Pain therapy
introduction
The term pain therapy summarizes all procedures that contribute to the relief of acute or chronic pain conditions.
Pain therapy makes use of many different options that can be selected and adapted individually depending on the type of pain and the patient.

What is a pain
Pain describes an unpleasant sensory and emotional experience that is associated with a (potential) Damage to body tissues.
Acute pain has a warning function. For example, if you touch the hot stove top, the pain that occurs quickly causes your hand to be withdrawn.
Without pain perception, the body is at greater risk of injury. One example is diabetics whose nerves are already damaged due to illness. They often lose pain in their legs, which means that injuries to the feet and lower legs often go unnoticed. In many cases, the lesions are not noticed until the tissue dies.
In contrast, chronic pain is often a problem. Chronic pain is when the pain has persisted for more than 3-6 months. In this case, the pain has lost its warning function and has a massive impact on the patient's quality of life. One example is phantom pain, in which patients feel pain in an amputated limb. An adapted pain therapy takes a lot of the suffering of these people.
Pain therapy principles
The different methods that can be used to treat pain work in very different ways. Accordingly, pain can be modulated and suppressed in different ways.
The individual painkillers can, for example, be peripheral, i.e. attach to pain receptors that are located directly at the point of origin of the pain, but they can also be central, i.e. affect the development of pain in the brain and spinal cord.
Weaker painkillers generally suppress the formation of messenger substances that irritate nerve endings and thereby generate pain. A well-known representative of this group is paracetamol, which inhibits a specific enzyme, cyclooxygenase. This enzyme makes certain substances that the nerve endings respond to with pain.
Stronger pain relievers, such as opioids, act on the one hand on pain receptors in the spinal cord and on the other on pain receptors in the brain.
In the spinal cord they dampen the transmission of pain by occupying the receptors in the pain-conducting nerve tracts and activating pain-relieving tracts.
In the brain, they cause a change in pain perception in the brain area responsible for this, the thalamus. There is a high density of pain receptors there, so that the painkillers can attack well there and lead to a dampening of the pain processing.
WHO level scheme
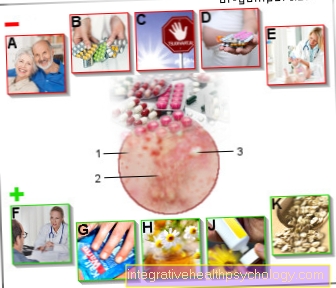
The World Health Organization (English: World Health Organization, WHO) has designed a four-step scheme for pain therapy, which was originally developed for tumor patients, but which is also used to treat other types of pain:
- Stage 1: So-called non-opioid analgesics are used in the first stage of treating pain that is not too severe, i.e. Painkillers that do not belong to the opioid class. These include e.g. Paracetamol, Metamizole and Diclofenac.
These painkillers are combined with so-called adjuvants.These are drugs that do not relieve the pain themselves, but are intended to reduce the side effects of pain relievers. These include Proton pump inhibitors to protect the stomach, laxatives to relax the bowel and prevent constipation (Constipation) and anti-emetics, which are supposed to reduce nausea and vomiting.
It can also be combined with coanalgesics. Coanalgesics themselves have no pain-relieving effect either, but they can increase the effect of pain relievers. This group includes some antidepressants and anti-epileptic drugs.
- Level 2: In the case of more severe pain, level 2 of the WHO level scheme combines level 1 non-opioids with low-potency opioids. Low-potency opioids already belong to the class of opioids, but have only a medium potency among these. These include tramadol, tilidine / naloxone and codeine. Also at level 2, adjuvants and coanalgesics are used in addition to pain therapy.
- Level 3: If the pain is very severe, level 3 of the WHO level scheme is used. Instead of the low-potency opioids, the high-potency opioids are combined with the level 1 non-opioid analgesics.
Highly potent opioids are characterized by a very strong pain-relieving effect. This class includes e.g. Fentanyl, buprenorphine, morphine, oxycodone and hydromorphone. The combination with coanalgesics and adjuvants is also mandatory at this stage.
- Stage 4: The most severe pain states often require invasive therapeutic methods. The painkillers are injected directly to the desired site of action using certain methods.
