Lichen Ruber
introduction
Lichen planus is a chronic disease of the skin (dermatosis) in which the symptoms of itching and skin changes are in the foreground.
There are different forms of lichen planus, which differ greatly in their appearance. Lichen planus is the most common, less common forms are lichen planus mucosae, lichen planus verrucosus and lichen planus acuminatus.

The epidemiology
Lichen planus is a relatively common skin disorder. About every 100th person is affected, with the peak of the disease between the ages of 30 and 60. Small children only very rarely suffer from lichen planus, if so usually after a flu-like infection. Men are affected slightly more often than women.
The reasons
Why a lichen planus develops has not yet been conclusively clarified. However, it is assumed that this clinical picture is an autoimmune disease. This means that the body's own defense cells wrongly classify the body's own cells, in this case cells from the lowest cell layer of the epidermis, as dangerous and therefore attack them.
This triggers an inflammatory reaction in the affected skin layer. In addition, it is assumed that there are certain risk factors that can promote the development of lichen planus. These include:
- Viral diseases (viral hepatitis)
- other skin diseases (psoriasis)
- certain medicines and
- some chemicals
In addition, there is a familial predisposition to lichen planus.
The symptoms
Symptoms differ depending on the type of lichen planus. In the classic lichen planus, there are blue-reddish, flat papules that are sharply delimited at the edge, which are often grouped and can also flow together to form regular plaques.
Typically, the papules have a fine white reticulated pattern on the surface that can be stripped off. This drawing is also known as the “Wickham Stripe”. Some areas of the skin are particularly often affected by these skin changes, including
- the flexors of the wrist and knee
- the lower back
- Lower leg and
- soles
These inflammatory changes are often accompanied by more or less pronounced itching. Occasionally it also happens that the nails are affected, which can then become thinner or even fall out.
Lichen planus typically has an intermittent course, which means that the skin changes can persist for several months or even years, then disappear and return at some point.
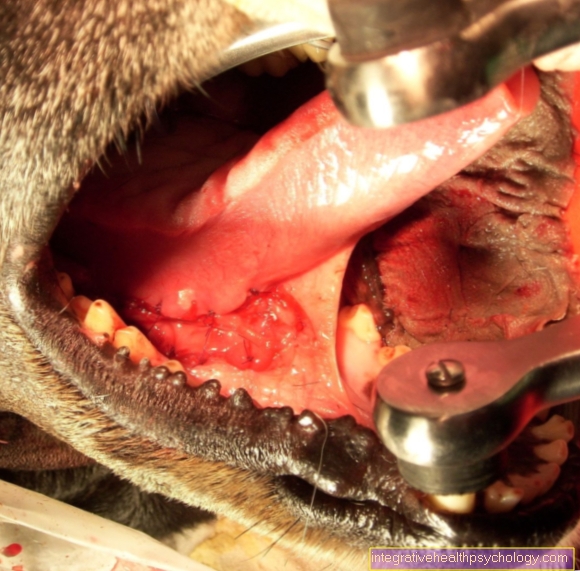
The lichen planus mucosae affects the mucous membranes
- Mouth / lips / tongue
- the outer section of the anal canal and
- the genital area (vagina or penile mucosa)
The papules resemble those of lichen planus, but are less likely to be associated with itching.
In lichen planus verrucosus, large red wart-like foci form, which in the course often lead to scarring. Lichen planus acuminatus is characterized by an infestation of hair follicles, which can lead to hair loss.
The diagnosis
The diagnosis is usually based on the characteristic clinical picture. To confirm this, a tissue sample can be taken from an affected area and examined finely (histologically). A thickening of the top layer of skin, defense cells and deposited antibodies can be detected under the microscope. In addition, blood tests (for example, if viral hepatitis is questionable) can sometimes be helpful.
It is important to rule out certain differential diagnoses, such as psoriasis or allergic reactions to certain drugs, before starting treatment.
The therapy
Treatment is not always necessary for lichen planus, as in most cases it resolves itself spontaneously. The prerequisite for this (just like for successful therapy) is to switch off any triggers such as medication.
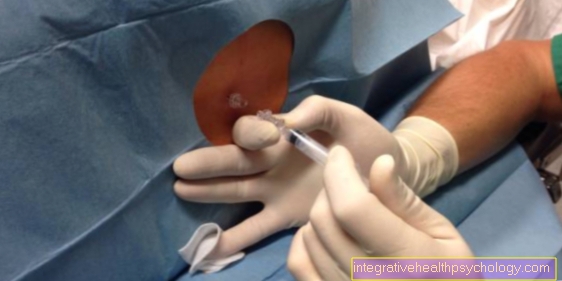
Only around 20% of patients benefit from therapy.Various cortisone preparations are available here to curb the inflammation and itching. Usually topical ointments or plasters are preferred first. If the symptoms do not improve or the infestation is very pronounced, crystal solutions can also be injected or cortisone tablets can be taken for a short time.
