Jaw pain
introduction
The jaw becomes anatomically the facial skull (Viscerocranium) and consists of two parts, the upper jaw (Maxilla) and the lower jaw (Mandible).
Both the upper jaw and the lower jaw serve as a support structure for the teeth embedded in them.
Jaw pain can originate from both the jawbone and the soft tissue surrounding it (e.g. the muscles) - the causes are very diverse. The pain is extremely stressful for those affected and may severely limit the quality of life.
Everyday things like drinking, eating and talking can be difficult and uncomfortable for people with jaw pain.
However, since it is not always easy to differentiate the exact cause of this jaw pain, it takes time to help the patient in the long term.
Initially, the affected patient can help himself by taking painkillers, but these cannot be taken indefinitely.
Long-term use or excessive doses of painkillers can have a negative effect on the organism and cause severe organ damage.
In the case of long-lasting jaw pain, it is advisable to visit a dentist and describe the problem as precisely as possible.
Visiting an orthodontist can also be advisable in many cases.
Overview of the causes of jaw pain
The causes of jaw pain are very diverse. However, it turns out that the temporomandibular joint is a common trigger for this pain. The temporomandibular joint is a very complex joint that is exposed to great stress on a daily basis. Like any other joint in the human body, this too can wear out over time if it is subjected to too much stress.
TMJ osteoarthritis
Arthrosis in the temporomandibular joint is not uncommon. The word "arthrosis“Is the medical term for joint wear due to overuse that exceeds normal age-related joint wear. Our jaws are actually constantly in motion - when talking, when chopping up food, when swallowing and even at night, often unconsciously. The older you get, the higher the risk that the temporomandibular joint will no longer be able to withstand constant stress and wear and tear will begin.
Improper stress on the temporomandibular joint
Another important cause, which is also related to the one just mentioned, is an incorrect load on the jaw. Such an incorrect load can also have effects on the temporomandibular joint and thus cause the pain or even lead to it itself.
The incorrect loading is usually triggered by missing teeth (often in the posterior region), an outdated crown or a new one that has not been correctly ground in and inserted, prostheses that are no longer well-fitting or tooth filling.
Inflammation in the jaw
Of course, what should not be ignored are inflammation or damage caused by bacteria that cause tooth decay and are often the cause of diseases in the oral cavity.
These bacteria can not only attack the tooth or its root, but also work their way systematically through the tissue and reach the bone, where they trigger an inflammation of the jaw. The diseases of the gums, also called gingivitis or periodontitis, can be preliminary stages that can also cause pain in the bones.
Injuries to the temporomandibular joint
Jaw pain can also occur as a result of an injury, possibly caused by a fall or a blow. The lock jaw phenomenon is also accompanied by pain, as the muscles can cramp when trying to open the mouth.
Grinding teeth
Another cause that affects many people is "bruxism". Bruxism is a grinding of teeth and strong clenching of the teeth, which usually happens unconsciously while sleeping. Triggers can be the following: a misalignment in the temporomandibular joint, an incorrect occlusion (contact between the upper and lower teeth) and, above all, stress and mental suffering.
Because of the course of the nerves, a cold can also radiate into the jaw. Jaw pain can also indicate a heart attack, albeit a very atypical symptom, which is then limited to the lower jaw and radiating to the left arm. Many people also suffer from poor posture, which leads to improper strain on the back and neck and must therefore also be considered as a cause of jaw pain.
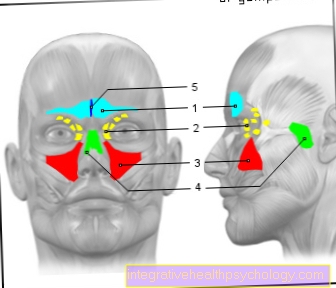
Jaw pain depending on the location
It is useful to classify the jaw pain according to its location - up / down / left / right or combinations - in order to then be able to rule out possible causes. When visiting the dentist, you should describe the pain you are experiencing as precisely as possible - this includes the respective painful area, the quality of the pain, any trigger factors or any other unusual complaints you may have noticed.
Upper jaw pain
The upper jaw is from Maxillary nerve supplied (2nd branch of Trigeminal nerve). Pain in this area can be caused by infections in the jawbone due to periodontal disease (common parlance: Periodontal diseaseDisease), sinusitis, or a single dying nerve on a tooth.
But also fractures, e.g. B. in the area of the front teeth in a fall or tumors can trigger pain in the upper jawbone.
The maxillary nerve is also irritated by constant pressure, so it can be responsible for pain during continuous grinding or night grinding.