Level 4 therefore includes epidural anesthesia (PDA) and spinal anesthesia (SPA), in which the pain medication is applied close to the spinal cord via a cannula, as well as peripheral local anesthesia, in which nerves can be blocked directly via a catheter. In addition, methods such as the spinal cord stimulation (English: Spinal Cord Stimulation, SCS) to level 4.
Regional anesthetic procedures
Epidural anesthesia (PDA)
The epidural anesthesia or also epidural anesthesia belongs to the regional anesthetic procedures.
It is often used to treat chronic pain and severe post-operative pain. The PDA is also popular as a pain therapy method in obstetrics.
For this purpose, the patient is injected with a pain reliever into the so-called epidural space, i.e. the space between the sheaths of the spinal canal. The drug is not injected directly into the spinal cord as is commonly believed.
However, it spreads from the epidural space itself to the spinal cord, where it then numbs the nerves running there. The pain medication can be administered once, e.g. for surgical purposes, but it can also be repeated over and over again via an indwelling catheter. The patient can also control this individually according to his current pain condition. This procedure is called patient-controlled epidural anesthesia (English: patient-controlled epidural analgesia, PCEA).
Spinal Anesthesia (SPA)
Spinal anesthesia is similar to epidural anesthesia and also belongs to the regional anesthetic procedures. The pain reliever is injected directly into the space where the nerves of the spinal cord run.
So that the spinal cord is not injured, the spinal anesthesia is only carried out in the lumbar region, where the spinal cord has already stopped and only the nerves run to the lower extremity. These evade the needle when the painkiller is injected, so the risk of injury is low.
Spinal anesthesia is often used for surgical purposes, as the need for painkillers after the operation is lower under local anesthesia during anesthesia. In addition, the procedure is less stressful for the organism, which is particularly important for patients with cardiovascular diseases.
Peripheral conduction anesthesia (PLA)
In peripheral conduction anesthesia, certain nerve bundles are blocked with a locally administered painkiller. This is used, for example, when severe pain conditions are to be expected after operations.
Read more about this under Femoral catheter
Brachial plexus anesthesia
The so-called brachial plexus is a plexus of nerves in the armpit area that consists of the nerves that supply the arm. During surgery in the shoulder or arm area, this nerve network can be blocked in a targeted manner in order to relieve the patient of the pain.
There are various access routes for this, namely on the one hand directly below the collarbone (infraclavicular access), in the neck area (interscalene access) or near the armpit (axillary access).
One of the three approaches is selected depending on the location of the intervention. Then the optimal position of the needle is determined by means of an electrical probe. For this purpose, electrical impulses are emitted, which lead to the contraction of the muscles when they are emitted in the area of the nerve plexus. As soon as this position has been found, the pain reliever can be applied there.
This is also possible in the form of patient-controlled analgesia, i.e. the patient can use a pump to control when a dose of pain medication is administered again. However, when using this procedure, brachial plexus paralysis can occur as a complication if nerves are injured.
Read more on the subject at: Brachial plexus anesthesia
Lumbosacral plexus
The lumbosacral plexus is the correlate to the brachial plexus on the lower extremity. This network of nerves supplies the legs and pelvic area.
When interfering with the thigh, knee, or lower leg, the lumbosacral plexus can be blocked in the same way as the brachial plexus. To do this, the pain reliever is injected into the groin near the large artery of the leg.
Read more on the topic: Regional anesthesia
Non-drug pain management
Spinal Cord Stimulation (SCS)
Spinal cord stimulation makes use of the physiology of pain transmission. This procedure belongs to the group of so-called neuromodulative procedures. For this purpose, an electrode is inserted into the patient's epidural space, via which electrical impulses can then be emitted.
The patient can control the strength of the impulses himself and adapt it to his needs. On the one hand, the electrical currents stimulate pain-relieving nerve cells in the spinal cord, and on the other, the impulses superimpose the pain impulses that are normally transported to the brain via the same nerve cells.
However, since these nerve cells have already been excited by the electrical impulses, they cannot pass the pain on at the same time, so that the pain perception is suppressed.
