Hip prosthesis
Synonyms in a broader sense
- Artificial hip joint
- Total hip replacement (HTEP or HTE)
- Hip joint prosthesis
- Total hip replacement
- HEP, TEP, HTEP
- Hip replacement
- Hip arthrosis
- Joint replacement
- Hip replacement
- Hip surgery
- Hip joint surgery
- McMinn prosthesis
- Cap prosthesis
- Short stem prosthesis
- Osteoarthritis of the hip
English: hip prosthesis.
definition
The designation Total hip joint prosthesis / hip prosthesis stands for "Artificial hip joint". The Hip prosthesis is the human hip joint modeled and thus basically consists of the same parts.
When a hip prosthesis is implanted, the pelvic joint socket is replaced with one Acetabular prosthesis (= „artificial pan"). The femoral head and the Femoral neck themselves are replaced by the prosthesis socket with an artificial head.
It is possible to use the components mentioned either with or without bone cement bone to fix.
There is also the possibility of a so-called Hemi - prosthesis to implant. In this case, only the femoral neck and femoral head are artificially renewed, but not the socket.
Age
Usually one occurs Hip osteoarthritis between the ages of 50 and 60.
In most cases, hip osteoarthritis is not restricted to one side and therefore occurs predominantly on both sides.
frequency
Every year around 200,000 artificial hip joints are implanted across Germany (= used). Since the number of hip prostheses has increased continuously in recent years, implantation surgery has meanwhile become a "Routine operation“Developed.
As the number of hip joint implants increases, the number of replacement operations is also increasing. It now amounts to around 10,000 per year.
Gender distribution
The gender ratio in terms of the occurrence of a Hip osteoarthritis and associated with it the implantation of a Hip prosthesis is 1.5: 1 (women: men).
Appointment with a hip expert?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The hip joint is one of the joints that are exposed to the greatest stress.
The treatment of the hip (e.g. hip arthrosis, hip impingement, etc.) therefore requires a lot of experience.
I treat all hip diseases with a focus on conservative methods.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Figure hip prosthesis
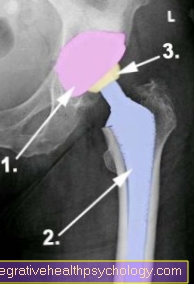
X-ray left hip
(Colored x-ray image)
- Cup of the hip prosthesis
- Prosthetic socket
- Prosthetic head
This hip prosthesis is a so-called cementless hip prosthesis, which is initially clamped in the bone and then grows into the bone.
You can find out more about this hip prosthesis below in this topic.
causes
Such Hip prosthesis surgery is usually necessary when the Hip joint is very advanced. Such an underlying coxarthrosis (derived from the Latin word: "Coxa" (= hip)) always implies a painful change in the area of the hip joint, which occurs due to the pathological wear of the articular cartilage.
Depending on the cause, a distinction is made between hip arthrosis:
- primary coxarthrosis and the
- secondary coxarthrosis.
One speaks of one primary hip arthrosis whenever one cannot name any obvious causes for the development.
From one secondary coxarthrosis one speaks, however, when the disease is based on another, or was caused by it. These causative diseases can be, for example, circulatory disorders (e.g. Perthes disease or the idiopathic femoral head necrosis) or Hip dysplasia be.
Other causes of a Hip arthrosis are among other:
- Inflammation (for example in rheumatic diseases / rheumatism / rheumatoid arthritis),
- But also (chronic) overloads or injuries
- congenital malformations
be.
All incorrect loads or diseases that result in a permanent incorrect load (pre-arthrotic deformity) cause injuries in the area of the joint structures as a result of accidents (e.g. a Femoral neck fracture in older people) or excessive mobility in the area of the joints can have a negative effect and thus permanently negatively affect the hip joint function. Obesity is considered to have an unfavorable influence on the development and course of hip osteoarthritis.
Further information on the development of hip arthrosis can be found at Hip osteoarthritis.
indication
The indications (triggering cause) for implanting a hip prosthesis:
The table below shows the likelihood of an indication Hip prosthesis if the disease is present. This means that such an operation is necessary in around 60% of all cases with primary coxarthrosis.
