Fatigue fracture - you need to know that!
definition
Under a fatigue fracture (synonyms: Fatigue fracture, stress fracture) is a broken bone that is caused by excessive stress over a long period of time.
Although the diagnosis is often difficult, once it has been made, the fracture can almost always be completely healed with the help of consistent immobilization of the affected extremity.
Read more on the topic: Stress fracture

introduction
A fatigue fracture is a bone fracture that is caused by long-lasting or often recurring excessive loads. So it does not suddenly come to an acute rupture due to external force, but it takes some time for the rupture to actually develop completely. This can ultimately happen through an unnoticed event.
Such fractures can occur in both healthy and diseased bones and are accordingly referred to as either stress fractures or insufficiency fractures.
Depending on which part of the body there is a fatigue fracture, there are different names for this type of fracture:
- The most common is the march fracture (on the second, third, or fourth metatarsal)
- the Jones fracture (fifth metatarsal)
- the cough fracture (ribs or vertebrae) and
- the Schipper's disease (cervical or thoracic vertebrae)
In addition, the fatigue fracture of the heel is also very common.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- Lumedis - orthopedic surgeons
Kaiserstrasse 14
60311 Frankfurt am Main
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see Lumedis - Orthopedists.
Causes of Fatigue Fracture
A fatigue fracture occurs when the affected bone is permanently overloaded. Every bone has a certain load limit, which is exceeded by tiny fractures in the bone (Microfractures) manifested. These are initially harmless and do not attract attention. Long-term or recurring overloading or incorrect loading can cause a large number of these small cracks. As a rule, the body can compensate for these small fractures by creating more bone substance.
At some point, however, this compensation mechanism is exhausted. As a result, the increased vulnerability of the affected bone leads to a fracture at some point, which is typically not caused by obvious trauma, but rather can be triggered by everyday movement. Due to this development of the disease, it is understandable that (competitive) athletes in particular often suffer from fatigue fractures and that these occur more frequently in the lower extremities.
Women who suffer from a disturbed menstrual cycle or who are going through menopause are particularly affected. If it's because of the hormone estrogen is lacking (at the same time there is also one osteoporosis) before, the bones can break more easily.
Read more on the topic: What kind of pain occurs with osteoporosis?
Some malpositions of the feet also favor the occurrence of a fatigue fracture. This includes the arches of the foot and an outward rotation of the feet when running, which increases the strain on the calf and shin bones. Long, violent coughing can also cause fatigue fractures (especially on the ribs or vertebral bodies).
Read more on the topic: Arches foot
In addition, there are a multitude of risk factors that mean that a fatigue fracture of one of the extremities is more likely to develop, even in otherwise healthy people. These include:
- taking certain medications (for example cortisone)
- a strict, unbalanced diet
- a narrow tibia or a small calf circumference with little muscle mass
- a sudden change in training (e.g. if you change your running speed / distance or the weight to be lifted) and
- Running routes that are either hard, uneven, or longer than 20 miles.
Symptoms and first signs of a fatigue fracture
Characteristic complaints are difficult to identify, especially with a fatigue fracture. The symptoms of a fatigue fracture typically develop insidiously, which is very different from those of an ordinary, acute fracture.
The first signs are slight pain, typically punctiform tenderness in the affected bone areas. Initially, it is pain that occurs predominantly during exercise, later it can also be felt at rest.
Depending on how pronounced the periosteum inflammation over the fatigue fracture is, there may also be swelling, reddening or overheating of the skin in the area.
However, these signs are often mistakenly dismissed as bruises or overuse. In the initial stages, the pain only occurs with exertion and disappears at rest. In addition, the function is mostly still preserved. As a result, most people do not think they have had a fracture.
The only first signs are the pressure pain with swelling and overheating of the region. Since these complaints can occur with many different diseases, it is difficult for those affected to recognize their disease early on.
Over time, those affected also have pain at rest, which does not subside even when fully relaxed. As a result, the resilience of the affected body part decreases more and more.