Read on here: Upper jaw pain
Lower jaw pain
Of the Mandibular nerve, who takes care of the lower jaw on both sides, is responsible when pain occurs in the lower jaw. As in the upper jaw, the cause can be a fracture, a tumor or other masses, inflammation in teeth due to dying teeth or pain in the temporomandibular joint at the end of the ascending branch of the lower jaw.
In the event of a fall, the chin endangers, so that fractures occur again and again. In this context, i.e. if the chin is subjected to force, it must always be checked whether there is pain in the temporomandibular joint that could be caused by a fracture of the temporomandibular joint head. A "no longer fitting-together of the rows of teeth" is an indirect sign here, which can also be proven by an X-ray image. The mandibular nerve is also irritated by constant pressure. One should pay attention to whether one often grinds one's teeth or presses them together.
Read more on the topic: Lower jaw pain
left or right jaw pain
In many cases, jaw pain is caused by signs of wear and tear in the jaw joint area.
Incorrectly adjusted fillings, prostheses, crowns or bridges as well as hereditary jaw anomalies can trigger these signs of wear. In addition, patients with enormous misaligned teeth often suffer from severe jaw pain.
The symptoms of pain are particularly evident when the temporomandibular joints are moved from the central axis to the right or left. For this reason, joint-related jaw pain occurs mainly when chewing, speaking and biting off. That is, in those movements in which the jaw joints slide to the left or right.
In addition, over-mobility of the jaw can lead to jaw pain. This increased mobility can be triggered by weakness of the ligaments and lead to jaw pain as the joint axis slides to the right or left.
Many patients also have excessive mobility when opening the mouth, which in worse cases can lead to dislocations (Dislocation) can lead. In extreme cases, the jaw joint can no longer be adjusted independently from such a wide opening.
Unilaterally localized pain in the jaw is usually associated with a dysfunction of the gnathological system (Gnathology deals with the question of how the rows of teeth and jaw relate to one another). Dead or dying teeth, tumors or fractures should be excluded beforehand. The symptoms can begin at the base of the lower jaw angle Masseter muscle (a mastication muscle) of the lower jaw over its entire length up to the temporomandibular joint and beyond into the temporal muscles (Temporalis muscle) broadcast.Even the neck, neck and shoulder muscles can then be affected. The cause can be varied. An unsupervised tooth gap, where a tooth from the opposing jaw "grows" into the gap and thus forms an obstacle to the normal chewing process, a wisdom tooth that lacks the antagonist (opposing tooth) or chewed off filling materials. Even chewed prosthetic teeth, the lack of a cusp shape allowing the head of the TMJ to dip too deeply into the socket, can lead to a compression in the TMJ.
Find out more about this topic at: TMJ osteoarthritis
Bilateral jaw pain
Simultaneous pain symptoms on both sides are often the result of overuse of the masticatory muscles with the resulting dysfunction. The mouth can then no longer be opened properly, the temporomandibular joints crack when the mouth is opened and / or closed, and the patient gets the feeling that the teeth no longer fit together properly.
It happens that here physiotherapy has to take place before a splint is made so that the patient can first open the mouth properly again. Only then can an impression be made for a splint.
Situational jaw pain
Jaw pain often manifests itself in colds, when one is under stress or e.g. even after drinking alcohol. Sometimes they only manifest themselves when chewing or are noticeable when grinding teeth. Dental interventions can also cause subsequent pain, for example after an injection, wisdom tooth surgery or root canal treatment.
Jaw pain with colds
In the case of a cold, the maxillary sinuses are often affected, i.e. H. the mucous membranes located there are inflamed, i.e. infected with bacteria. Pain in the jaw area due to a cold in the upper jaw is often related to the close proximity of the floor of the maxillary sinus to the tips of the roots of the teeth in the posterior area. If there is an infection there (sinusitis), the path of the bacteria is very short and the nerve supplying the upper jaw (Maxillary nerve) is temporarily irritated. As the cold subsides, the symptoms usually go away. Therefore, it is possible that a cold can also cause pain in the jaw.
You might also be interested in: Sinus infection and toothache
Jaw pain during chewing movements
If you feel a pain in the jaw while chewing normally, there are several possible causes. The simplest cause is a hard particle such as B. a cherry stone that you bite on. The affected teeth, which are not completely rigidly fused with the jawbone, are attached to fibers (Sharpey fibers) are suspended, pressed down to the bottom of the alveolus (bone compartment of the tooth), which leads to a compression (squeezing) of the nerves entering the tooth there. As a result, the mouth is reflexively forced to open. The situation is similar after a visit to the dentist, in which a tooth has, for example, received a new filling, partial crown or crown. If the height is incorrect, the tooth can hurt so badly when you bite that you can even feel the pain in the jaw.
