Hepatitis C virus
Definition - What is the Hepatitis C Virus?
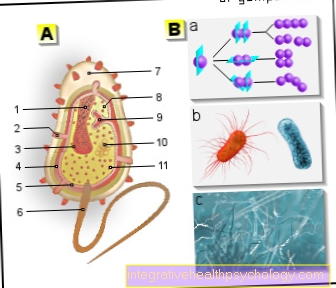
The hepatitis C virus belongs to the Flaviviridae group and is a so-called RNA virus. It triggers inflammation of the liver tissue (hepatitis).
There are different genotypes of the hepatitis C virus with different genetic material. Determining the genotype is important for treatment. If left untreated, hepatitis C quickly and often becomes permanent inflammation of the liver, with damage to liver tissue. The risk of liver cirrhosis and liver cell carcinoma is greatly increased. Around 70 million people around the world are permanently infected with the virus, with its spread particularly striking in African countries, the Middle East and East Asia. In Germany around 0.3% are infected with hepatitis C. Humans are currently the only known host.

What types are there?
The hepatitis C virus (HCV) is a so-called RNA virus.
In comparison, the human genome is stored in the DNA. For protein biosynthesis, for example, the DNA first has to be transcribed into RNA so that new proteins can be formed. There are 6 different genotypes (1-6) for the hepatitis C pathogen due to a high mutation rate. This means that the genetic material of the respective types is different. These genotypes are in turn divided into different subtypes (a, b, c ...) and so far over 80 subtypes have been identified. It has been proven that the genotypes or subtypes differ in about a third of their genetic makeup.
The distribution of the genotypes is striking geographically. Genotypes 1-3 occur mainly in Europe and the USA, with type 1 being the most common in Europe. Unfortunately, it was found that this type 1 responded worse than the others to therapy. In addition, so-called quasi-species of the hepatitis C virus can also occur, which differ only slightly from the genetic material. Renewed infection with another HCV type is possible after hepatitis C has healed due to the different genotypes and subtypes.
Read more on the topic: Hepatitis C.
How does the virus spread?
The virus can be transmitted through different routes of infection. In almost half of the cases, however, the source or route of the infection is unknown.
The main route of transmission of the virus, however, is parenteral (i.e. immediately through the digestive or gastrointestinal tract). This often happens through the so-called “needle sharing” among drug addicts. Since the viruses get directly into the blood, an infection is more likely. The virus can also be transmitted in so-called needlestick injuries, which particularly affect medical personnel. This results in an injury with a needle that was previously in the patient (for example when taking blood).
It can also be transmitted through infected needles when piercing or tattooing. In emerging countries, the risk of transmission through blood reserves, in which the blood is not yet consistently tested due to the high costs, is much higher. On the other hand, the virus can be transmitted “vertically”. This means that an infected mother will pass the virus on to the child. The likelihood of infection depends on the viral load in the mother's blood. In Germany, vertical infection occurs in approx. 1-6% of cases.
The sexual transmission of the hepatitis C virus plays a somewhat subordinate role. Open wounds in the genital and mouth area also result in an increased risk of infection.
What does the viral load mean?
The viral load, or “viral load”, simply means the amount of virus. It determines quantitatively how many virus particles are in the blood of an infected patient. The viral load of the hepatitis C virus is measured by means of PCR (polymerase chain reaction, direct virus detection), whereby the number of HCV RNA is determined and correlated with the amount of viruses.
The hepatitis C virus RNA can usually be detected 1 to 2 weeks after infection. But the viral load is not only determined to see whether an infection has taken place, but also to control the therapy and the course of the disease and to determine how infectious a patient is.
A low viral load at the beginning of the illness can speak for a shorter duration of therapy. In addition, the drop in HCV-RNA in the blood during therapy is an indication of therapeutic success.
If HCV-RNA is no longer detectable 6 weeks after the end of therapy, this indicates that the therapy has been successful and that hepatitis C has healed. If the viral load does not decrease within six months, it is referred to as chronic hepatitis C infection. However, the level of the viral load does not correlate with the severity of the liver cell damage.
You might also be interested in: Hepatitis C test
What effects does the viral load have on the risk of infection?
In contrast to liver cell damage, the HCV viral load correlates with the infectivity or the risk of infection. This means that the higher the viral load in the blood, the higher the probability of the virus being transmitted to the environment. Conversely, the risk of infection would decrease if the viral load was reduced. A combined infection with HIV is usually associated with an increased viral load of the hepatitis C virus and can thus increase the risk of infection.
Read more on the topic: Route of transmission and infection of hepatitis C
How long is the survival time of a hepatitis C virus?
Outside the body, hepatitis C viruses remain infectious for a relatively long time.
However, the survivability of the virus also depends on the surface or medium on which the hepatitis C pathogen is located. In addition, the ambient temperature is decisive for the survival time. It has been proven that the hepatitis C virus has a very long survival time and infectiousness - in some cases up to more than 60 days - with sufficient blood volume (e.g. in syringes) and cooler temperatures such as 4 ° C. However, the infectiousness is already greatly reduced after one day and infection is therefore becoming increasingly unlikely.
Read more on the topic: Vaccination against hepatitis C