In contrast to regular bone fractures, fatigue fractures are not accompanied by a sudden loss of function in the affected part of the body, but develop gradually.
Duration of the fatigue fracture
The duration of a fatigue fracture varies with regard to the healing process, depending on the location and severity of the fracture, as well as the adherence to therapeutic measures on the part of the person concerned.
The immobilization (bandage, plaster of paris, orthopedic splinting, relief with crutches, etc.) usually takes two to four weeks, after which the stress can be increased steadily.
It is also important that there is no complete immobilization in the relief phase, but that the affected part of the body is still stressed to a certain extent as part of the physiotherapy so that there is no muscle breakdown and further demineralization of the bone substance.
On average, one can assume complete healing after 6-8 weeks if the break was recognized in time and treated accordingly. Otherwise the healing process can take up to 6 months.
It is particularly difficult to regain full resilience. Even when the fracture has healed, you shouldn't put full weight on immediately, but slowly bring the affected bone back up to the load. A full resilience is therefore usually only possible after about 4-6 months.
A fatigue fracture can heal in two ways. On the one hand, via what is known as primary wound healing through surgical treatment of the fracture. On the other hand, through secondary wound healing with the help of a purely conservative treatment. Secondary wound healing usually takes several weeks. The healing time is thus longer than with the surgical treatment with the aid of which healing takes place after only a few weeks.
In both cases, the prerequisite is that therapeutic measures such as immobilization of the affected area apply. The immobilization alone takes between 2-4 weeks. Only in this way can a fatigue fracture heal without complications and without any consequential damage within 6-8 weeks.
Diagnosis of the fatigue fracture
The diagnosis of a fatigue fracture is often difficult.
Often, athletes simply come to the doctor with complaints of their feet, lower legs or thighs, which are described as unclear pain. If the doctor suspects a fatigue fracture, he will conduct a targeted survey of the medical history (anamnesis).
Important questions here are, for example:
- how long the pain has been going on
- when they occur (permanently or only under stress)
- whether there have been recent accidents or other possible causes of the pain and
- in women: there are abnormalities in the menstrual cycle or whether the menopause has already started
In addition, it is always interesting to find out whether there are other diseases (osteoporosis, foot deformities).
This questionnaire is followed by a physical examination, during which the doctor looks at the painful area and checks whether there has been any swelling, overheating or reddening there.
If a fatigue fracture is still suspected, an X-ray is usually taken. However, many fatigue fractures cannot be seen in the X-ray image, especially at an early stage. So if the image is normal, another image can either be taken after one or two weeks, or computed tomography (CT), magnetic resonance imaging (MRI) or scintigraphy can be performed. The last two of these imaging processes in particular are much more complex and expensive than X-rays, but in case of doubt they can provide a much more reliable and earlier result.
As part of the diagnosis, the doctor must always clarify whether the symptoms could have another cause. Compartment syndrome and shinbone syndrome cause similar complaints, as do some tumors and infections. Probably the most important differential diagnosis of a fatigue fracture is rheumatism. Many patients confuse a fatigue fracture with rheumatic complaints, which is why they see a doctor very late or not at all.
Read more on the topic: Shin splints
Locations of a fatigue fracture
Fatigue fracture of the heel
A fracture in the heel area can cause severe pain in the affected patient. The cause of the fatigue fracture of the heel is in most cases excessive stress when walking and running. For this reason, such fatigue fractures in the heel area can be observed especially in runners and hikers.
In addition to the metatarsus and the shin, the heel is one of those parts of the body where excessive stress often leads to a stress fracture (synonym: stress fracture). In addition, there is a risk of inflammatory processes developing in the area of the bone fracture in the affected patients. For this reason, a specialist should be consulted immediately in the event of existing pain symptoms and the suspicion of a fatigue fracture of the heel.
Patients who have a fatigue fracture of the heel usually complain of severe pain that makes it almost impossible to occur. In addition, the examination reveals significant swelling and redness in the heel area. The diagnosis of a fatigue fracture of the heel is made on the basis of the clinical symptoms and the production of X-rays in two different planes. For this purpose, the foot is shown both from the front and from the side. If the findings are unclear, computed tomography (CT) and / or magnetic resonance imaging (MRI) may also be necessary.
