rubella
Synonyms in the broadest sense
Rubella, rubella infection, rubella virus, rubella rash, rubella rash
English:
German measles, Rubella
Epidemiology / Occurrence
The virus, which is widespread worldwide, is transmitted via the air (= airborne) by droplets, e.g. when coughing, sneezing or through direct saliva contact while kissing.
Rubella is a so-called "childhood disease", but it can be observed that due to the insufficient vaccination of the population, the age peak of the disease is shifting into adolescence and adulthood.
In about 50% of cases, the patients show no clinical signs (physical characteristics) of rubella infection, such as the characteristic rubella rash (= skin appearance, rash), which is why in these cases one speaks of a subclinical course of the infectious disease.

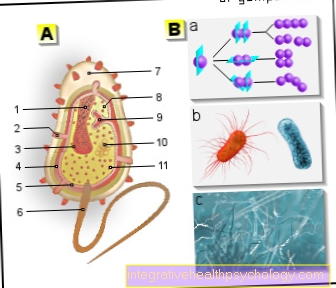
infection
The infection takes place via a so-called Droplet infection. It means that when sneezing or coughing finest droplets are ejected. The infectious rubella viruses sit in these droplets and are thus transmitted from one person to another.
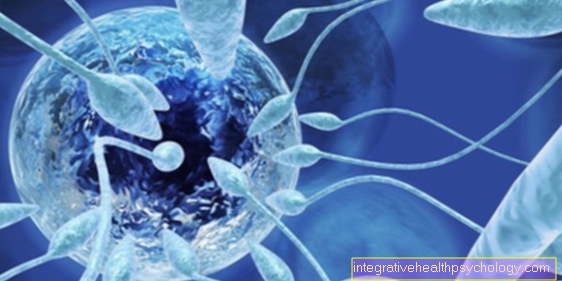
The Transmission from the mother via the placenta on the unborn child. Unfortunately, the placenta does not represent a barrier for the rubella virus, which thus spreads unhindered via the blood to the embryo or fetus. Up to the 10th week of pregnancy, there is an infection and a dramatic course in 50% of cases. Between the 10th and 17th, 10-20% of the time. Only after the 18th week of pregnancy is there only a low risk of infection and the extent of the complications is less pronounced.
The Risk of contagion consists about a week before and a weeke after the rash appears. Children infected during pregnancy can be contagious for up to a year. Overall, however, the actual number of transmissions and infections cannot be assessed as very high.
Risk of contagion
The risk of infection begins about a week before the outbreak of Skin manifestations and ends Further seven days after its occurrence.
Cause / origin
The virus enters the body through the mucous membranes of the respiratory tract, reaches the Lymph nodes of the head and neck area and multiplies there.
In response to the body's response to the virus replicating, the lymph nodes may become swollen and painful. Lymph node swelling occurs about five to six days after the virus enters the body.
After another 10 days, the viruses are in the blood circulation Circulatory system to skin been transported and call there the typical of rubella disease Exanthema (rash) on. This lasts for four to five days.
The infected person excretes the rubella virus via the secretion of the nasopharynx, with the exhaled air, urine and stool.
Read more of the causes of one here: Rash
Pathogen
This is what causes rubella Rubella virus. It is an RNA virus from the genus Togaviridae. The rubella virus is coming only in humans in front. Man is thus the only host.
The rubella virus, like the measles, mumps, or chickenpox virus, causes one typical childhood illness.
Symptoms
Before the rash occurs (= exanthema), flu-like symptoms such as fever, limb pain, headache or sensitivity to light are possible.
The rash is light red and small spots, whereby the individual skin symptoms do not merge into one another (= non-confluent exanthema). It usually begins behind the ears and spreads from here over the trunk of the body, arms and legs.
The body temperature is only moderately, if at all, increased in the course of the disease.
Elderly patients with rubella, i.e. Adolescents and adults are often affected by a temporary joint inflammation (= arthritis) with painful movement restrictions.
See on this subject also Adult rubella
In most cases, the rubella sufferer will recover within a few days after the rash occurs.
Characteristics of rubella
Characteristic of rubella infection are the skin rash and swollen lymph nodes at the neck, in the neck and behind the ears;
Rubella in babies - what are the special features?
The Newborn has one in the first few weeks of life certain nest protection against rubella by the mother's antibodiesin case the mother had rubella disease in childhood or who received two rubella vaccinations. However, this protection evaporated quickly, so that the two rubella vaccinations are more than recommended.