Another option is local light therapy or local photo chemotherapy (PUVA). Further radiation options are UVB therapy or a balneo PUVA. If all therapeutic options have been exhausted and have not led to sufficient improvement, a more aggressive, immunosuppressive treatment, for example with ciclospoprin A, can be carried out.
Prognosis
If the therapy is carried out consistently, the lichen planus will usually heal after a few months (on average around 9 to 18).
However, in most patients, relapses (= reappearance of the disease) occur at some point. In some cases, foci that elude a successful therapy can mutate into a precancerous stage (precancerous disease), which is why it makes sense to visit a doctor regularly for follow-up checks if the infection persists for a long time.
The prophylaxis
Since it is not yet known for sure what causes a lichen planus, it is not yet possible to effectively prevent this disease.
The different forms
Lichen planus
Lichen planus is the most common type of lichen planus and occurs in both men and women. The disease manifests itself as small reddish nodules with a clear border, which are accompanied by inflammation and itching. These so-called papules occur predominantly in the area of the flexor side of the wrist, on the lower back, on the knee and on the skin of the lower leg and forearm.
The exact cause of lichen planus is still unknown. So-called autoantibodies are one approach to explaining lichen planus. These are proteins of the human immune system, which in this case normally recognize and mark foreign substances. This allows immune cells to quickly and effectively eliminate these invaders. But if these antibodies are disrupted in an autoimmune disease, the body forms antibodies against the body's own tissue and damages it.
There is currently no direct method for curing lichen planus. Fortunately, the papules go away on their own after a few months. The main aim of therapy is therefore to alleviate the symptoms of the skin disease. This is usually done through cortisol therapy. A healthy diet, radiation therapy and the avoidance of frequent stress also have a positive influence on recovery. In addition, you shouldn't scratch yourself despite itching to avoid additional inflammation.
It is also important to know that lichen planus can occur in phases. This means that even after successful treatment and the symptoms disappear, the disease can reappear at a later point in time. In this case, the therapy starts all over again.
Often, skin ulcers such as those found in lichen planus are associated with cancer by laypeople. In the case of nodal lichen, however, this is not the case, as the papules neither grow into foreign tissue nor even scatter throughout the body. Despite the harmless course of the skin disease, a doctor should be consulted in order to rule out related diseases.
If you would like to find out more about the topic, read our next article at: Lichen planus
Lichen planus exanthematicus
Lichen planus exanthematicus is another variant of the lichens planus. It often shows up on the typical parts of the body that are affected by this skin disease. Mucous membranes and nails may or may not be involved. It is characterized by reddening of the skin and bumps in the skin caused by inflammatory processes. In technical jargon, one speaks of an erythemaopapular character. The bumps in the skin are known as nodules or papules. In the exanthematic lichen planus, these can be hexagonal.
Sometimes whitish stripes can also appear on the skin or mucous membrane. They are a sign of the widening of a certain layer of the epidermis. These strips are called Wickham strips. The diagnosis is often a visual diagnosis.
Exanthematic lichen planus is one of the most common skin diseases. Men are more often affected than women. The cause has not yet been fully clarified. Lichen planus exanthematicus is treated with antihistamines, with topical steroid creams and, if necessary, with an operation, an occlusion. In addition, tar is used for treatment and there is an injection with steroid crystal suspension. In some cases, radiation is also done. Acitretin, chloroquine, azathioprine, ciclosporin and DADPS are used as medication.
Lichen planus mucosae
The lichen planus mucosae is a chronically recurrent disease of a mucous membrane, but mostly of the oral mucosa. Mucous membranes are found in various parts of the body, including the intestines, the nose, the uterus and the mouth. Their task is a mechanical protection of the underlying organ, as well as secretion and absorption of substances.
The mucous membrane (mucosa) lines cavities in the body and is covered by a layer of mucus - hence its name. A defect in the mucous membrane can lead to a loss of function or even death of the affected organ. Lichen planus mucosae can best be translated as “nodular lichen of the mucous membrane”.
The cause of the lichen ruber mucosae is the subject of research, one suspects a drug-induced or autoimmune process. The therapy of the lichen planus mucosae is also here lengthy and difficult.
Lichen planus verrucosus
The word "verrucosus", from the Latin for "wart-shaped" describes this sub-form of the lichen planus relatively aptly. It occurs preferentially on the extensor sides of the lower legs and less often on the back of the hand and is considered to be particularly resistant to therapy and therefore very tedious. The disease usually lasts for no less than 5 years.
Lichen planus verrucosus presents itself as a nodular to wart-shaped skin disorder: the nodules can occur individually or in small groups and range in size from a few millimeters to 3 centimeters. In individual cases, several nodules can grow together and form warts up to 10 cm in size. The patient feels severe itching, which, among other things, leads to the formation of scars, which is associated with the healing of these nodules.
The therapy is complex and relies primarily on drugs that relieve inflammation and itching, such as glucocorticoids (cortisone). These are either taken orally or injected directly into the subcutaneous tissue at the affected area. External radiation therapy can also be used. Therapy is important because if the lichen planus verrucosus is not treated, it can degenerate into a carcinoma - i.e. there is a risk of skin cancer.