The fatigue fracture of the heel can, depending on the severity and exact location, non-surgically (conservative) or surgically. An uncomplicated fatigue fracture of the heel with well-adapted fracture ends can in most cases be treated with a simple plaster cast. Pain relievers such as paracetamol or ibuprofen can be taken to relieve pain. Despite the plaster cast, the affected patient has to take care of the fractured heel for a period of ten to twelve days.
A dislocated fatigue fracture of the heel usually requires surgical correction. During the surgical procedure, the broken ends are stored together and connected to one another with wires and / or plates. The foot can then be cast in plaster up to the lower leg and thereby relieved. The wires and / or plates can (but do not have to) be removed after a few months. Surgical intervention is also essential if the ankle is involved.
Fatigue fracture in the foot
Since the foot is exposed to enormous stress, especially in runners, this area of the body is where fatigue fractures are particularly common. In people who regularly cope with long marching or hiking routes, the fatigue fracture occurs primarily in the metatarsal area, near the second toe.
Similar to the fracture of the heel, the fatigue fracture of the metatarsus is also noticeable through the sudden onset of severe pain. Classically, the pain symptoms intensify when walking or running. In addition, the broken foot looks swollen and may show severe reddening of the skin.
The fatigue fracture on the foot cannot always be proven by X-rays in the first few days. The production of x-rays in two planes is often only effective in diagnostics with a delay of three to four weeks. The reason for this is the fact that the fatigue fracture on the foot can usually only be detected by the occurrence of typical calcifications in the area of the fracture ends. If the symptoms are appropriate, the suspicion of a fatigue fracture on the foot can only be confirmed by a bone scintigraphic examination or an MRI of the foot. A skeletal calligraphy and an MRI of the foot can reliably demonstrate a fatigue fracture in this area.
The fatigue fracture in the area of the foot must urgently be relieved and immobilized. If the fracture ends are in the area of the metatarsus, a sufficient immobilization can be achieved by wearing a so-called "forefoot release shoe". Decongestant measures such as lymph node drainage and kinesio tapes can be used as support. A fatigue fracture on the foot usually heals completely within 4 to 6 weeks.
You can find out more about this topic at: Fatigue fracture in the foot
Fatigue fracture in the metatarsus
A fatigue fracture in the metatarsus results from prolonged overloading of a joint or a bone and is usually caused without additional external force. Theoretically, you can suffer a fatigue fracture in any bone, but bones that have to withstand particularly high loads are predestined.
It is therefore not surprising that athletes in particular often suffer from a fatigue fracture in the metatarsus. In general, the metatarsus includes the 5 metatarsal bones (Metatarsal bone). Especially with various jumping exercises, it can be that the metatarsus is overloaded.
If this overload persists, the structure of the bone and thus its resistance can change as a result of this overload. For example, a figure skater might want to try out a new figure in which she puts particular stress on the metatarsus, which initially only results in small softening and cracks in the bones in this area of the foot, which then deepen. Especially with such new exercises it can be that you overestimate yourself and especially the strength of your bones and thus provoke an overtired fracture.
Due to the permanent overloading of the metatarsus, a stress fracture can slowly develop. This means that the bone continues to tear due to the constant overload until it finally does not have a sufficient bond and breaks.
However, it is important that a fatigue fracture in the metatarsus, as in any other bone, does not manifest itself like a classic fracture with suddenly severe pain and is due to an event such as an acute fall. Usually, the patient already feels the first mild symptoms in the overload phase. For example, the metatarsus may be slightly swollen or the patient may experience increased pain in the metatarsal area after exercising.
In the case of the fatigue book itself, the symptoms usually intensify, that is, the metatarsus is more swollen due to the fatigue fracture, possibly has a slightly bluish discoloration due to bleeding and that there is more pain.