The rubella infection initially proceeds as in older children. There is an easy one Impairment of the general condition. The baby is limp and drinking behavior is usually reduced. The nose runs and the eyes are common reddened in the sense of conjunctivitis. There are also other unspecific complaints such as Headache and body aches and a Swelling of the lymph nodes around the neck and behind the ears. The temperature can reach a maximum of 38 ° C, in some cases even higher.
A few days after this unspecific feeling of illness, the typical rash on. This impresses bright red, easily distinguishable from each other, small to medium spots. At first they can be seen behind the ears or on the head and then spread to the trunk of the body, as well as arms and legs. Within three days but the rash is again disappeared.
Rubella embryopathy or rubella fetopathy are a specialty of babies:
- In the Rubella embryopathy the infection occurs as early as the first trimester of pregnancy, when the mother falls ill with rubella if the protection is inadequate and the unborn child is affected. At the beginning of pregnancy, complications occur in up to 90% of cases. Often there is a termination of pregnancy, an intellectual disability or the so-called Gregg triad. This consists of one Inner ear numbness, one grey star and various heart defects. The degree of severity varies depending on the week of pregnancy in which the infection took place.
- In the Rubella fetopathy the infection occurs after the first trimester of pregnancy. Here in the baby there can be one Inflammation of the liver (hepatitis) or one Enlargement of the spleen (splenomegaly) come. Furthermore are Changes in blood countsuch as anemia (haemolytic anemia) or a drop in blood platelets (thrombocytopenia).
Rubella in adults - what are the special features?
Since rubella is a typical childhood disease, rubella only occurs in adults Rare in front. However, unvaccinated adults are just as likely to be infected as children.
A particular danger exists for the Unborn unvaccinated pregnant womenwho become infected with rubella.
Rubella in adults run away as is the case with children unspecific. At first there are classic Symptoms of a cold like runny nose, headache and body aches and slightly elevated temperatures. In half of the cases, the rubella infection is over. The other half of those affected get other symptoms, like one Swelling of the lymph nodes or the typical fine-spotted rashwhich spreads from the head (usually behind the ears) to the body.
They occur more often in adults than in children certain complications on. Overall, however, these are still very rare. This includes Joint pain (arthralgia) and Inflammation of the joints (arthritis)which, however, can also be observed in older children. There are also cases in which it spreads to the lower airways in the sense of a bronchitis comes. A spread to that Brain (encephalitis) and on the Pericardium or the heart muscle are also possible.
diagnosis
The clinical symptoms are often not characteristic of rubella disease. Since detecting the virus itself is difficult, take one Rubella antibody detection in front:
are IgM antibodies (see also: immune system) against the rubella virus is present in the blood, this indicates a current Rubella infection, but is Not proving that the IgM antibody concentration can also be increased by other viral diseases or can be increased for a long time after an infection has passed and has subsided (up to a year after the rubella disease).
To confirm or exclude rubella disease, two blood samples should be taken every 14 days and a test for IgG antibodies against rubella should be carried out.
This procedure is mainly used during pregnancy:
If the unborn child is suspected of having rubella infection, two blood samples are taken to determine the IgG concentration (= IgG titer determination).
If the mother is immune to the virus on the basis of the determined values, infection of the unborn child is excluded.
An invasive method is required to detect rubella infection in children:
By means of amniotic fluid puncture and examinations or a child's blood sample in the mother's womb, the detection of the presence of nucleic acid (genetic material of the virus) of the virus can be made in the child.
vaccination
The vaccination recommendations in Germany are based on the Standing Vaccination Commission STIKO. This recommends:
- The first rubella vaccination already in the first 11 to 14 months of age perform.
- The second rubella vaccination should then be in second year of life between the 15th and 23rd month of life.
Since rubella is a typical childhood disease, the early vaccination time is not surprising. The second vaccination is not to be regarded as a booster. After the first vaccination, around 90-95% of those vaccinated have adequate protection against rubella. The remaining percent, which only acquired insufficient protection after the first vaccination, should be achieved through the second vaccination. The second vaccination therefore serves to compensate for possible vaccination failures.
A refreshing after several years, as is known from other vaccinations, is the rubella vaccination unnecessary. If the rubella vaccination was missed in childhood, it can and should be done at any time in adulthood. This recommendation applies to all adults with an unclear vaccination status, with none or only one of the two vaccinations. Women of childbearing age should pay particular attention to adequate vaccination against rubella, as infection during pregnancy can have serious consequences for the unborn child.
