Temporomandibular joint pain
introduction
Pain in the temporomandibular joint can be triggered by:
- the bony structures or the joint capsule or
- the muscles responsible for chewing and speaking

Above all, misalignment of the teeth and an asymmetrical jaw closure can increasingly stress the joint and provoke temporomandibular joint pain. Furthermore, worn or poorly fitted dentures can lead to problems in the temporomandibular joint.
Read more on the topic: Temporomandibular joint pain
Causes of TMJ pain
The causes of temporomandibular joint pain can be varied. Since the treatment of this problem should be strictly dependent on its cause, it is important to pay close attention to when the temporomandibular joint pain occurs.
In addition, it is important for the attending dentist to find out under which conditions the affected patients experience relief and which processes aggravate the pain symptoms.
In the most common cases, the so-called CMD syndrome (Craniomandibular dysfunction) causal. This disease is a malfunction of the jaw parts themselves. Severe tooth misalignments that have not been treated or only insufficiently orthodontic are the most common causes of craniomandibular dysfunction, which leads to the patient's perception of temporomandibular joint pain. In addition, this disease often occurs after the wisdom teeth erupt. This is due to the fact that the size of the jaw has decreased significantly over time and therefore does not offer enough space to accommodate 32 teeth. After the wisdom teeth have erupted, there is often incorrect loading of the temporomandibular joint. Typical accompanying symptoms of craniomandibular dysfunction are frequent earache, chronic headache and backache (the neck is affected in most patients), and visual disturbances. In addition, one-sided stress while chewing is considered to be the cause of TMJ pain.
Read more on the topic: Craniomandibular Dysfunction
Many affected patients also report that they tend to grind their teeth in particularly stressful situations. As a result, these patients notice severe temporomandibular joint pain as soon as they get up.
Read more on the topic: Grinding your teeth
Furthermore, bacterial or viral infections can lead to inflammation in the temporomandibular joint and in this way provoke the development of pain. On the one hand, back and neck pain are usually among the most common side effects that occur in the course of TMJ pain, on the other hand, such problems can occur in the The spine area itself can also be the cause of the occurrence of TMJ pain. Other possible reasons for such a pain problem are:
- Tension in the masticatory muscles (also as part of a lockjaw)
- Cysts in the upper or lower jaw,
- Diseases of the ears or sinuses and, in rare cases, various heart diseases
inflammation
Both pain and functional problems in the area of the temporomandibular joint can occur if it is inflamed. One of the most common causes of an inflamed TMJ is problems during the eruption of the wisdom teeth. In people who do not have enough space in the jaw to accommodate eight teeth per quadrant, inflammation of the bone, gum and temporomandibular joint capsule can occur during the growth of the wisdom teeth.
In some cases, simply ablating the affected section of the gum line can correct this problem. However, many patients who suffer from an inflamed temporomandibular joint due to growth difficulties of the wisdom teeth are not spared removal.
Read more on the topic: TMJ inflammation
Disc shift
A cartilage disc (disc) is located in the temporomandibular joint to ensure that the individual parts of the jaw joint slide regularly. Since the temporomandibular joint is one of those joints that are largely stabilized by ligaments, the cartilage disc can slip in the event of severe overloading (disc displacement).
In principle, the disc can slide forward (ventral), backward (dorsal) or to the side (lateral). In dentistry, a distinction is made between complete displacement of the disc and incomplete displacement of the cartilage disc. The latter occurs with many during the wide opening of the mouth, but remains without consequences apart from an audible click, since the disc slides back to its original position relatively quickly.
A complete displacement of the disc without independent repositioning is usually illustrated by an obstruction of the proper mouth opening. An extensive functional dental analysis is carried out to diagnose a disc displacement. In addition, an X-ray or a temporomandibular joint MRI can be useful. If the findings are uncertain, a so-called arthroscopy (joint mirroring) often leads to confirmation of the diagnosis. During the joint endoscopy, a temporomandibular joint irrigation (lavage) can already be carried out in most cases in order to loosen possible adhesions from the cartilage disc.