However, in comparison to a "real“Break does not result in a sudden onset of the symptoms but only in an intensification of the already existing symptoms. This also explains why many athletes may not notice that they have suffered a fatigue fracture in the metatarsus for a long time. The important thing here is to pay attention to the body's minor symptoms.
If the metatarsus is no longer properly resilient and is also slightly swollen and / or red and / or painful, it can very well be that the metatarsal fracture is due to fatigue, which should definitely be treated. In the early stages, it is usually sufficient to keep the foot still and not put any more weight on it, but if you ignore the symptoms and continue to load the metatarsus despite a fatigue fracture, the fracture deepens and surgery may even be necessary.
The most common reason for a fatigue fracture in the metatarsus is excessive jogging. Runners with a weekly volume of more than 50 km / week are at risk. Runners with a weekly volume of 10 - 20 km / week cannot usually suffer a fatigue fracture in the metatarsus.
You can find out more about this topic at: Fatigue fracture in the metatarsus
Shin fatigue fracture
Permanent overloading of the bone is also the most common cause of a fatigue fracture on the shin. In the area of the shin, fatigue fractures are divided into two classes. A distinction is made between fractures of the healthy shin and fractures of the pathologically altered shin. The fatigue fracture of the shin, which is solely due to excessive stress, is also known as a stress fracture.
In the case of pathologically altered bone substance, on the other hand, even light loads are sufficient to cause a fatigue fracture. In such cases, one speaks synonymously of insufficiency fractures. This type of fatigue fracture on the shin is triggered by osteoporotic changes, rheumatoid arthritis or rickets. As a result of these diseases, the shin becomes increasingly porous and less resistant to compressive forces.
Typical symptoms of a fatigue fracture are shin pain, which begins insidiously, increases under stress and subsides again when at rest. In the case of a long-lasting fracture, the pain symptoms become more apparent, so that symptoms become noticeable in the course of the fracture even when the patient is at rest. In addition, swelling and redness can often be observed in the area of the shin. A fatigue fracture of the shin does not usually cause a restriction of mobility.
The therapy of the tibial fracture is carried out by immobilizing the affected leg for several weeks. In most cases, a plaster cast is applied for this purpose. If the fracture ends are poorly adapted, however, surgical treatment of the tibia may be necessary. During the surgical correction, the ends of the bones are brought closer together and connected to one another with special screws and / or a metal plate.
In general, the healing process of the fatigue fracture on the shin is significantly accelerated after surgical correction. The lower leg can be used again much faster.
In most cases, the cause of a fatigue fracture on the shin - as with a fatigue fracture of the metatarsus - is excessive jogging (more than 50 km / week).
You can find out more about this topic at: Fatigue fracture in the shin
Fatigue fracture in the knee
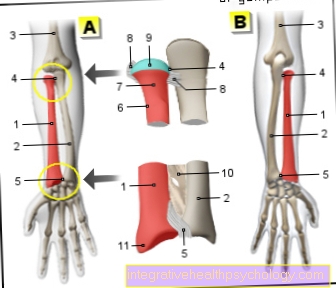
A fatigue fracture in the knee always occurs when the knee is overexerted for a long period of time. However, since the knee is a joint, it is not the knee itself that breaks but one of the surrounding bones. For example, the head of the fibula bone of the lower leg (Fibular) to be affected. This little head is located on the outside below the knee and is particularly prone to fatigue fractures as it is a very narrow bone that is at risk for a fatigue fracture in the knee, especially when the knee is rotated.
As with any other fatigue fracture, it is important that the symptoms manifest themselves slowly and not like a "normal“Breakage can be caused by external forces such as a fall. However, a fatigue fracture in the fibular head usually manifests itself as a significant restriction in movement of the knee and lower leg.
However, a fatigue fracture in the knee area can also occur directly in the kneecap (patella) arise. Especially in athletes who put a lot of strain on their knees, such as gymnasts or dancers, it can happen that the kneecap continues to tear until a fatigue fracture occurs. Such a break manifests itself especially with knee movements through pain, swelling or redness in the area of the knee. Climbing stairs in particular is becoming increasingly difficult for the affected patients because the knee is particularly stressed, but jogging can also cause considerable impairments. Here, too, it is important to pay attention to the signs of a fatigue fracture in the knee and not to underestimate them. Even if a fatigue fracture manifests itself through slowly increasing pain and not through suddenly acute pain, the bone can be damaged just as much as if it is suddenly broken by an external influence (fall, blow ...).
