Reflux
synonym
GERD (Gastroesophageal reflux disease), Reflux disease
definition
- Gastroesophageal reflux: Backflow of stomach contents into the esophagus due to incomplete closure of the sphincter muscle at the stomach entrance.
- Physiological reflux: is a reflux of stomach contents that occasionally occurs in healthy people when they eat high-fat meals and wine.
- Gastroesophageal reflux disease: This disease shows changes in the lining of the esophagus due to constant reflux (Esophagus).

Disease incidence
In the western population there are approx 20% affected by reflux disease 60% no mucosal changes in the endoscopic examination. However, 40% already have visible changes. 5% of people with a GERD develop a so-called in the course of their lives Beret esophagus, with these develops in 10% of the cases Esophageal cancer.
causes
One cause of the Reflux It is possible that the lower esophageal sphincter does not close properly and that the gastric juice flows back into the esophagus. This is also the most common cause of reflux disease. Another cause can be pregnancy, as in about 50% of all expectant mothers especially im last trimester of pregnancy Reflux occurs.
Other reasons for reflux can be: Condition after surgical treatment of a Achalasia (this is a muscular constriction of the lower esophagus due to a nerve malformation), a narrowing of the stomach outlet, or sceroderma (a hardening of the connective tissue skin or internal organs).
Pathogenesis
An inadequate antireflux barrier of the lower Esophageal muscle (also unterer Ösophagussphinkter, or LES for short), which is located between the stomach entrance and the lower esophagus, is one of the main causes of gastroesophageal reflux disease. In the healthy the lower forms UÖS a pressure barrier, the pressure in the esophagus at rest approximately 10-25 mmHg higher than im stomach. Only during the act of swallowing does the LES relax for a short time.
In the patient there is an inadequate relaxation of the lower esophageal sphincter muscle outside the act of swallowing, or the pressure is too low, so that no pressure barrier can be built up. Other factors for one of the inadequate antireflux barrier can be Obesity, late large evening meals, alcohol and Coffee enjoyment. The second major cause of GERD is what is known as aggressive reflux. This is an acid reflux of gastric juice.
Symptoms

In two thirds of all patients, the main symptom is heartburn, a burning pain behind the sternum that occurs especially after meals, at night and when lying down. A feeling of pressure behind the breastbone can also occur. In 60% of the patients there is belching of air, in half of the patients there is difficulty swallowing.
Soapy or salty taste after belching can occur as well as nausea and vomiting. All the symptoms are aggravated by pressing, lying on your back, bending over, physical exertion, certain foods and medicines, and also by stress. Chronic cough, possibly hoarseness or nocturnal sleep disorders can be a sign of a "Extra-esophageal manifestation“ (Above the esophagus manifestation) of reflux disease.
Read more on the topic: Burning behind the breastbone.
with the baby / child
Occasional reflux is just as normal and harmless in babies and children as it is in adults. Only if the reflux leads to further abnormalities or complications does it require treatment. The symptoms of pathological reflux are often symptoms of failure to thrive. The children are noticeable with insufficient weight gain or growth that is not age-appropriate. Accompanying this, increased vomiting or refusal to eat can often be observed (you can find more here Causes of vomiting).
Reactive respiratory diseases, such as asthma (here it goes Symptoms of asthma), but can also trigger reflux.
The physical cause of reflux is the same as in adults. The lower sphincter on the esophagus contracts incorrectly, and as a result, stomach acid can travel up the esophagus. In children, this phenomenon is caused by a hernia in the diaphragm in up to 80% of cases. The esophagus usually enters the abdomen through a small opening in the diaphragm. There it flows into the stomach. This is fixed in the abdomen due to its larger volume and cannot pass through this narrow point. In addition, the esophageal sphincter is located directly under the constriction and can therefore control the passage of food towards the stomach. However, if the point of passage is enlarged, parts of the stomach, anatomically speaking, may get into the chest cavity. The sphincter loses its hold just below the diaphragm and the pressure in the stomach can exceed its muscle strength. Reflux is the result.