In addition, inflammatory cells that may have migrated into the joint can be flushed out of the joint chamber. For patients who suffer from a disc displacement with independent repositioning, the production of an occlusal splint is usually the treatment method of choice. Regular wearing of this splint prevents the rows of teeth from clenching and relaxes the masticatory muscles.
In this way, overstressing of the temporomandibular joint is reduced and further displacement of the disc is prevented. In severe cases, manual treatment in combination with special temporomandibular joint physiotherapy can also be helpful. An occlusal splint can also be useful for patients who suffer from a disc displacement without reduction. In addition, surgical repositioning of the cartilage disc may be necessary in order to stabilize it in the long term.
In general, affected patients should be careful not to eat foods that are too hard in the future, as this can put a lot of stress on the jaw joints while chewing.
therapy
Since temporomandibular joint pain can have many causes, the treatment largely depends on the diagnosis made by the dentist.
If the temporomandibular joint pain is demonstrably provoked by worn or incorrectly adapted dentures, it is essential to replace or improve them as soon as possible.
For inflammatory temporomandibular joint pain, the focus of which is muscle inflammation or inflammation of the joints themselves, pain-relieving (Analgesics), as well as anti-inflammatory (Anti-inflammatory drugs) Medication is being taken. If strong tension also occurs in the course of the inflammatory processes, these can be treated with targeted massages and relaxation exercises.
In addition, orthodontic treatment can be useful for patients whose temporomandibular joint pain is caused by asymmetries in relation to the position of the teeth or by crowding of the teeth. In patients who tend to grind their teeth in stressful life situations (Bruxism), or if you bite the halves of the jaw violently, making and wearing a bite splint on a regular basis can usually help.
Read more on the topic: Occlusion therapy
This measure is primarily used to avoid further tooth wear. In addition, the jawbone in the joint is held in a more relaxed position while wearing the bite splint. The result is a rapid reduction in temporomandibular joint pain.
What to do with temporomandibular joint pain
Therapy for TMJ pain includes many methods.
The first thing to do when it first occurs is: stay calm and consider whether a certain event may be related to the pain. These can be previous dental treatments, accidents (fall or impact), colds, poor reclining positions when sleeping or the like. Protection of the joint often brings the desired effect, but only treats the symptoms. It is important that the cause of the problem is found and corrected. Otherwise the temporomandibular joint pain may reappear after a short time.
Hard or tough food should be avoided during this time, as it puts a lot of stress on the joint. Moderate exposure is often perceived as mitigating. Muscle exercises such as opening and closing the mouth in a straight line, self-massage or a slight stretch can loosen the tense muscles. Care must be taken that if the complaints are unclear, there should not be excessive opening or stretching. This could lead to a clamp in the jaw.
Often times, jaw problems are associated with work or family stress. As a result, teeth grinding or clenching and permanently tense muscles are promoted.
This can be prevented by reducing stress through yoga, autogenic training or targeted relaxation of the respective muscle groups (progressive muscle relaxation according to Jacobson).
Lying on your stomach or on your side while sleeping causes unilateral pressure on the jaw joint, which can result in jaw joint pain. The back sleeping position has therefore proven itself in the event of complaints. If the pain is acute, taking a painkiller for a short time can be useful.
In general, however, it can be said that a visit to the dentist is urgently recommended if the pain persists. The temporomandibular joint is part of a complex system in the body, which can also be responsible for complaints in the neck and spine. It deserves professional treatment by a competent doctor who is familiar with all therapy options. For example, he can adapt custom-made occlusion splints. These splints can compensate for a badly adjusted bite and thus prevent pain.
Read more on the topic: Grinding splint, occlusion splint
Physiotherapy and physiotherapy can also be prescribed by the doctor. As a result, muscular complaints that radiate to the temporomandibular joint are weakened or even completely eliminated.