Usually, a fatigue fracture in the knee can be treated well with simple immobilization of the knee, but it is important that the patient also adheres to it and that the knee is not continually overloaded, otherwise permanent damage can occur, which above all are associated with major impairments in the knee.
See also: Pain in the knee
Fatigue fracture in the fibula / outer ankle
A fatigue fracture in the fibula area (Fibular) can arise either in the area of the knee, i.e. on the fibular head, or in the lower area of the fibula, the area of the outer malleolus. Only very rarely does the fibula break through in the middle and when it does, it is more likely through a "normal“Breakage as a result of external forces of violence than as a result of long-term overload such as occurs with a fatigue break.
In the area of the outer ankle (Lateral malleolus), especially if there is a persistent overload during long marches, for example in the armed forces or through hard jogging training, a breakdown in fatigue can occur. This manifests itself in repeated swellings in the area of the ankle as well as redness and pain on the foot. The pain gets worse with strain, i.e. when running but especially when jumping or jogging, as the break then deepens due to the continued strain.
A fatigue fracture in the outer ankle is particularly encouraged if the patient repeatedly kinks while jogging / marching and thereby puts a lot of strain on the ligaments and muscles, but also on the bones.
Here, too, it is important to absolutely spare the fatigue fracture in the outer ankle and to stop training for a longer period of time, otherwise the fracture will continue deeper and deeper and can lead to considerable impairment. Since the first symptoms are usually only expressed by slight swelling and moderate pain, it is important to pay attention to these small signs, otherwise a fracture due to fatigue can usually only be diagnosed at an advanced stage.
Wrist fatigue fracture
A fatigue fracture in general is the result of prolonged stress on one or more bones that together form a joint, such as the wrist. The wrist (articulatio manus) consists of the lower parts of the forearm and the front row of the carpal bones; more precisely, the wrist consists of the spoke (radius), an articular surface (Radioulnar disc) and the 3 carpal bones Os scaphoideum, os lunatum and os triquetrum. Theoretically, a fatigue fracture can occur in any of these bones (although the disc is not a bone and is therefore not further described).
Gymnasts, who often put a lot of strain on their wrists, are particularly at risk, but musicians, too, can strain and irritate the bones in the wrist due to prolonged improper loading that leads to a fatigue fracture. This manifests itself in swelling and slight pain in the area of the wrist, whereby the pain becomes worse under the load and the swelling increases depending on the degree of load.
Since a fatigue fracture only begins insidiously at first, it is important that it is diagnosed in good time, otherwise it can happen that, for example, the upper part of the radius breaks completely. In this case, a simple protection is often not enough, the wrist must be operated on and it then takes a lot longer until the wrist can be used adequately again. Especially since the wrist is responsible for filigree work, a fatigue break in this area should not be underestimated and the first signs should not be ignored.
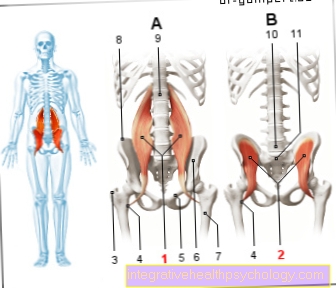
Hip fatigue fracture
Fatigue fractures of the hipbone are rare. There are more frequent fractures near the hip joint, for example the thighbone.
The causes are often sports that are particularly stressful for the lower extremities (cross-country skiing, football, gymnastics, etc.) - a so-called stress fracture then occurs in the hip.
If there is a fatigue fracture in the hip area due to existing osteoporosis, it is an insufficiency fracture.
In the event of a manifest fatigue fracture, those affected must above all respect the immobilization and thus relief and implement it consistently so that an optimal healing process can occur.
