Lymphedema of the legs
definition
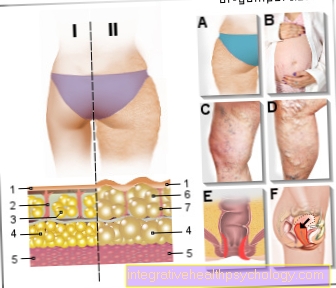
The term "lymphedema" describes a swelling of the connective tissue below the skin, which can be attributed to a build-up of lymphatic fluid.
The lymph fluid transports nutrients and waste materials from the tissue fluid into the venous vessels of the body.
Lymphedema occurs when more lymph fluid accumulates than the lymphatic vessels can transport away.
The causes of lymphedema of the legs can be divided into three groups:
- Obstruction or obstruction of the lymph vessels
- Destruction of the lymph vessels,
- Decrease in size / malposition (hypoplasia) of the lymph vessels;
In the following article you can read why lymphedema develops in heat or during pregnancy: Edema in the leg - these are the causes

There is no cure for leg lymphedema.
In stage 1 it can be transferred to the latency stage through consistent therapeutic measures, a stage in which there is still no swelling despite the damaged lymphatic tract.
If the disease is more advanced, good therapy can be expected to improve, but not to cure it.
Find out all about the topic here: Lymphedema.
Treatment / therapy
Leg lymphedema has four stages.
The stages range from stage 0, the latency stage, to stage 3, elephantiasis.
Treatment can only bring the disease back to the latency stage in stage 1, the phase of soft swelling that can still be pushed away.
In the later stages, therapy is still useful to slow the progression of lymphedema of the legs.
Complex physical decongestive therapy (KPE) is an important therapy method.
This therapy method consists of four important components: manual lymphatic drainage, skin care, compression, movement.
The CPE is not suitable for acute inflammation of the lymphatic vessels, heart failure or malignant lymphoma (cancer of the lymph tissue).
Manual Lymph Drainage (MLD), which is performed with the therapist's hands, works through a combination of compression (pressure), movement and breathing.
This improves the transport capabilities of the damaged lymph vessels and part of the swelling can be reduced and transported away via the lymph vessels.
Good skin care is necessary to prevent inflammation and tearing of the skin.
The compression is intended to prevent further development of the lymphedema after satisfactory decongestion.
Patients are provided with either compression stockings or leg wraps.
Exercise therapy also supports the treatment of leg lymphedema.
For more information about lymphatic drainage and how it works, read our article: Lymph drainage - this is how it works
Which exercises help?
In general, exercise promotes the removal of lymph fluid from the tissue and thus helps to reduce the lymphedema.
It is important that the compression stockings are worn during the movement exercises, because they also support the removal of the lymph.
Quieter sports are well suited: quiet walks, moderate hiking, Nordic walking, cycling and swimming.
The steady movement supports the muscle pump, which promotes the return flow of venous blood to the heart.
This also indirectly improves the return flow of the lymph fluid into the venous vessels.
Special gymnastics exercises that patients can learn during physiotherapeutic treatment and that should also be performed consistently and daily by the patient at home are also very suitable.
The concept of "decongestion gymnastics" is relatively new.
First the lymph nodes are activated by circular, massaging movements and then simple exercises are performed while the compression stockings are worn.
For example, these are: Slow running and conscious rolling of the feet, standing on tiptoe and lowering again, etc.
Homeopathic remedies
Homeopathic recommendations for lymphedema of the legs are, for example:
-
Lycopodium clavatum
-
Gingko biloba
-
Fucus vesiculosus
-
Sodium sulfuricum
Can lymphedema of the legs also be operated on?
The first step in the treatment of lymphedema of the legs is Complex Physical Decongestion Therapy.
Only when this method is no longer sufficient can an operation be considered.
The possible surgical methods have not yet been well researched scientifically and can be divided into three groups:
1. Restoration of the broken lymphatic system by transplanting the body's own lymph vessels to the affected areas,
2. Redirecting the fluid through new connections between lymphatic vessels and veins,
3. Removal of affected tissue (last option).
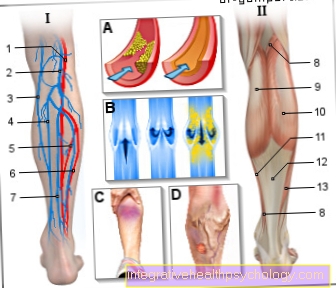
What do compression stockings do?
With the constant pressure on the legs, compression stockings promote the venous return of the blood towards the heart and thus the return of lymphatic fluid into the veins.
Compression stockings for lymphedema of the legs should only be worn when the lymphedema has already significantly decreased due to manual lymphatic drainage, since the stockings themselves cannot improve the lymphedema, but stabilize the status quo.