Adults can get rubella just like children and thus endanger their environment. Unvaccinated children and pregnant women are particularly at risk from this. A catch-up vaccination should be given even if an adult had a supposed rubella infection in childhood. Since rubella cannot always be clearly differentiated from other childhood diseases, it is not possible to say with absolute certainty who really had the rubella. In some cases, even with a real rubella disease, it seems possible that it can be infected again at a later point in time.
Unfortunately, there is no longer any possibility of getting the vaccination during pregnancy. The rubella vaccine is a so-called Live vaccine and may not with existing pregnancy be injected. Such a vaccination increases the risk of malformations in the unborn child. Unvaccinated pregnant women should therefore avoid community facilities or events where there are many children who are potentially at risk of infection. Only in the Lactation it is possible to catch up with the rubella vaccination again.
vaccine
The rubella vaccine is a live vaccine. This is produced from weakened rubella virus. Usually the first vaccination is given in combination with measles and mumps as an MMR vaccination.
The name of this combination vaccination has a different name depending on the manufacturer. Three typical examples are M-M-RVAXPRO®, MMR-Priorix® or simply Priorix®. The price for the Priorix® vaccine is around € 30. The vaccination by the doctor will then be charged again separately.
In the second vaccination, the vaccine against chickenpox (varicella) is added as an MMRV vaccination. This vaccination is then e.g. Priorix Tetra®. The costs for this are around € 70. Protection against multiple diseases can be achieved with one syringe.
Since the rubella vaccination follows the STIKO recommendation, the costs of the vaccination are covered by the health insurance in almost all cases. If one is exposed to an increased risk of rubella infection through one's job, the employer must bear the costs of the vaccination in accordance with the Ordinance on Occupational Health Care (ArbMedVV). These include e.g. Institutions for the examination, therapy and care of children, but also research institutions and laboratories with the possibility of contact with infected samples.
Titer determination
The Titer determination for rubella plays a major role Pregnant women an important role:
- A high titer speaks for one adequate protection for the unborn child during pregnancy.
- At a low titer exists one Danger for the unborn child, when the mother gets rubella.
Protection can be assumed at a titer of over 1:32. There are certain in the blood IgG antibodies intended against rubella, which allows a statement to be made about the immune system. If the titer is too low, there is the possibility of passive immunization up to the 18th week of pregnancy within five (better three) days after contact with rubella. Passive immunization means that the body is supplied with IgG antibodies from outside and does not have to produce them itself (as would be the case with active immunization). Passive immunization reduces transmission to the child and, in the best case, completely prevents it.
A Catch up the vaccination against rubella is unfortunately at the time of Pregnancy no longer possible. The live vaccination creates the risk of malformations.
incubation period
The Time from contagion with rubella until the outbreak the rubella is on average 14-21 days.
In 50% of the cases however, the disease progresses asymptomatic and does not even appear.
Reporting requirement
The disease and death of a child from rubella embryopathy is notifiable.
Differential diagnosis / exclusion diseases
Rubella disease must be differentiated from other diseases that also lead to a reddish rash. These include the measles, the Three-day fever (= Erythema subitum) and the Ringlet rubella (= Erythema infectiosum).
In addition, it is necessary to distinguish between diseases associated with swelling of the lymph nodes. You have to think of the following diseases: Pfeiffer's glandular fever (= infectious mononucleosis) or a Cytomegaly infection.
Rubella embryopathy must be differentiated from other, prenatal (= intrauterine) infections. Infections of the child before birth can e.g. caused by toxoplasma, varicella / chickenpox virus, listeria or the cytomegalovirus.
Treatment / therapy of rubella
A Therapy of the causei.e. a treatment for the virus, is not possible. Since rubella is a typical childhood viral disease, it can only be treated symptomatically with a lot of patience.
An antibiotic, on the other hand, does not fight the viruses. A antibiotic is only used if by one additional bacterial infection is to go out. Symptomatic measures include e.g. antipyretic agentsthat relieve headache and limb pain at the same time. Some children respond better to ibuprofen, while others respond better to paracetamol. These medications can also be given alternately in order to get a "fever" under control.