A much rarer cause is a congenital malformation of the esophagus, which had to be corrected surgically. Any operation on the esophagus can result in reflux. The treatment of reflux in very young children is often conservative in order to avoid the side effects of medication. Elevation of the upper body during and after meals and the administration of locust bean gum should therefore be attempted for at least six months. If there is no improvement, drug therapy or, if necessary, surgical treatment can then be considered.
Complications
Ulcer in the esophagus, Bleeding, Swallow from Stomach contents above all At night, beret esophagus (Berett Syndrome), Difficulty swallowing due to narrowing of the esophagus.
Due to the loss of blood, a Iron deficiency anemia occur. Anemia is sometimes the first symptom why patients see a doctor in the first place. At the Beret esophagus there is a transformation (metaplasia) of the epithelium of the esophagus. This syndrome is considered to be Precancer (Precancerous disease), which is why patients with this disease should have a medical check every 3-5 years whether a cancer originated.
bronchial asthma and the Reflux disease are closely related, namely a connection between the two can often be established, namely at around 30% or more. How exactly this relationship exists has not yet been clarified. One theory is that the reflux of gastric juice also enters the Bronchi of the lung and irritates it strongly. Another assumption is that the acidity of gastric juice is tenth Cranial nerve, Vagus nerve, irritates, which results in a narrowing of the bronchi. In the course of a reflux disease, a dentist should be consulted, as it is easier to injure the Enamel can come.
Reflux esophagitis
Inflammation of the esophagus can occur as a result of reflux and can be explained by the anatomical conditions in the esophagus and stomach. The esophagus is made up of a different type of mucous membrane than the stomach. In the esophagus there is a so-called "squamous epithelium". It is described in a purely striking way as a simple layer that only passes on food pulp and has no other functions.
The stomach, in turn, contains a so-called "columnar epithelium". This mucous membrane has the ability to protect itself from stomach acid by producing a protective film. If gastric acid gets into the esophagus as part of reflux, the epithelium located there cannot protect itself from the acid in the accumulated food pulp. The result is that its surface is irritated by the acid. The structure of the mucous membrane is lost with increased contact and inflammation of the affected areas occurs. This process manifests itself symptomatically in heartburn through to pain during and after ingestion. The inflammation will only be able to recede if renewed contact with gastric acid is prevented.
Read more on the subject at: Reflux esophagitis
Laryngitis
The development of a laryngitis is rarely observed in reflux. However, it is quite possible with severe reflux. To do this, however, the partially digested food must reach the throat area. The epiglottis is anatomically located between the throat and the windpipe. In the case of reflux, this means that those affected feel the rise of the thickened food pulp in the form of severe heartburn in the throat area and a simultaneous feeling of regurgitation. This means that the food can sometimes get back into the mouth and mimic a weakened vomiting.
The lining of the larynx can then be irritated by the stomach acid. With increased contact, the surface structure of the mucous membrane can then be increasingly attacked, which results in inflammation. For those affected, this manifests itself in a burning sensation when swallowing or breathing. Furthermore, pain in the throat area when swallowing food is typical. The voice is not affected by a pure inflammation of the epiglottis. However, if stomach acid gets past the epiglottis into the windpipe, as if swallowed, it can also attack the vocal cords. Those affected might then notice hoarseness as a further symptom.
Inflammation of the stomach lining
Reflux often occurs in combination with inflammation of the stomach lining. However, it is important to know that they do not have to be present at the same time. Rather, they are to be viewed as two independent clinical pictures that can influence one another. An increased production of gastric acid can destroy the protective film over the stomach lining. The result is irritation of the mucous membrane, which can become inflamed with prolonged contact. If the inflammation continues, a painful ulcer can develop.
However, the inflammation of the lining of the stomach does not lead to dysfunction of the lower esophageal sphincter. This requires other factors such as a diaphragmatic hernia to be present. However, if there is an abnormal closing mechanism, the increased production of gastric acid can aggravate an existing reflux. Symptoms such as heartburn or painful food intake are exacerbated as more stomach acid can get into the esophagus. The dangerous thing about the combination of these two diseases is that the increased production of stomach acid can mean more damage to the esophagus. The stronger the inflammatory reaction in the esophagus, the more the mucous membrane tends to lose its actual cell structure. The conversion process therefore carries the risk of degeneration, which in the worst case can lead to cancer.