60% primary hip arthrosis (with no apparent cause)
7% Rheumatoid arthritis
11% Fractures and dislocations, especially the femoral neck fracture
7% Aseptic bone necrosis (femoral head necrosis = circulatory disorder in the femoral head)
9% Other indications (causes)
6% Revisions / repeat operations
Risk factors for hip osteoarthritis
As mentioned above, there are various risk factors that can cause a Hip osteoarthritis increase and thus the likelihood of a Hip prosthesis increase. Some of the essential factors are listed again in the following. You can find more information about some diseases. To do this, simply click on the relevant point.
- Congenital malpositions (e.g. hip dislocation, Perthes disease, epiphysiolysis capitis femoris) that were not corrected in infancy.
- Overload and improper strain at work or in sport
- Joint inflammation (for example in rheumatic diseases),
- Fractures (especially: femoral neck fracture)
- Obesity (not an osteoarthritis risk factor as such. Obesity, however, accelerates the progression of an already existing osteoarthritis).
- Sedentary lifestyle
- Leg length difference
- Idiopathic necrosis (loss of bone mass as a result of insufficient blood supply as a result of injuries (trauma)).
- Bone tumors
Symptoms / complaints
The anamnese (Inquiry about the medical history) to indicate a Hip prosthesis is operated on different levels. First of all, the family history with regard to frequent, early arthrosis, resp. rheumatic diseases questioned.
Also one Personal history (subjective history of illness) seems important to get between the primary and secondary osteoarthritis to be able to distinguish. As part of the personal anamnesis, it is of interest whether hip joint diseases or operations have already taken place, whether there are metabolic diseases or whether the pain extends to other joints.
The arthrosis This is mainly a pain in the groin and buttocks, but it can be from the hip joint from down to the thigh or even that Knee joint radiate into it. Also pain in the area Lumbar spine are conceivable.
In addition, patients often complain of start-up, enema or exertion pain, which can then extend in more advanced stages to pain at rest, which mainly occurs at night.
Because of the for the Hip osteoarthritis typical movement restrictions, which are due to the misalignment of the hip joint and the muscle tension, the quality of life of the patient can be severely restricted. Everyday, "normal" movements are always very difficult: the maximum walking distance is reduced, and putting on shoes and stockings can become a burden.
The picture at the top right shows how the findings of a Hip osteoarthritis represents intraoperatively. The femoral head and socket are removed from the cartilage, which exposes the bone in these areas.
diagnosis
The diagnosis is made based on anamnesis (family history, personal history), physical examination (pain localization) with additional confirmation by X-rays of the affected hip side. As part of a movement test of the Hip joint be flexion, extension, internal and external rotation, as well Abduction and Adduction checked. In the presence of coxarthrosis, the internal rotation in the hip joint is particularly limited; the entire leg appears to be shortened due to muscle shortening.
Read more about the topic here: MRI scan for implants such as artificial hip joints
Types of hip prostheses
Which type of hip prosthesis is used in the respective patient depends not only on age and bone condition but also on the degree of disease of the hip joint.
In general, a distinction is made between partial hip joint prostheses, in which only individual structures involved in the joint are replaced by artificial materials, and the so-called total hip joint prosthesis (Hip TEP), which replaces all joint structures.
Partial endoprostheses of the hip include, on the one hand, the femoral head prosthesis, in which only the femoral head, but not the acetabulum, is replaced. The artificial femoral head is made with a more or less long hip shaft (normal or Short stem prosthesis) anchored in the thigh bone.
On the other hand, it falls McKinn hip cap prosthesis under the partial arthroplasty. The endogenous femoral head is retained and is crowned with an artificial cap after the original cartilage has been removed. The corresponding artificial acetabulum is placed “classically” in the pelvic bone.
The total hip prosthesis, on the other hand, is characterized by the fact that both the femoral head and part of the thigh bone as well as the acetabulum are completely replaced by prosthetics.
Material of a hip prosthesis
The material from which the respective implanted hip prostheses are made can vary and differ from patient to patient and from model to model. In addition, a hip prosthesis consists not only of a single material, but usually of several.
The shaft of the hip prosthesis, which is in Thigh bone is usually made of titanium, just like the prosthetic socket, which will then replace the actual socket. Titanium is often used as a basic material due to its stability, its durability and its good compatibility.