The first exercise should be done with targeted and joint-friendly sports such as swimming without footwork with increasing aqua jogging. This means that there is hardly any stress on the hips.
Unfortunately, since the fatigue fracture on the hip is very rare, it is often not immediately recognized as such. It is all the more important that those affected notice the first signs of a fatigue fracture - and take them seriously.
The treatment of such a fatigue fracture varies from person to person. It can heal with conservative measures alone, but sometimes also requires surgical treatment.
Duration vs. Healing from a fatigue fracture
A fatigue fracture always occurs when a bone is permanently improperly and excessively stressed, which leads to a softening of the bone structure. As a result, smaller cracks appear in the bone and the fracture point becomes deeper and deeper.
Compared to a "normal“A fracture caused by external forces such as a fall, the healing of a fatigue fracture, if it is diagnosed and treated in good time, is usually quite problem-free.
First of all, it is important not to put any further stress on the fatigue fracture, as otherwise healing cannot take place properly. This means that the affected bone or joint must be immobilized as far as possible. A plaster of paris is not always required here, splints or bandages are often used, but it is important that any form of sport that would further strain the bone is strictly forbidden, otherwise the fracture will deepen and worsen.
However, if you make sure that the bone or the affected joint is immobilized, a fatigue fracture usually heals within 6-8 weeks without further complications or damage.
Unfortunately, the healing time can vary considerably. E.g. A fatigue fracture on the shin takes significantly longer than a fatigue fracture on the metatarsus.
If bones are affected that are responsible for the functionality of a joint, such as the wrist or knee, it can be helpful to visit physiotherapy in addition to immobilization. During physiotherapy, on the one hand, attention is paid to whether the healing of the fatigue fracture progresses smoothly, and on the other hand, the patient can be helped so that the joint is fully resilient again after the fatigue fracture.
In addition, it is important to use nutrition to support the healing process in the event of a stress fracture. A fatigue fracture leads to a softening of the bone, more precisely it leads to demineralization.In order to counteract this and thus support the healing of the fatigue fracture, but also as a prophylaxis against another fatigue fracture, it is important to provide the bones with sufficient calcium and vitamin D. Calcium is mainly found in dairy products and yoghurt, as is vitamin D. For a sufficient supply of vitamin D, however, it is important that our skin has something on a regular basis Sun because only then can vitamin D be converted into its metabolites that are active for the body. However, these measures are more of a supportive nature.
The healing itself requires the strict protection of the bone already mentioned and should by no means be underestimated.
therapy
Depending on the time of diagnosis and the severity of the fatigue fracture, different treatment methods are selected.
If damage to the bone is detected at an early stage, i.e. before the actual fracture has occurred, it is always advisable to take care of the affected extremity, which in any case means a break in training for athletes. Physiotherapy has a supportive effect at such a stage.
If, on the other hand, the fracture has already formed, the corresponding part of the body must be immobilized with a bandage (more rarely with a plaster of paris) and relieved.
Painkillers can also be used. Anti-inflammatory drugs, local cold therapy, and vitamin or calcium supplements also help to alleviate the pain.
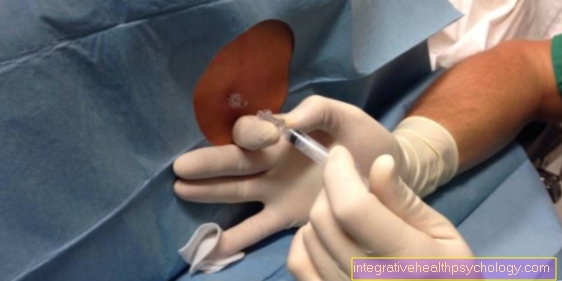
Only if there is a really serious break is surgery performed. Again, there are various methods that are suitable for therapy:
- The so-called intramedullary nailing
- the screwing with titanium screws or
- the spongiosaplasty
Following these surgical interventions, the extremity is immobilized with a splint. Even if this phase is usually “only” about two to four weeks, full resilience is usually only achieved after about half a year.
In addition to treating the fracture, treatment of an underlying disease may of course always be required.
