therapy. This usually consists of the administration of antibiotics, since such inflammations are in most cases bacterial. If the drug therapy does not have the desired effect or if the inflammation spreads systemically or to soft tissues, it may be necessary to surgically remove the inflammation and, if necessary, to replace the bone with a prosthesis. The aim of any therapy, however, is initially to preserve the bone and its function.
Read more on the subject at: Inflammation of the foot or periosteum of the heel
Inflammation of the bone in the toe
Inflammation in the bone can also occur on one or more toes. A common reason for this are non-healing wounds on the toes (Ulcers). These are particularly common long-term diabetics or Circulatory disorders of the legs (PAD or peripheral arterial disease) on.
If the wounds have persisted for several weeks and are deep and extensive, there is a risk of the infection spreading to the bones. In some cases the wound is so deep that the bone surface is already visible from the outside.
Additional evidence of inflammation of the toe bones can be general Redness, swelling, and pain in the toes be. The mobility in the toe joints can also be restricted.
If inflammation of the toe bones is suspected, the doctor will make the diagnosis through the clinical judgment of the affected toe and through Inflammatory parameters in the blood.
Also X-rays can provide information about the inflammation and destruction in the bone. In any case, adequate therapy should be started immediately, which usually consists of the administration of antibiotics. If the course is severe, a operative clearance of the inflamed tissue to prevent the inflammation from spreading to surrounding tissue and adjacent bones.