Diagnosis
An anamnesis, so a Initial meeting, the corresponding clinical symptoms and the initial use of a certain drug for a probationary period are often the first diagnostic steps of the attending physician.
The real diagnosis is made by a Gastroscopy (Endoscopy). On the basis of the endoscopically determined tissue disorder, the reflux esophagitis, which Esophagitis, divide into three classifications. The classification according to Savary and Miller:
- 0. There is a backflow of gastric juice, but without changes to the mucous membranes.
- 1. Unrelated changes in the mucous membrane, either only red spots exist or white evidence is deposited in the middle of the red spots.
- 2. Spreading spots along the folds of the mucous membrane.
- 3. Here the lesion (the damage) the entire circumference of the lower esophagus.
- 4. Is the complication stage. Ulcerations, strictures (severe narrowing of the esophagus) and the beret esophagus occur.
Another classification is that MUSE - classification to mention after Armstrong. The word stands for metaplasia, ulcer, stricture and erosion. It divides all four into four degrees of severity:
- from 0 = missing;
- 1 = slightly;
- 2 = moderate;
- to 3 = severe.
The third division of reflux esophagitis is the Los Angeles classification. A distinction is made between four stages from A to D.
- Stage A: the changes in the mucous membrane (erosions) have a diameter smaller than 5mm and are located between the individual folds of the mucous membrane.
- Stage B: here the changes in the mucous membranes are greater than 5mm.
- Stage C: the erosions are connected to one another via the folds of the mucous membrane. However, the defects cover less than 75% of the circumference of the esophagus.
- Stage D: is very similar to stage C, except that the defects affect more than 75% of the esophageal circumference. Another diagnostic step is 24-hour pH metry. The acidic stomach contents are passed through the 24 hours using a thin nose outgoing probe.
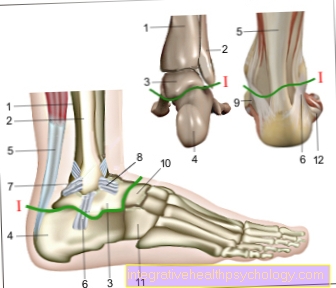
surgery
The principle of any reflux operation is to improve the function of the lower esophageal sphincter. There are various technical procedures that vary depending on the clinic and the expertise of the surgeon. The most common surgery uses part of the stomach to strengthen the lower sphincter muscle. To do this, it is placed around the esophagus as a cuff and fixed to it. This procedure is the "Nissen fundoplication". The sheath of the esophagus is 360 ° and thus completely encloses the esophagus.
Alternative procedures only sheath the esophagus in 180 ° or 270 °. The advantage of this operation is that no foreign material is introduced into the body. Other procedures do this without changing the shape of the stomach. To do this, bands or rings are placed around the esophagus. However, they are the same in their operating principle. Which operation is the best or the right one must be decided individually, depending on which procedure is suitable for the physical circumstances and wishes of the patient.
Reflux ring
A reflux ring is a magnetic ring placed around the lower sphincter muscle of the esophagus, which supports or even completely replaces the physiological function of the sphincter muscle. Visually, the ring can be imagined as a band of many magnetic beads that can be detached from each other when pulled or pushed. In the body, this means that when food is ingested, the ring in the lumen of the esophagus can widen when the food is weighted, so that the food can pass into the stomach. However, once it has passed its structure, the attraction of the magnets is again greater than the pressure in the lumen of the empty esophagus and the ring contracts again.
The effect is that the stomach is optimally sealed off from the esophagus whenever there is no food or fluid intake.The challenge with this procedure is to determine the adequate attraction of the magnets and the optimal diameter of the ring for the person concerned. A ring that is too wide does not seal the esophagus sufficiently, while a ring that is too narrow can seriously impede a passage in the form of swallowing disorders. In addition, the ring is a foreign body that can potentially trigger an intolerance reaction in the body. The advantage, however, after a successful operation is that the person concerned no longer has to take medication for the reflux and the stomach is kept in its original shape.