Sacroiliitis
definition
As Sacroiliitis is called inflammatory changes, the the Sacroiliac joint, so the joint between Sacrum and Iliac bone at the bottom of the Spine, affect. This inflammation is chronically progressive and pronounced painful.

causes
Sacroiliitis is extremely rare as a single disease. As a rule, it is a secondary disease or complication of an existing underlying disease. Diseases that are often associated with sacroiliitis are many rheumatic diseases, such as
- the ankylosing spondylitis
- Reiter's disease (or reactive arthritis in general)
- Behçet's disease
and - psoriatic arthritis.
Chronic inflammatory bowel diseases (Crohn's disease and ulcerative colitis) are also regularly associated with sacroiliitis.
It has not yet been clarified which factors must ultimately be present for sacroiliitis to occur. As for most of the diseases mentioned above, it is noticeable that there is an accumulation of the HLA-B27 protein complex among those affected. Thus there is a genetic disposition.
Signs
The first signs of sacroiliitis are usually pain in the lower back or buttocks. In general, such complaints are very common and sacroiliitis is only the cause in rare cases. However, in contrast to most other causes of pain, typical signs of this disease are that the symptoms mainly appear at night and in the early hours of the morning. On the other hand, after getting out of bed and when moving, the symptoms improve. Since most back pain is triggered or exacerbated by exercise, this is another sign of sacroiliitis.
A radiation of the pain in the thigh is also possible, but no specific sign of the disease. In the further course, signs such as pain when sitting, running, climbing stairs or standing for long periods of time may appear. If signs of sacroiliitis are noticed, a doctor should be seen so that they can investigate any suspicion of the disease.
Symptoms
The leading symptom of sacroiliitis is the inflammatory lower back or buttock painthat classically either only at night or In the morning occurs or at least becomes less severe during the day. Typically there is a Knocking pain or one Displacement pain over the changed sacroiliac joints. In some patients, the pain radiates into the Thigh out. There is also one Stiffness the affected region, which has been removed using Move can improve.
One-sided (right / left)
Unilateral sacroiliitis is the exception. However, it can happen that initially only the left or the right side is affected and then the opposite side becomes infected as well. In addition, the sacroiliitis can be more pronounced on the left or right, so that there are more symptoms on the corresponding side. If the symptoms are strictly one-sided, the diagnosis of sacroiliitis should be reconsidered. Often there is another cause of the complaints such as irritation of the sciatic nerve or a herniated disc.
On both sides
The sacrum (Sacrum) is connected to the iliac bones on the right and left by the less flexible sacroiliac joint. Sacroiliitis typically affects both sides. However, one side can be affected more than the other, so that the symptoms are accordingly more pronounced on the respective side.
Diagnosis of sacroiliitis
In order to diagnose sacroiliitis, the first step is to collect the medical history (anamnese) important. This is followed by a clinical exam to check the amount of motion in the lower spine. There are also some tests that make the presence of sacroiliitis very likely. This includes the attempt to climb a chair and a positive Mennell's sign: The patient lying on his side bends the leg lying below maximally, while the other is retroflexed (bent backwards). This triggers the typical lower back pain in sacroiliitis.
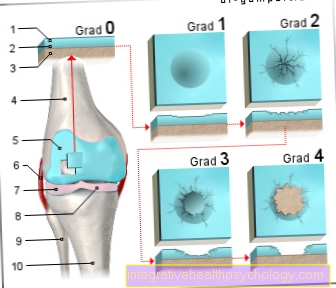
The diagnosis is confirmed by imaging procedures. With an X-ray, sacroiliitis can be divided into a grade of 1 to 4 using the New York criteria.
- In first-degree sacroiliitis there are suspicious changes
- in grade two there are circumscribed erosions and / or subchondral sclerosis, although the joint space is still normally wide.
- If it is grade three, there are clear erosions or sclerosings and the joint space is either enlarged or narrowed. In addition, ankylosis buds may already be present here.
- The fourth degree sacroiliitis is characterized by ankylosis, that is, a stiffening of the joint.
In the X-ray, however, changes can only be detected after an average of eight years of illness. Magnetic resonance imaging (MRI of the sacroiliac joint or MRI of the lumbar spine) allows an earlier diagnosis.
