Complications of spinal anesthesia
Side effects, risks and complications
Performing spinal anesthesia is comparatively low in risk and side effects. In the days after the SPA, headaches can occur (so-called post-spinal headaches). This is caused by the not always avoidable loss of cerebral spinal cord water and is always easy to treat.
In addition, urination disorders can occur if the effect of the spinal anesthesia has not yet been completely eliminated. However, if these symptoms occur, they will go away within a few hours.
Furthermore, the injection site can be infected.
The following complications are mentioned for the sake of completeness, but they are extremely rare:
- Slow heartbeat, drop in blood pressure or paralysis of breathing. However, these complications can be treated well through the use of emergency medication.
- Damage to the spinal cord from the puncture needle
- Allergic reactions to the local anesthetic
If a larger vein is pierced during the puncture, the escaping blood can compress the spinal cord and, in the worst case, lead to permanent damage.
However, this risk can be minimized considerably by checking beforehand whether the blood has the normal ability to clot when it emerges from a vessel
What must be considered before applying spinal anesthesia?
To minimize the risk of spinal cord compression from blood leaking from a vein, the ability of the blood to clot must be checked. This ability is among other things after ingestion anticoagulant drugs limited. In a preliminary discussion, it can be clarified with the anesthetist when these medications can no longer be taken. The following times apply as a rough guide:
- Unfractionated heparin must be discontinued 4 hours before an SPA (spinal anesthesia), low molecular weight heparin 12 hours beforehand.
- Non-steroidal anti-inflammatory drugs (e.g. ibuprofen, diclofenac, etc.) may last 24 hours before the SPA (spinal anesthesia)
- There must be at least 3 days between taking acetylsalicylic acid (aspirin) for single doses greater than 100mg per day and a SPA
- The intake of clopidogrel (Plavix®) should be stopped 10 days beforehand
- Marcumar or warfarin must first be switched to heparin
It should also be noted that this information does not exclusively refer to medication that has been prescribed by the doctor: Even taking painkillers on your own responsibility in the days before the operation can significantly increase the risk of bleeding.
When should spinal anesthesia not be performed?
Spinal anesthesia should not be performed if:
- Blood clotting disorders
- Infections / skin diseases in the area of the injection area
- Severe cardiovascular disease
- Anemia (so-called hypovolemia)
- Head-down position during the operation
- Increase in intracranial pressure
In individual cases, however, the anesthetist will decide whether there are any concerns about the implementation of a SPA (spinal anesthesia).
Read more on the topic: Xarelto®
Who Needs an Epidural Blood Patch?
Cerebrospinal fluid punctures or spinal anesthesia can lead to small openings in the membranes of the spinal cord.
Usually these openings close on their own very quickly.
In some patients, however, these remain open for a few days or sometimes longer and severe headaches develop.
These are usually stronger when standing than when lying down.
The so-called liquor leak should be closed with the blood patch and the pain should subside.
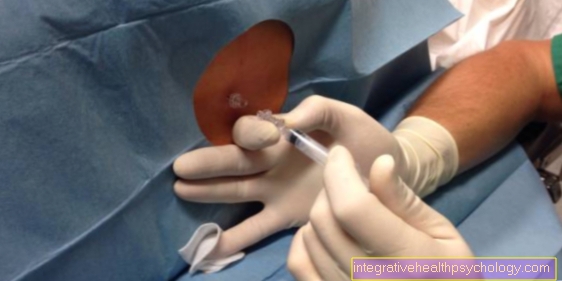
This involves taking some blood from the patient and applying it to the areas that have remained open, so that they scar and the openings close.
This procedure only takes place if the CSF leak does not close by itself.
Can a headache be permanent?
Usually the headache disappears after a few days after spinal anesthesia.
In rare cases, however, the pain can remain for a longer period of time.
Some sufferers report headaches that still occur after more than a year.
In those affected with persistent headaches, a blood patch or surgical repair of the CSF leak can be carried out, which in most cases ends the headache.
Can nerve root irritation occur?
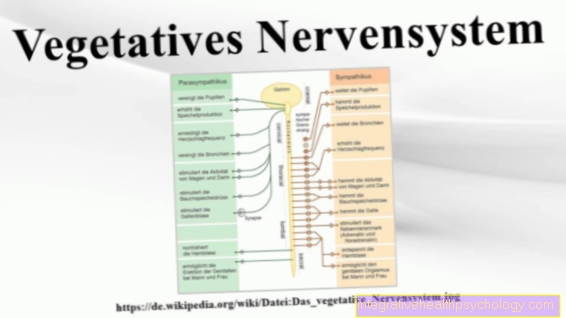
Nerve root irritation describes an irritation of the first sections of the nerves that emerge from the spinal cord.
This can manifest itself in different ways.
Some people experience pain, others report numbness in their legs or abnormal sensations.
The irritation can have various causes.
In spinal anesthesia, a cannula is pushed between the vertebral bodies up to the spinal cord.
Nerve damage can occur here, although this is very rare, since the spinal cord is no longer affected in the spinal canal section.
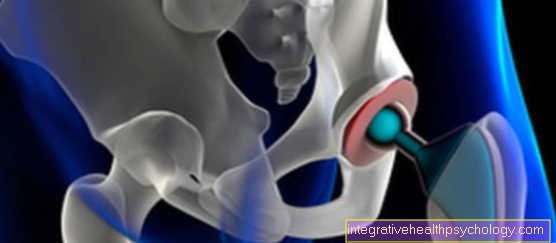
After spinal anesthesia, a bruise can form in the spinal canal.
This can put pressure on the nerve roots and thereby also lead to paralysis, pain or numbness.
These symptoms are very similar to a herniated disc.
The location of the numbness and pain is often not in the back itself, but in the area of the body for which the nerve root is responsible.
For example, with spinal anesthesia in the lumbar region, numbness can occur in the legs.
In most cases, symptoms resolve with the bruise.



























.jpg)