Read more on the topic: Toothache when chewing
Fillings are often placed under local anesthesia (syringe) so that the numb feeling does not allow correct feedback about the correct filling height. Although the dentist has the option of using a colored occlusion film to check the height, lying down for a long time and keeping the mouth open often falsifies the normal position of the rows of teeth in relation to one another.
Another way to feel pain when chewing can be found in the temporomandibular joint. Between the parts of the upper and lower jaw, which form the temporomandibular joint, there is a cartilage disc, which supports the movement process under normal function. However, if the distance between the upper and lower jaw is too small, compression occurs here as well and, as a result, permanent deformation (compression and permanent deformation) so that the movement causes pain. The reasons for the gaps being too short can be, for example, fillings that are too short, denture teeth that have been chewed down or teeth that have been gnashed.
Jaw pain from grinding teeth
Pain in the jaw area caused by grinding teeth can be felt in the teeth as well as in the jawbone or jaw joint. The pain in the teeth can be caused by the overload and rotational movement (torsion) that occur when the teeth are ground. This results in microcracks both in the outer shell of the tooth (tooth enamel) and at the transition between tooth enamel and root cement (layer on the surface of the root). Tiny parts of the enamel prisms involved in the external tooth structure are almost "blown out" by improper loading. These in turn allow tooth parts that are connected to nerve fibers to react to this fact. Prolonged grinding of teeth can also have led to a loss of height and thus to a lowering of the bite position, resulting in pain in the jaw joint.
Read more on the topic: Grinding teeth in sleep
Jaw pain from stress
Pain in the jaw is often simply a result of stress. Most patients do not even notice that they are constantly grinding their teeth or clenching the rows of teeth tightly together, even if they do it during the day. This behavior is known as bruxism. A tense posture, in which the muscles can no longer find their way back into a relaxed position on their own, can also be an expression of stress. During exercise, you literally clench your teeth, which is only done unconsciously.
Jaw pain from tension
Tension in the jaw muscles is mainly due to misalignments of the jaws in relation to one another. The cause can be unilateral or bilateral incorrect loading due to missing teeth (i.e. due to tooth gaps) and the resulting elongated, i.e. elongated teeth (unimpeded growth in length), damage to the temporomandibular joint, poor working posture (e.g. bent sitting at the computer) or accidental damage that is not due to scarring of the muscles Allow more relaxation of the muscles.
In addition to physiotherapy, physiotherapy (including osteopathy) or muscle relaxants (drug for chemical muscle loosening), relaxation techniques such as progressive muscle relaxation, meditation, yoga or Pilates can also lead to relaxation and end the jaw pain or prevent it from developing in the first place.
Jaw pain after drinking alcohol
Pain in the jaw area after alcohol consumption is usually reported by teeth that have already been damaged and show an inflammatory reaction that has started or has taken place. When you drink alcohol, the blood vessels inside the tooth pulp (nerve) expand and you can literally feel your own pulse. Alcohol consumption after surgery has proven to be extremely bad. The mechanism of widening the blood vessels again plays a decisive role. The blood vessels that are already closed cannot withstand the pressure and open up again, causing secondary bleeding with corresponding pain. This can lead to the piercing (surgical method for vascular occlusion) of the vessel if a pressure bandage is no longer sufficient.
Read also: Toothache after consuming alcohol
Jaw pain after root canal treatment
Carious defects that are not treated over a long period of time cause severe stabbing and / or throbbing pain after a while. This jaw pain is a warning sign. The affected patient should urgently consult a dentist and promptly initiate appropriate treatment.
Deep carious defects that have already penetrated the tooth structure and opened the medullary cavity can damage the nerve fibers and cause the tooth to die. In these cases, the jaw pain that occurs can usually only be relieved by a so-called root canal treatment. In the course of this therapeutic measure, the tooth pulp and the nerve fibers embedded in it become complete away and the root cavity through a artificial Filling material closed.
But jaw pain can also recur after a root canal treatment. There can be various causes for this phenomenon. Patients who suffer from jaw pain in the same localization after a completed root canal treatment should consult a dentist promptly. An X-ray examination of the affected tooth can quickly provide information about which measures must be taken and whether the tooth can still be preserved. In everyday clinical practice, it has been shown that pain after a root treatment is usually not a good starting point for tooth preservation.
On the one hand, the recurrence of jaw pain after root canal treatment could be due to the fact that the first attempt at treatment no Complete evacuation of the root canal has taken place and there are therefore still bacteria in the root canal system. Performing a root canal treatment is very complicated, especially for patients who have very narrow or crooked root canals. On the other hand, jaw pain after root treatment can be an indication of the formation of a cyst in the area of the root tip.