Lichen planus follicularis
Lichen planus follicularis (acuminatus) often occurs on the hairy parts of the body. Characteristic are multiple, conical elevations on the hair follicles. Often they show up in the form of a rash with an unclear border. Usually only mild itching occurs. The scalp is often affected. The formation of the described papules prevents newly growing hair from reaching the surface. As a result, lichen planus follicular hair loss and a pitted bald area can occur.
The diagnosis is made based on clinical signs and microscopy of the area. In terms of differential diagnosis, the doctor differentiates between leucoplacia nicotinica, candiosis, lupus erytehrmatodes, contact allergy and secondary syphilis.
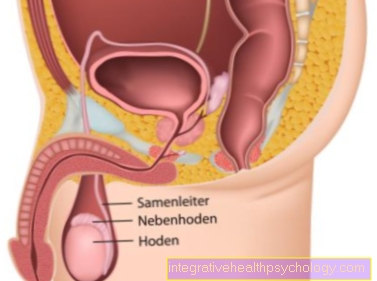
Lichen planus genitalis
Lichen planus can also occur in the genital area. This must be distinguished from a lichen sclerosus et atrophicus. Compared to this, lichen planus in the genital area is less common.
Most of the time, a genital lichen planus is based on a hormonal imbalance. This can happen especially in phases of hormonal changes. For women, this can be the case during pregnancy, for example.
Lichen planopilaris
Lichen planopilaris is a chronic skin condition that can lead to atrophy of the hair follicles and baldness. The cause is still unknown. It is believed that there is a chronic disorder of the cornification of the hair follicle epithelium. The subsequent destructive processes presumably lead to the destruction of the hair follicles and the hair shaft. A loss of cytokeratin 15-positive stem cells was found. The connection to other diseases such as keratosis pilaris, follicullitis decalvans and lichen planus follicularis is unclear.
Lichen planopilaris usually occurs in middle age. Women are affected more often than men. The disease usually manifests itself in the side and front of the head. The back of the head is less affected. The clinical picture is similar to the clinical picture of follicular lichen planus. The extensor sides of the upper arms, the thighs, the oral mucosa and the nails can also be affected. In addition to the visual diagnosis, the microscopic image is used to make the diagnosis.
The different locations
Lichen ruber on the oral mucosa
One of the most common places of manifestation of the lichen planus is the mouth or the oral mucosa. One speaks here of "OLP", the "oral lichen ruber". This is affected in 20-30% of the cases, which is why it is discussed separately in the following: It manifests itself in the reddish colored areas of burning in the oral mucosa are streaked with white. These stripes are also called "Wickham Striae" (for Latin: stripes = striae) after their discoverer Louis F. Wickham. They arise from a widening of the mucous membrane epithelium.
In general, women are more often (approx. Twice as often) affected by the lichen planus of the oral mucosa than men, the age of onset is between 40 and 60 years. In addition to the impressive stripes of the oral mucosa, depending on the definition, five to six different forms of lichen ruber in the mouth are subdivided: the bullous form (with blistering), the erosive form (with skin erosions), the reticular form: the lichen forms a network-like structure on the oral mucosa. Furthermore the atrophic form (with tissue shrinkage), the nodular (papular form), and the plaque-like.
Depending on the form, different differential diagnoses can be considered, but the therapy after a clear diagnosis does not differ. The above-mentioned forms can also occur on all other body mucous membranes.
For more information, read on here: Oral lichen planus.
Lichen ruber on the head / scalp
Another sub-form of lichen planus is manifestation on the scalp or its hair follicles. This form is particularly harmful for the patient, as it is associated with rapidly progressing alopecia (i.e. hair loss). This alopecia is also not naturally reversible after the hair follicles on the scalp have been attacked.
In addition to hair loss, as with the other forms of lichen planus, itching and reddening of the skin also occur. The redness is flat and blurred, so it extends over the entire scalp without a border. The skin becomes scaly to scabby and itchy, the follicular epithelium of the hair cells - i.e. the layer of cells that surrounds the newly growing hair at the root - dies off and the hair falls out.
Therapeutically, a tincture with a strong glucocorticoid can be applied. Injecting the infected areas is also possible, but does not bring too much success. Overall, however, the therapy is difficult and is usually not very successful. Gradients over several years are also absolutely normal with this form. After the disease has healed, large, hairless areas of scarring remain, the follicular epithelial cells of which are destroyed. The only solution for cosmetic correction in this case is a hair transplant.
Early diagnosis is important in order to prevent alopecia as early as possible. However, due to the abundance of differential diagnostic diseases, this is not always easy.
Further topics from this area:

Skin disorders
There are various skin diseases, some of which are harmless, but can also be an expression of a malignant disease. Among other things, color and shape can provide important information about the cause.
Here you get to the topic: Skin diseases

Skin changes
Skin changes such as wrinkling is a natural phenomenon of aging. Other changes in the skin can be an expression of a disease of the skin or other organs.
Here you get to the topic: Skin changes