In some cases, psychosomatic treatment can also be effective. This includes occupational therapy, music therapy or body therapy.
Surgical therapy is a last resort. It is only to be used in particularly severe cases. The dentist will be referred to a specialist for this purpose, and the pros and cons must be carefully weighed before the procedure.
Which medications can help?
New therapeutic approaches work with botox and ensure forced relaxation by specifically switching off the muscle activity of the chewing muscles. This muscle relaxation can also be achieved with special medication, which, however, require a prescription.
In the case of severe acute pain, the patient has the option of resorting to pain medication, for example ibuprofen. In the case of self-medication, however, the maximum dose written on the package insert should never be exceeded. In order to ensure safe use, an agreement with the treating doctor is considered useful. This can also determine that for the individually appropriate case.
Relaxation exercises
With many ailments in the temporomandibular joint area, simple relaxation exercises can have enormous effects. When these exercises are carried out regularly, not only do the muscles of the jaw joint relax, but they also seem to have a positive effect on the neck and throat muscles.
Exercise 1: Targeted, deep inhalation and exhalation: During this exercise, the hands should be placed relaxed on the stomach while breathing slowly and as deeply as possible into the stomach. After about three to four breaths, the head is gently pulled to the right side and gently stretched. After taking more breaths, the head should be switched to the left side.
In order to achieve relaxation of the chewing, neck and throat muscles with the help of this exercise, care should be taken not to lift the shoulders but to let them hang loosely.
Exercise 2: Relaxation of the jaw muscles and the temporomandibular joint: During this exercise the patient has to bend his head slightly forward and place the fingertips of the hands on the left and right of the temporomandibular joints. Once the temporomandibular fossa is felt under the fingertips, the fingers are properly placed.
This is followed by 3 to 4 calm, deep breaths, during which you only inhale through your nose and exhale through your mouth. If done correctly, the jaw muscles relax noticeably during this exercise.
Exercise 3: masticatory muscles: Another exercise that relaxes the masticatory muscles in a targeted manner can easily be performed alongside everyday tasks. Patients who suffer from improper stress on the temporomandibular joints should ensure that the tip of the tongue is loosely placed behind the front teeth of the upper jaw several times a day. The lower jaw sinks a little and the masseter muscles relax.
Exercise 4: The masticatory muscles can be trained by pressing one hand against the chin and moving the chin forward against this resistance. This tension should be held for 10 seconds. In addition, the hand can also be pressed against the cheek and the lower jaw pushed against it to the side in order to exercise all the existing massage muscle groups.
Repeating this several times a day can sustainably strengthen the muscles.
homeopathy
There are homeopathic preparations that can alleviate the accompanying symptoms of TMJ symptoms, but they cannot eliminate the source of the problem, as it cannot be reached by globules. If the temporomandibular joint problems are caused by grinding, the preparation Cina D6 can help. Cuprum metallicum D12 can also help with lack of sleep and fatigue. Other globules such as Zincum metallicum D12 and Podophyllum D6 can also reduce temporomandibular joint problems sustainably and strengthen the immune system.
The exact dosage should be discussed with the attending dentist or the oral and maxillofacial surgeon so as not to reduce the success of conservative or surgical therapy by the doctor. Self-medication is not recommended.
Which doctor treats TMJ pain?
The dentist generally treats TMJ problems. However, this is only able to treat the pain conservatively through splint therapy or physiotherapy. If an operation is necessary, you will be referred to an oral and maxillofacial surgeon. Surgical interventions include, for example, punctures of the joint, leveling of the joint surfaces and joint reflections.
diagnosis
For the patient concerned, the choice is one suitable dentist a crucial basis for the therapeutic success of the Temporomandibular joint pain represent.
Ideally, the person concerned should have one Specialists to seek out experience in the field of Temporomandibular joint disease Has. The dentist will be able to determine after an extensive doctor-patient discussion and a few examinations what cause is underlying the temporomandibular joint pain.