You might also be interested in: The jaw cyst
Jaw pain after a wisdom tooth operation
Even before an operation, erupting wisdom teeth cause great problems for the patient. The wisdom teeth are a rudiment from prehistoric times, when humans had to chew food even more by chewing. Nowadays they are no longer needed.
However, every second person does not have enough space for the figure 8, so that when they break through, there is pain in the jaw. If the teeth remain in the jaw, they usually do not cause any problems, only the eruption brings the suffering. If they break through only partially, they are an easy target for bacteria, which can also migrate into the jaw and cause pain.
Read more on the topic: Operation on the wisdom tooth
Jaw pain after wisdom tooth surgery is not uncommon and is part of the normal healing process, such as a thick cheek, bruising and difficulty swallowing. They arise from the procedure that takes place under anesthesia. The wisdom teeth are usually very deep and wedged in the bone, so that the bone is affected during the procedure and has to withstand great loads. As a side effect, there is also jaw pain after the operation, but it should get better over time.
Nerve endings are exposed and the tissue fluid required for healing can also cause the pain. If this does not improve, however, it is strongly advisable to visit the attending physician again, as alveolitis sicca could possibly have developed, which causes the further jaw pain. In alveolitis sicca, the empty tooth socket becomes inflamed by bacteria, as the protective blood glaucoma has disintegrated or has not developed.
Jaw pain after an injection
A syringe can be used during dental treatments to relieve the patient of the pain and make the procedure as bearable as possible. Usually these jaw pain occurs with a restricted mouth opening. This is also called a jaw clamp.
This is because the needle may have broken a blood vessel or bleed into the tissue when the needle was injected. The vascular injury can result in a bruise. However, this type of jaw pain disappears on its own after a certain time.
Side effects in addition to jaw pain
Often, jaw pain is accompanied by ear pain or headache. A cracking jaw joint can also occur and unsettle the affected person. Some jaw pain can in rare cases also indicate a heart attack.
Pain in jaw and ear
Diseases of the teeth, the tooth supporting apparatus or the temporomandibular joints do not only cause symptoms that are limited to the oral cavity.
In many cases, jaw pain is combined with painful sensations in the ear. During chewing, biting or speaking, many patients experience jaw pain that extends into the ear. This phenomenon is mostly caused by excessive or incorrect loading of the temporomandibular joint.
In addition, strong tension in the masticatory muscles can lead to jaw pain that radiates to the ear and puts a lot of strain on the patient. In these cases, a targeted massage of the tense muscles is often felt to be soothing. A long term cure is this way, however Rare possible.
Both stress-related and tension-related jaw pain with involvement of the ear should be assessed by a dentist. In many cases, the symptoms can be dealt with very quickly by simple means such as grinding splints or physiotherapy.
Read our article on this: Pain in jaw and ear.
Headache and jaw pain
Headaches usually go hand in hand with jaw pain and occur especially as a side effect if the problem has existed for a longer period of time. The above-mentioned wear and tear on the temporomandibular joint can not only lead to jaw pain, pain when chewing, speaking or yawning, but also to headaches.
The permanent incorrect stress caused by grinding and pressing at night or dental prosthesis work that causes problems can also cause headaches as a further side effect. The individual parts of the body cannot be assessed separately, but all work together must be viewed as a whole system. A cold can also cause headaches, for example from constant sneezing.
In addition to jaw pain, wisdom teeth can also trigger headaches. Frequently, however, the accompanying symptoms of headaches also lead to misdiagnosis, as the causes are widely spread. The fact that jaw pain is often not limited to the jaw area due to its origin is also shown by the fact that temporomandibular joint problems cause ear pain very quickly.
Cracking jaw joint
Temporomandibular joint noises (cracking) are in principle harmless in the majority of cases and must Not must be treated. Nevertheless, patients who frequently experience a cracking in the temporomandibular joint should consult a dentist in order to rule out a serious underlying disease.
Extensive diagnostics are particularly useful if jaw pain and / or restrictions in the range of motion are observed in addition to the cracking.
In the case of noises caused by the temporomandibular joint, a distinction must be made between so-called rubbing noises and the real click.
In many cases, rubbing noises do not require treatment, but can also be a first indication of a change in the shape of the joint head (for example due to osteoarthritis). In addition, such rubbing noises can also be caused by the smallest cracks in the area of the cartilage disc (disc) of the temporomandibular joint.
A click in the temporomandibular joint, however, usually indicates a shift in the position of the cartilage disc.