The MRI of the lumbar spine / pelvis definitely shows the inflammation of the ISG. The state of the joint (SI joint arthrosis) can also be reliably shown by the MRI of the lumbar spine / pelvis.
If sacroiliitis is diagnosed without any of the above-mentioned underlying diseases being known beforehand, further diagnostics should be carried out in order not to overlook these sometimes serious diseases and to be able to treat them quickly.
Important differential diagnoses are:
- osteoporosis
- Herniated discs of the lumbar spine
and - Spinal problems caused by tumors
Tuberculous or bacterial inflammation of the spine can occasionally cause symptoms that resemble those of sacroiliitis.
MRI of the pelvis
In some cases, if sacroiliitis is suspected of being present, MRI imaging (Magnetic resonance imaging). However, every diagnosis starts with a physical examination and a medical consultation. If, for example, abnormalities arise during the so-called attempt to climb a chair or the Mennell's sign, the suspicion of sacroiliitis should be clarified. However, the standard procedure is a conventional X-ray of the sacroiliac joints. Depending on the result, an MRI of the pelvis can also be performed.
While bony changes in the sense of a sacroiliitis that has existed for a long time can be seen in the X-ray, the MRI is the only method that offers the possibility of depicting acute inflammatory changes. Inflammatory processes can be shown either by the administration of contrast media or by special computer calculations in which the display of fatty tissue is suppressed and thus a contrast is achieved. Contrast media are used in most cases, but it is not absolutely necessary. In addition, the contrast media used differ from those used in computed tomography (CT).
Contrast media for an MRI can usually be given despite a "contrast media allergy". In contrast to CT with contrast agent, kidney or thyroid disease is also not a problem. The great advantage of an MRI of the pelvis is that even an early stage sacroiliitis that has not yet caused any bony changes can be detected. However, the interpretation is very demanding and not always clearly possible. The major disadvantages are the high cost of the investigation and the limited availability.
Read more on this topic at:
- MRI of the pelvis
- The MRI examination
laboratory
If there is suspicion that sacroiliitis is present or if this has already been proven by an imaging procedure, a blood test is usually carried out in the laboratory. Typically, an inflammatory reaction can be detected. This means that values such as blood sedimentation or CRP can be increased. However, these values are very unspecific and an increase can have a variety of possible causes. On the other hand, a very special value, which is determined in the case of sacroiliitis in the blood, is HLA B27. If this marker can be detected, there is a high probability that ankylosing spondylitis or a related disease is present. It is also typical for these diseases that other laboratory values such as rheumatoid factors or antibodies, which would indicate an autoimmune disease, are in the normal range. The determination of these values is therefore made to rule out other diseases.
Read more on this topic at:
- Levels of inflammation in the blood
therapy
The therapy of sacroiliitis is mainly based on two building blocks: The consistent one physical therapy and the Pain relief. Physiotherapy should be carried out under professional supervision, and it is important that a patient is also given guidance on how to do this independent To be able to do gymnastics regularly at home. For the treatment of pain there are primarily drugs from the group of non-steroidal anti-inflammatory drugs (NSAID) used. These include, among others Ibuprofen or Diclofenac. First of all, sufferers should only use these pain relievers if necessary take and only when really necessary continuously, and then only for a limited time.
Ask another option Corticosteroids a. These only should at times and if possible only when other pain medication has shown no effect. These corticosteroids can also be applied directly to the affected sacroiliac joints injected become.
There are others anti-inflammatory drugs, such as Sulfasalazine or the so-called Biologicalsthat can be used in the treatment of sacroiliitis. Whether the gift of these means makes sense is or not, but also depends above all on the underlying disease of the sacroiliitis.
In the case of very advanced diseases, a operative therapy be considered, with the Advantages and disadvantages must be discussed in detail by patient and doctor. If the decision to have a surgical intervention has been made, either a Joint replacement or one Righting operation in question.
Duration
Once sacroiliitis has manifested itself and has been clearly diagnosed as such, it usually accompanies the sufferer for a lifetime. In the course of the disease there is typically an increasing deterioration. While initially there is only pain in the lower back or the buttocks, it can lead to restricted mobility and postural damage in the course. If you start early, regularly and consistently perform physiotherapy, deterioration can usually be postponed.This can often prevent a significant impairment of activity and quality of life for many years.