The inlay of the artificial joint socket, which rests on the titanium socket and can be viewed as a kind of joint cartilage replacement, is mostly made up Polyethylene (plastic) or Ceramics. Polyethylene is considered to be particularly wear-resistant and resistant to oxidation. Ceramic has proven itself in long-term use and is therefore suitable for younger, more active patients and patients with metal allergies.
The joint ball head can also be made of ceramic or modified titanium. Material combinations in the sliding pairing are also possible. Basically, all hip prostheses and prosthesis components are nickel-free.
Information on the operation, complications, prosthesis models and signs of loosening can be found on the following pages:
You will find information on the following topics:
- Operation of a hip prosthesis
- Complications of hip replacement surgery
- Short stem prosthesis
- McMinn prosthesis
- Pressure disc prosthesis
Loosening of a hip prosthesis
In the operative orthopedics the implantation of hip prostheses is one of the most successful and uncomplicated interventions. In over 90% of the cases there are no late complications like this Loosening of the prosthesis. Though rare, it can be consequential in less than 10% complication come.
The cause of the loosening of the material can lie on the one hand in changes in the connection between bone and prosthesis or between bone and bone cement, on the other hand in the smallest particles, which arise from material abrasion and which over time are deposited in the surrounding tissue between bone and prosthesis and cause irritation and Can lead to inflammatory processes.
This in turn leads to tissue changes and bone defects, which cause the prosthesis to loosen. This is usually expressed through drawing pains in the groin, the buttocks or the thighs, which become stronger over time, are initially dependent on the load, but can later turn into pain at rest and can lead to the inability to walk.
If there is loosening of the prosthesis, which can be confirmed by adequate imaging (e.g. a X-ray) could be confirmed, another operation to change the prosthesis (Change operation) is displayed.
Hip prosthesis dislocated
If the prosthetic head slips out of the prosthetic socket after a successful implantation operation, one also speaks of a dislocated artificial hip joint or from a so-called Hip prosthesis dislocation.
It is one of the possible Risks after hip surgery, because an artificial joint is generally less stable and resilient than the body's own. Especially in the first 3 months after the operation, there is an increased risk of dislocation, especially due to excessive, incorrect movements in the hip joint, muscular insufficiency, hyperlaxicity of the joint or incorrect position of the prosthesis parts.
If a dislocation has occurred, the artificial joint must be adjusted again under short anesthesia. The complication rate for a dislocation is around 17-18%so that 11-24% of all revision operations are performed on this basis.
The op
The scope of the Surgery to insert a hip prosthesis depends on whether a partial or total endoprosthesis is used, i.e. the hip joint is only partially or completely replaced by artificial prosthesis parts.
A distinction is made between the classic surgical technique of the minimally invasive access techniqueThe latter is preferred due to the tissue protection and the better, faster and less complication-free healing process.
As a rule, the operation is carried out after a prior surgery and anesthesia discussion with the respective specialists general anesthetic carried out.
With the minimally invasive method, the approx. 8-10cm long skin incision in the side of the hip (antero-lateral approach) over the large rolling mound so that the surgeon can then depict the hip joint without having to cut through muscles or tendons. A minimally invasive rear access through the gluteal muscles is also possible (postero-lateral approach). In contrast, with the classic access method, muscles and tendons were or are severed, which then have to be sewn together again and heal.
Next, the joint capsule and the femoral head are removed and the joint socket is milled out so that it is the right size for the artificial socket used. Once this has been done, the acetabular prosthesis part and the associated inlay are inserted.
The following is now the Thigh bone Hollowed out a little and milled out until the desired prosthesis shaft diameter is achieved. Then the stem prosthesis is inserted and a trial femoral head is attached. With this the femoral head is brought into the socket and the joint is thus "composed". If everything fits perfectly, the trial femoral head is exchanged for the original, artificial femoral head.
Finally a Redon drainage placed in the wound, which in the following days allows blood and wound fluid to drain out of the wound. The wound is closed and the skin is closed either with a thread or staple suture.
In general, the insertion of the prosthesis parts can take place without cement or the prosthesis parts are cemented into the bone. This depends in particular on the nature or the condition of the prosthesis-bearing bone portions.