Especially when one is suspected Misalignment In the area of the jaw, an extensive examination by the attending dentist is essential. Common research methods include:
- Scan,
- a so-called Functional analysis
- such as X-rays of the teeth, of the Jawbone and the Temporomandibular joints.
Unilateral temporomandibular joint pain
Sometimes the symptoms are unilateral. The reason for this is a natural wear and tear of the body, the TMJ osteoarthritis. This disease, which occurs especially in advanced age due to the constant movement of the joint, becomes favored by one-sided stress on the joint. Cause can be here unilateral tooth loss be.
The osteoarthritis shows through rheumatoid, pulling and yourself pain radiating to the environment. Often she is also with Rubbing / cracking / grinding noises connected. Pain when yawning, Chew, Speak or eat, the up to the neck and shoulder region can radiate are not uncommon. If the temporomandibular joint pain occurs suddenly, one can too wrong lying position be the reason.
Ask less common causes Developmental disorders or Temporomandibular joint tumors They occur mostly on one side and can be determined by the attending physician.
Left and right have the same causes. Everything that can happen on one side can happen on the other. No information is available to suggest that any particular side is affected more often.
Pain
A temporomandibular joint that hurts can have many different causes.
In many of those affected, abnormalities can be found in the area of the bony temporomandibular joint parts. In addition, a temporomandibular joint that is painful is often caused by incorrect or overstressing or damage to the cartilaginous disc.
The main problem with any TMJ defects is the fact that they usually go undetected for too long. In most cases, the affected patients only present themselves to a dental practice when the underlying disease is very advanced.
The masticatory muscles can usually compensate for incorrect loads on the temporomandibular joint, which may occur as a result of osteoarthritis, for a long time. However, this inevitably leads to severe tension and impaired muscle function. At this point in time, the patient is already in a vicious circle, as the osteoarthritis is driven further by counteracting the muscles and the temporomandibular joint usually hurts more. For this reason, it is important for patients with a painful temporomandibular joint to seek dental help as early as possible.
Most causes of TMJ problems can be treated with simple means in their early stages. In most cases, making a special occlusal splint can provide long-term relief from the symptoms. In addition, most of those affected find it helpful to regularly carry out targeted relaxation exercises or physiotherapy measures.
If the temporomandibular joint is acutely painful, pain relievers (analgesics) such as Ibuprofen® or Paracetamol® can be taken.
It can also be that the pain only radiates into the jaw joint, but the cause lies in the jaw itself.
Find out more at: Jaw pain
Temporomandibular joint pain after dental treatment
After a dental treatment, temporomandibular joint pain can occur for various reasons. This is typical here Overloading the temporomandibular jointthat through a Long Duration of treatment and with a corresponding Opening time of the mouth is caused. By a Overstretching of the muscle fibers creates a Fiber injurythat to sore muscles leads. Usually sound this after about 2-3 days off again. However, if the symptoms do not improve or persistent should be a new one after this time Doctor visit occur.
Especially patients with already existing TMJ problems are here endangered and should inform your dentist of any existing symptoms before starting treatment. They can then adjust the treatment accordingly. In addition, a not suitable, so too high / too low filling, Crown, Bridge or prosthesis cause TMJ pain after treatment. When clenching creates a wrong bite position, the rows of teeth can no longer close in their usual position. The body then tries to put the lower jaw in its usual position and presses the rows of teeth against each other. This creates a one-sided (pressure) load on the joint. This can cause teeth grinding or clenching at night. By a easy correction by the dentist (called “grinding in”) this problem can usually be resolved quickly.
Temporomandibular joint pain with a cold
Typically goes one Cold not with TMJ pain hand in hand.
Sometimes you can Jaw pain in the upper jaw arise when the Viruses spread to the sinuses and caused inflammation there. This pain rarely radiates to the upper jaw. If you have a cold or a flu-like infection, however, it is possible that Muscle aches occur. These can then also affect the jaw joint in the head and neck area. Usually this pain will improve after 3-4 days.