Learn more about this: My jaw joint cracks
Jaw pain indicating a heart attack
Pain that radiates to the lower jaw can actually be an indication of a heart attack. The typical signs of a heart attack are sudden and persistent chest pain, often radiating to the left arm. They can also reach into the stomach or between the shoulder blades. In addition, there is a sallow complexion, cold, damp hands, cold sweat on the face, severe shortness of breath, which can increase to the point of death. If these symptoms occur in addition to the jaw pain, an ambulance should be alerted urgently.
Read more on the topic: Heart attack
forecast
The prognosis for all possible pain in the jaw area is generally good if prompt medical or dental treatment has taken place and the patient shows a high level of cooperation.
A possible exception are the defects in tumor occurrences. Here, the primary tumor and the course of the disease as well as timely treatment are decisive. In second place are temporomandibular joint damage, as there are few options for complete recovery; osteoarthritis can develop that is no longer curable. All other causes such as pure muscle pain or inflamed teeth are usually healed after a few days.
Duration of jaw pain
The duration of the pain in the jaw always depends on the underlying cause. A fracture no longer hurts if it has been treated appropriately, e.g. screwed with metal plates. Muscle pain no longer hurts when a muscle has learned to relax again in addition to tension or if it has been helped to relax through external intervention (physiotherapy). Temporomandibular joint pain often subsides with the insertion of a grinding splint and teeth in the jaw no longer hurt if the inflammation sources have been removed or pain medication has been taken. All causes together are based on the assumption that the patient fulfills his part in the healing process and allows himself to be guided.
Treatment options for jaw pain
Since many patients who suffer from jaw pain have purely mechanical causes, treatment can be relatively simple.
If the jaw pain is caused by crowns, bridges and / or tooth fillings that are too high, it is advisable to have them replaced or abraded by a dentist. Many patients already feel great relief after this simple measure and notice a decrease in jaw pain.
A so-called functional splint can serve as a therapeutic approach for patients who grind their teeth heavily at night or who bite their jaws too tightly. The splint acts as a buffer between the teeth of the upper and lower jaw and reduces the forces acting on the temporomandibular joints. These patients can easily help each other out in everyday life.
If the tongue is consciously placed against the palate, behind the incisors, the masticatory muscles relax automatically and the joints are relieved.
If a misaligned tooth and / or jaw is the reason for the development of the jaw pain, an orthodontist should urgently be consulted. He can assess exactly to what extent an improvement can be achieved and which orthodontic measures are necessary to help the patient and reduce the jaw pain.
Home remedies for jaw pain
Home remedies for pain in the jaw area can only be used sensibly if the cause of the pain symptom is known. This would mean, for example, that the warmth, which one perceives as beneficial and relaxing when the chewing muscles are tense, has a counterproductive effect on the inflamed tooth. Heat would even increase the pain here, as the heat supplied can intensify the inflammation.
A painkiller like ibuprofen can "take the edge off" of the pain until you have the opportunity to go to the dentist for an appointment.
Read more on the topic: Home remedies for toothache
Homeopathy for treating jaw pain
In the case of jaw pain caused by overstraining the jaw by grinding and pressing (bruxing), naturopathic treatments such as homeopathy can also help. A large number of preparations aim to alleviate the triggers such as nervousness, emotional stress, pressure to perform or sleep disorders with the help of globules (Latin: spheres). As a rule, they consist of a sugar component and diluted active ingredients such as B. Cina D 6, Cuprum D 12, Phytolacca D 6 or magnesium phos. D12. Which of these active ingredients can specifically counteract nervousness, exhaustion or stress remains a decision of the treating doctor or advising pharmacist.
diagnosis
If you have severe pain in the jaw area, you should make an appointment with a dentist as soon as possible. This is the first point of contact and the doctor refers you to an orthodontist after assessment and if necessary.
The attending dentist examines the area in the mouth and will then usually arrange for an X-ray, on which the bone structure and perhaps a possible inflammation can be seen and examined. Subsequent treatment steps or referrals to another specialist will then be initiated to treat the cause of the jaw pain.
Which doctor is the right contact person?
In addition to the family dentist with special knowledge of functional diagnostics and analysis, the oral and maxillofacial surgeon is also a suitable contact person for pain in the jaw area. Because the complaints can originate from both the jawbone and the muscles surrounding it.
An ENT doctor can also be consulted in the case of jaw pain that could have arisen due to a cold or the like, but usually the cause is in the temporomandibular joint area or in caries.
Recommendations from our editorial team
- TMJ arthrosis
- What you should know about TMJ pain
- The craniomandibular dysfunction
- The therapeutic bite splint
- The TMJ
























-de-quervain.jpg)