Degree of severity after hip prosthesis
Of the Degree of disability (GdB) is a measure of the impairment of a person due to a disability and comes from the German law for severely disabled people.
Is "just" a hip joint affected and a hip joint prosthesis is only implanted on one side 20% degree the severe disability. If both hip joints are affected and a prosthesis was inserted on both sides, even 40%.
In general, from a degree of disability of 30%, equality can take place at the Employment Agency, from 50% the respective person is considered severely disabled.
forecast
For most patients, a hip joint endoprosthesis can produce good to very good long-term results. Above all, the pain relief in combination with a significantly improved mobility and thus a considerable increase in quality of life has a positive effect.
Surgical intervention in the case of fractures near the hip joint, which tend to be very common in older people, stabilizes the hip joint and promises quick mobilization instead of long weeks of bed rest without surgery.
The service life of the prostheses is limited. As a rule, a replacement operation has to be carried out after an average of 12 to 18 years. The word “average” already implies deviations in both directions. This means that individual prosthesis models can last significantly longer, but the lifespan of the prosthesis can also be significantly below average. There are several factors that can negatively affect the life of the prosthesis. For example, the prosthesis can loosen after a few years due to accidents, overloading, osteoporosis or "material abrasion". A change operation then becomes a necessity.
As one can imagine, however, such change operations cannot be carried out permanently. This means that they should be avoided if possible, but definitely postponed for a long time. All factors that could result in such loosening of the hip prosthesis should be avoided. In particular, excessive overloading of the artificial hip joint by lifting heavy loads or performing joint-jarring sports should be avoided.
Research is currently working on the development of so-called "abrasion-free" materials. This means that sooner or later, on the part of the material, one can speak of “the best starting conditions”. The patient then only has to help with appropriate correct behavior in order to be able to achieve significantly better prognoses.
You might also be interested in: Rehabilitation after installing a hip prosthesis
Sports with a hip prosthesis
Problem: uncontrolled movements!
There are sports that are suitable, conditionally suitable or unsuitable for prosthesis wearers. The classification depends on the frequency of the so-called critical movements. Such critical movements are usually understood to mean extreme movements, such as strong turning movements, compression, movements of the leg towards the body (= adduction), or crossed leg positions. Especially the movements mentioned can be a Dislocation (= dislocation) of the hip prosthesis / hip endoprosthesis cause. This may mean that another operation may be necessary.
As a result, sports that are particularly stressful in the areas of speed and endurance, in which there may still be constant changes of direction, are unsuitable. Most ball sports cannot rule out such critical movements, because uncontrolled movements occur again and again, especially in contact with an opponent (man against man). The ball sports of bounce and bat are an exception. To further unsuitable sports include martial arts, setback games (tennis, squash, ...), jumping sports, alpine skiing and much more. Ask your attending physician whether and to what extent he can still endorse “your” previous sport. He can individually assess what is best for you.
Experts are arguing about the just mentioned sport “alpine skiing”. There are supporters, but also strict opponents. But since it applies avoid critical movements and falls, one can say: experienced skiers who have been practicing the sport for many decades can usually ski relatively safely with prostheses, especially if trips on mogul slopes and in deep snow are avoided and the runs are limited to groomed slopes. However, the risk is extremely high in the event that falls occur.
What do I have to consider when choosing the sport?
As mentioned above, it is extremely important that sports with high impact loads are avoided. Sports that involve abrupt movements should also be avoided.
So far there have been no surveys as to which types of sport could possibly cause the prosthesis to loosen up. However, there are surveys that examined tennis in particular with regard to the loosening of the prosthesis. In summary, it can be said that a minimally increased loosening rate could be determined. However, since tennis as such implies improved muscles in the corresponding hip area, the advantages and disadvantages - statistically speaking - offset each other.
The tennis the double game, as this reduced the number of damaging starts and stops.
Suitable sports:
- Running / walking
- hike
- Cross-country skiing
- To go biking
- swim
- To dance
Conditionally suitable sports:
- golf
- Skittles / bowling
- sailing
- tennis
- Table tennis
Unsuitable sports:
- Alpine skiing
- Soccer
- Handball
- volleyball
- basketball
- horse riding








.jpg)