Measures like leg wraps can also help. The children are often better off just by lowering the fever (antipyresis). If the fever persists for three days, a pediatrician should be consulted for further clarification. Adequate hydration is essential, especially for babies. If the drinking behavior is greatly reduced, an infusion system may be necessary in the hospital. With rubella, however, the children are usually not severely affected and handling at home is possible. Adults also need to be patient, drink a lot and, if necessary, take measures to reduce fever or to relieve pain.
Children with a congenital (in the womb / during the birth acquired) rubella infection must be comprehensively cared for and their development encouraged.
Complications
Complications are very rare and, if they occur, consist of a persistent, chronic joint inflammation or inflammation of the brain that occurs much later than progressive rubella panencephalitis is called, so an encephalitis that is caused by the rubella virus and the whole brain concerns.
Is a pregnant woman suffering from rubella who is not immune to the rubella virus (p. immune system), the risk of infection for the unborn child varies depending on the stage of pregnancy:
Rubella During Pregnancy
The earlier the infection occurs in pregnancy, the more likely it is that proper organ development will be impaired in the child.
At a maternal rubella infection In the 2nd to 6th week of pregnancy over 60% of the children are harmed, in the 13th to 17th week of pregnancy this percentage drops to 10%.
After the 4th month of pregnancy rubella disease in the mother does not lead to child damage more often than in pregnancies without rubella infection.
Congenital rubella is when the child was infected with the virus in the womb. This takes place via the placenta (placenta): The rubella virus enters the mother's nasopharynx, multiplies in the local lymph nodes of the upper respiratory tract and finally gets into the blood. During pregnancy, the child can become infected with the virus via the placenta.
Approx. 100 newborn children suffer damage from maternal rubella infection each year; one speaks of the Rubella embryopathywhen the child's development in the womb is impaired by the viral infection. The Gregg Syndrome describes typical developmental disorders or organ damage in prenatally infected children and is made up of the following points:
- deafness
- Lens opacity (= cataract, cataract)
- Heart defect
Also are Developmental disorders of a general nature such as low birth weight or growth retardation are common. It can also lead to damage and incorrect systems central nervous system, the Ears, eyes and come to the internal organs.
Rubella in early pregnancy
If the rubella infection has been detected during pregnancy, the doctor can carry out an interruption of pregnancy up to the 4th month of pregnancy as a permissible medical measure, as serious damage to the child can be assumed.
Prognosis and course
The rubella progression in children, adolescents and adults is usually mild and without complications.
A child with congenital rubella, however, has a poor prognosis and is impaired in its development by the damage to its organs.
prophylaxis
The prophylaxis (prevention) of rubella is of crucial importance, because through the Vaccination against rubella complications and damage to the unborn child can be effectively prevented.
All children, girls and boys, should twice be vaccinated against rubella, as the boys, as carriers of the disease, can infect the girls or women.
The vaccination against rubella is recommended from the age of 15 months and the second vaccination can follow the first at an interval of four weeks.
The simultaneous vaccination with a combination vaccine against is recommended measles, mumps and rubellaEach vaccination can also be done individually. The vaccine against the rubella virus is a so-called Live vaccine:
During its production, rubella viruses are weakened in their effect and the ability to multiply is switched off. When the body comes into contact with the weakened form of the virus, the Immune systemby which the vaccinated person becomes immune to the viruses, i.e. if you come into contact with the virus again, the disease does not occur.
The vaccination has a high rate of effectiveness, 95% of all vaccinated people are immune to rubella virus infection. The vaccination protection lasts for 15-30 years.
5-10% of those vaccinated can develop one within 5-7 days Vaccination reaction come in the form of a fever and a small speckled rash.
Also one Vaccination in adulthood is possible, there are two prerequisites for this in women: there must be no pregnancy at the time of the vaccination and pregnancy must be excluded in the two cycles following the vaccination, as the vaccination causes damage to the unborn child. Women of childbearing age should be immunized against rubella and if they are not vaccinated against rubella in front ensure pregnancy through vaccination.
In adults, joint pain may occur after the rubella vaccination.
The following people must not be vaccinated with the rubella vaccine:
People who take drugs that suppress the immune response (= immunosuppressive therapy); People with weak immune systems (e.g. AIDS); if you are allergic to egg white, because the vaccine contains such components from egg white and pregnant women.
Passive immunization
The administration of protective antibodies in the form of immunoglobulins (= passive immunization) within 72 hours does not reliably protect the child against infection if the mother who is not immune to the rubella virus has come into contact with the virus.





















.jpg)