What to do if the break does not heal Shock wave therapy as an alternative
A fatigue fracture usually heals well if treated conservatively and in a timely manner.
However, if the healing of a fatigue fracture takes a long time and the desired results are not achieved after a while, shock wave therapy can be tried as a supportive measure.
In such cases, shock wave therapy can be helpful.
A non-invasive procedure that makes use of acoustic pressure waves is hidden behind shock wave therapy. These pressure waves release their energy deep down as soon as they hit the bone.
In the event of a fatigue fracture, the shock wave is aimed specifically at the point of fracture. This is why one speaks of focused shock wave therapy.
The effect is based on the stimulation of bone growth, as the waves produce and release more bone-forming hormones
The blood circulation is increased, the regeneration of damaged tissue is promoted and pain is alleviated.
The broken bone can grow back together through the newly created bone tissue. As a result, the bone regains stability. The use of shock wave therapy has no side effects and is very low-risk.
Depending on the strength and repetition of the applied shock wave, slight pain can still occur. If shock wave therapy is used to treat a stress fracture, the procedure is usually painless.
Shock wave therapy should not be used in the period of acute inflammation of the periosteum, which often accompanies a stress fracture.
The treatment is usually carried out on an outpatient basis by the orthopedic surgeon, is painless and usually takes 5-15 minutes per application. After about 2-5 repetitions, the first successes can often be seen.
Shock wave therapy is therefore a good alternative to surgical treatment of a fatigue fracture. Depending on the response of those affected to shock wave therapy, it can even replace an operation.
Since this is an individual health service (= IGel), statutory health insurance companies do not pay for shock wave therapy for the treatment of a fatigue fracture. A reimbursement of the costs of such a shock wave therapy unfortunately remains an individual decision at the moment.
For detailed information on this topic, see: Shock wave therapy
Course of fatigue fractures
In general, fatigue fractures progress very well, as the fractures usually heal well with adequate treatment and reduced stress.
However, especially if the diagnosis is made late, it can take up to six months for the affected area of the body to regain its original strength.
Incomplete healing is extremely rare.
Immobilization (especially if done with a plaster cast) requires the administration of a heparin syringe once a day. This is an anticoagulant drug that is supposed to prevent the complication of thrombosis from occurring during therapy. This is the occlusion of a vein by a blood clot, which can be very painful.
A fatigue fracture that is treated conservatively (not surgically) in most cases is healed by the secondary path. This means that inferior bone tissue, known as callus, is formed first over several steps. This bone-like substance is transformed over time through a remodeling process (Remodeling) replaced by stable bone tissue. Secondary healing may take a few weeks.
A surgically treated fatigue fracture with well-adapted fracture ends, on the other hand, is usually healed through the primary route. This means that inferior bone tissue is never formed. Rather, the organism immediately connects the broken ends with stable bone substance. The healing time is therefore usually significantly shorter after surgery without complications. In addition, the treatment results are much better in most cases after the healing is complete.
With the appropriate prophylaxis, however, this side effect can be prevented relatively well.
prophylaxis
To one Fatigue fracture to prevent, it makes sense to do it with any kind of burden Not to exaggerate.
For (competitive) athletes in particular, this means that a Exercise program well worked out have to be. That always includes that Warm up before training that Adhere to from Rest breaks and a special equipment, for example wearing running shoes that are able to cushion shocks somewhat. It is best to look into the care, support one Sports medic who goes that Monitored training and is always available for questions and problems.
In principle of course always, but especially with such athletes it is important to have one balanced nutrition to take care that the body with sufficient Nutrients (Vitamins, calcium) supplies that also for one healthy bone growth are necessary.
In addition, it is of course important to be certain Underlying diseases as a osteoporosis to detect and adequate to to treat, as this risk for one Fatigue fracture considerable increase can.
In addition, especially as an athlete, one should always have the diagnosis “fatigue fracture” in the back of one's mind and with Painthat on not an acute event can be traced back and that persist over a longer period of time, think about it and then necessarily one To see a doctor.