A treatment he follows similar to home remedies for a sore throat. Repeated chamomile steam baths are preferable to medication. The tablets should only be taken as directed by the attending physician. Furthermore, a Otitis media affect the temporomandibular joint. This can quickly be triggered by a cold, especially in (small) children, and it affects adults less often. Due to the spatial and nervous proximity, the inflammation can then also be projected onto the temporomandibular joint and trigger a painful stimulus there.
Temporomandibular joint pain with earache
Complaints in the temporomandibular joints can also trigger pain in this region due to the anatomical proximity to the inner ear. Due to the causal tension in the muscles, the muscle cords can block nerve tracts and thus lead to dull pain. Furthermore, the patient can feel a pressure in the ear, which is increased by increased head movements. The blockage can also cause a loss of sensitivity, causing the patient to feel numb in the skin around the ear.
Sensitivity can be so limited that touch can hardly be felt. Jumping out or knocking out of the temporomandibular joint, the dislocation, can also affect the ear as a result of the force that causes pressure pain to be felt. Furthermore, the earache can occur circadian or on special occasions. If the affected person uses the temporomandibular joint heavily, for example when eating, the area of the ear is always stressed if the joint is disturbed and the earache occurs at the same time.
In addition, the symptoms can occur more often in the evening, when the cortisol level is highest, as the irritation threshold is lowered. Cortisol is considered to be a stress hormone that negatively affects the sensation of pain, so that the person affected feels pain most strongly when the level of the hormone is highest. Furthermore, there are no more distractions for the patient in the evening when he wants to rest, which increases the perception of the pain.
Temporomandibular joint pain after braces
Orthodontics shifts the rows of teeth so that a neutral bite is created. It is not uncommon for the patient to develop TMJ problems after the treatment, as soon as all teeth are in the desired position. The new position of the teeth calls for a new adjustment of the temporomandibular joints, which can result in discomfort. This pain mainly occurs shortly after orthodontic treatment with braces and can decrease over time. If this is not the case, the persistent symptoms must first be treated with conservative therapy methods (splint therapy, physiotherapy).
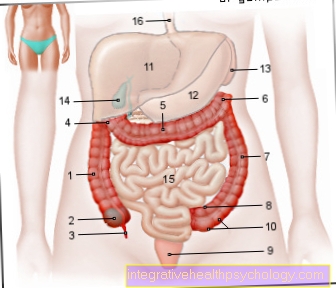
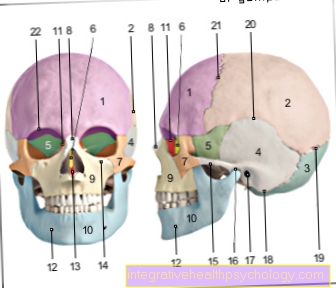
anatomy
The Temporomandibular joint (Latin articulation temporo-mandibularis) provides a flexible connection between the bony Upper- (lat. Maxilla) and the Lower jaw (lat. Mandible) represent.
It works in the jaw joint Mandibular fossa (lat. Mandibular fossa) direct contact with the head of the Upper jaw (Caput mandibulae) a. The upper jaw bone forms the very rigid part of the jaw joint, whereas the lower jaw is almost freely movable. Both structures are only supported by one movable cartilage (Discus) separated.
This cartilage disc divides the temporomandibular joint into two functionally independent parts, the upper and lower joint space. While the upper part of the joint for Sliding movements is responsible, rotary movements occur mainly in the area of the lower joint space.
At Chew or Speak Now these two ranges of motion have to be cleverly combined with each other, i.e. so-called Turn-Sliding movements are executed.
The lower jaw fossa, which forms a kind of joint socket, is forwarded by one under the name Articular tuberosity known structure limited, the rear boundary forms the so-called Retroarticular process.