Compression stockings with lymphedema of the legs must not be worn in severe peripheral arterial occlusive disease (PAD) if the ankle pressure is below 80mmHg.
These are the causes
The causes of lymphedema of the legs are also divided into primary and secondary.
Primary lymphedema is when the lymphedema of the legs is not explained by other diseases, but is a disease of its own.
The cause here are congenital malformations of the lymphatic system.
In most cases, women are affected and the disease is diagnosed by the age of 17.
Primary lymphedema begins in the feet and spreads along the leg.
In around 10% of cases, the primary lymphedema of the legs is due to a hereditary disease (e.g. Nonne-Milroy syndrome).
The majority of patients with lymphedema of the legs, however, suffer from what is known as secondary lymphedema, which is due to another disease.
Possible reasons are tumors, operations, accidents, inflammation of the lymph vessels, radiation therapy and congestion in the venous system.
This lymphedema of the legs is often one-sided and spreads “from top to bottom”, as the lymph fluid first accumulates where the lymph vessels have been destroyed or obstructed and then backs up towards the feet.
The causes for the development of edema in general can be found in the following article: Causes of Edema
Concomitant symptoms
The main symptom of lymphedema of the legs is swelling caused by the accumulated lymphatic fluid.
- Stage 0, latency stage: legs are not yet swollen, although the lymph vessels are already damaged.
- Stage 1: There is a slight, compressible swelling that does not yet cause pain.
Lymphedema of the legs can also be felt by pressing shoes or cutting socks, and trousers may no longer fit properly or cut in.
The symptoms of lymphedema are more pronounced in warm temperatures, and women often report that the symptoms are worse with menstruation. - From stage 2: Later, when the swelling is very severe, affected patients also suffer from pain in the legs and feet.
An accompanying symptom of lymphedema of the legs are the so-called box toes, as the toes become rectangular due to the swelling. It is also typical that with lymphedema of the legs it is difficult or impossible to lift the folds of skin over the toes.
In the course of the disease, other accompanying symptoms of lymphedema develop: The skin is tight and causes an uncomfortable feeling, the patients complain of heavy and stiff legs.
The skin color changes and the affected areas become darker.
In addition, the texture of the skin changes: It becomes firmer and coarser.
- Stage 3, final stage: The swelling is completely hardened and the leg is misshapen, which is known as elephantiasis.
Swelling of the legs can include also induce thrombosis. Read more about this and other causes of swollen legs at:
Swollen legs - causes & therapy
When does pain occur?
At the beginning of the disease there is usually no pain with lymphedema of the legs, the legs are only slightly swollen in the early stages (stage 0 and stage 1) and the swelling can be pushed away.
As the disease progresses, the swelling continues to increase, the skin feeling tense and the feeling of very heavy legs are the result.
The lymphedema of the legs is actually not painful, but these sensations can be perceived as painful.
The pressing pain caused by lymphedema of the legs can usually be successfully relieved by lymphedema therapy.
It is important to start treatment early and to use regular therapy to prevent the pain from worsening.
If pain occurs with a known lymphedema, this can be an indication of an inflammation of the lymphedema (erysipelas, wound rose).
How is leg lymphedema diagnosed?
Leg swelling can have a number of causes.
The diagnosis of "lymphedema of the legs" can be made through a medical consultation (anamnesis) and a physical examination of the legs.
With lymphedema of the legs, the toes are also swollen and appear as "box toes" due to the accumulation of lymph fluid in the tissue.
It is then no longer possible to lift a fold of skin over the toes, which is known as the positive "Stemmer sign".
In addition, clear transverse folds form on the toes, and the skin surface of the affected area becomes rough.
Due to these characteristic features, the diagnosis “lymphedema of the legs” is easy to make and a clear differentiation from venous edema is possible.
Lymphedema of the legs after an operation
Lymphedema of the legs can occur after operations in which the lymph nodes and lymph vessels in the abdomen had to be removed.
These lymph nodes are namely the drainage points for the lymph fluid from the legs.
If they are injured or removed, the lymph backs up in the legs and secondary lymphedema of the legs develops.
Most of these lymph nodes are removed as part of cancer surgery, such as ovarian or cervical cancer.
What is understood by the rose / lymphangitis?
The wound rose (medical erysipelas) is an infectious disease that spreads via the lymphatic system.
The infectious agents, mostly bacteria of the genus Streptococcus, can penetrate the body through the smallest injuries to the skin.
There they trigger inflammation and spread via the lymphatic system.
Affected areas of the body are painfully swollen, overheated and reddened.
Lymphedema of the legs promotes the development of a sore rose.
Treatment is with antibiotics.
If the rose is discovered too late or not treated, blood poisoning with fever and chills can result.