Course and prognosis
Sacroiliitis is one of the chronic progressive inflammationwhich means that once it has occurred it Not more Completely is to be healed and tends to increase over time Heaviness increases. By consistent physiotherapy can a Severe disability nowadays, however, mostly prevented.
Can sacroiliitis be cured?
Sacroiliitis is medically classified as a steadily progressive disease and is therefore usually not completely curable. In most cases, the symptoms keep increasing. However, the course of the disease can be slowed down with regular and individually adapted therapy and in the best case even temporarily stopped. Since a cure can usually not be the goal of the treatment, an alleviation of symptoms and an improvement in the quality of life are sought instead.
Degree of disability (GdB)
The degree of disability (GdB) in sacroiliitis is primarily dependent on functional impairments such as mobility impairment and reduced resilience as well as a possible involvement of other organ systems and any symptoms that may arise as a result. The following values can provide an orientation for inflammatory rheumatic diseases in general, in which sacroiliitis usually occurs: In the case of only slight complaints without significant functional impairment, a maximum degree of disability of ten percent is assigned. In the case of slight functional impairments and low disease activity, the maximum degree of disability that can be expected is 20 to 40 percent. For a degree of disability of over 50% and thus a severe disability, there must be at least permanent significant functional restrictions. In the case of irreversible damage such as stiffening of the back, even 80 to 100 percent are possible.
Sports with sacrolitis
In the case of sacroiliitis, there is no ban on sports; on the contrary, sufficient physical activity is important in order to positively influence the course of the disease. Regular exercise can often prevent the otherwise impending stiffening of the back or at least delay it. There are no general recommendations or restrictions as to which sport should be performed with sacroiliitis. Above all, it is important to find a regular activity that can be carried out with joy and motivation. However, it is particularly important to perform the movements correctly and with a straight posture. For example, you should make sure you have a sufficiently large step width when doing Nordic Walking. In addition, pain must not be ignored and if you experience frequent complaints, you should change your sport if necessary. The best thing to do is to get advice from your doctor or physiotherapist about the most suitable sports for you.
Association with other diseases
Association with Bechterew's disease
Sacroiliitis is the key symptom of the group of inflammatory spinal diseases (Spondylarthridia). The best known disease is Bechterew's disease. However, sacroiliitis does not always occur at the beginning of the disease process. Occasionally, ankylosing spondylitis manifests itself initially as a non-specific inflammation of other joints, so that a diagnosis can often only be made at the beginning. If ankylosing spondylitis is not present, there may also be a less common cause of sacroiliitis, such as an infection.
Read more on this topic at: ankylosing spondylitis
Association with Crohn's disease
Crohn's disease is a chronic inflammatory bowel disease. There is a high association with ankylosing spondylitis, which is the cause of sacroiliitis in most cases. Between five and ten percent of the patients who suffer from ankylosing spondylitis are also suffering from a chronic inflammatory bowel disease such as Crohn's disease. Therefore, if diarrhea is a frequent additional symptom in the presence of sacroiliitis, this association should be considered. The suspicion of a chronic inflammatory bowel disease can be clarified by means of a colonoscopy.
Read more on this topic at:
- Chronic Inflammatory Bowel Disease
- Crohn's disease
HLA B27
HLA is the abbreviation for human leukocyte antigen. It is a system of special structures found on white blood cells that can vary from person to person. It has been found that some HLA groups have an association with certain diseases. The HLA B27 can be detected in 95 percent of people with ankylosing spondylitis. This condition is a common cause of sacroiliitis.
However, HLA B27 detection alone is not proof of the disease, as there are also healthy people with this HLA type. Likewise, five percent of those affected do not have HLA B27. However, if symptoms of sacroiliitis are present, detection of HLA B27 can provide an indication of the presence of ankylosing spondylitis or a related disease. If the result is negative, the diagnosis is unlikely but not impossible. A test for HLA B27 must therefore always be assessed in the individual overall view of the patient's findings.
trigger
The triggers of sacroiliitis are not clearly understood and are still the subject of current research. The inflammation of the joint between the sacrum and iliac bone usually occurs in the context of a rheumatic disease such as Bechterew's disease or a chronic inflammatory bowel disease such as Crohn's disease. There is an increased risk of the onset of sacroiliitis with certain genetic, i.e. inherited, predispositions. Another family member does not necessarily have to be affected. Occasionally, however, there is a familial accumulation of diseases from the named group of forms.