Transcutaneous electrical nerve stimulation (TENS)
The transcutaneous electrical nerve stimulation is based on a similar principle to the previously described spinal cord stimulation.
With TENS, however, adhesive electrodes are stuck directly onto the painful area.
Electrical impulses that can be emitted via the electrodes stimulate the nerves in this area, which then conduct the impulses to the spinal cord. There the artificially created stimuli compete with the pain impulses and ensure that these can no longer be passed on to the brain in full strength.
In addition, inhibitory pain pathways are activated with TENS as well as with spinal cord stimulation, which additionally suppress the transmission of pain.
Chordotomy
The chordotomy is one of the so-called neuroablative procedures. Fibers of the pain-conducting pathways in the spinal cord are severed in a targeted manner. This is done with the help of a probe that obliterates the pain fibers with either heat or electric current.
The chordotomy is used especially for tumor patients who suffer from severe pain that cannot be controlled otherwise. In particular, pain that only occurs on one side of the body can be treated well with this procedure, as usually only fibers on one side of the spinal cord are severed. This leads to the loss of pain sensation on the opposite side of the body, as the fibers cross in the spinal cord.
Theoretically, the pain pathways in both halves of the body can also be severed, but this increases the risk of injuring other important nerve pathways, which is why unilateral surgery is always preferred. The patient is effectively relieved of pain, but the pain sensation can return over time. This is explained by the activation of alternative pain pathways.
Cryoanalgesia
Cryoanalgesia (icing) is used particularly for the therapy of chronic pain in the spinal column area. The desired nerve is exposed to extreme cold using a special probe (approx. -65 ° C) exposed.
This leads to the destruction of the nerve, so that the pain perception in its supply area disappears. However, there is a chance that the nerve will recover after a while.
Massage therapy
Certain massage techniques can also have a positive effect on pain symptoms.
The massage improves the blood supply to the tissue, which means that nerve-irritating substances and waste products from the cells are removed more quickly. This improves the metabolic status in the muscles.
Massage oils and ointments with arnica, rosemary, devil's claw or pine also improve the blood circulation in the tissue. In addition, reflexology and acupressure can influence internal organs, which can contribute to relaxation and pain relief in these areas.
Direct application of heat can also help to alleviate the pain, as heat also promotes blood circulation and relaxation of the muscles. For example, hot water bottles, warming plasters (e.g. ThermaCare®) or warming pillows are available.
Herbal pain therapy
In the herbal medicine field, there are some preparations that can relieve pain. This particularly applies to pain in the musculoskeletal system, i.e. pain in the muscles and joints. The herbal preparations are usually applied to the affected areas in the form of ointments or oils.
arnica
Arnica has an anti-inflammatory and analgesic effect. The ingredient responsible for this is the helenanine. Arnica is used especially for inflammation of the mucous membranes, bruises, muscle and joint problems.
Would you like to know more about this topic? Read our next article below: Arnica
Devil's claw
The root of the devil's claw has proven itself particularly in the therapy of back pain caused by wear and tear.
The ingredient that determines its effectiveness is the harpagoside. This leads to the inhibition of the formation of pro-inflammatory messenger substances that irritate the nerve endings.
It also leads to the formation of nitric oxide, which improves blood circulation, and the formation of prostaglandins. Prostaglandins are tissue hormones that i.a. Suppress inflammatory processes.
Devil's Claw is suitable for chronic pain therapy, but for the treatment of acute pain, as it takes several days to achieve its full strength.
Are you more interested in this topic? Read more about this under: Devil's Claw
Cayenne pepper
Cayenne pepper contains the active ingredient capsaicin. When applied to painful parts of the body, capsaicin initially activates pain fibers, which is manifested in initial burning and warming of the skin.
Ultimately, however, capsaicin suppresses the release of pain-mediating messenger substances, which reduces the perception of pain. In addition, capsaicin has an anti-inflammatory effect.
Cayenne pepper is used to treat back pain, painful muscle tension, as well as pain from shingles and diabetic nerve damage (diabetic neuropathy).
You can read more in-depth information on this topic in our next article: Cayenne pepper
Willow bark
Willow bark contains the active ingredient salicin, which is metabolized to salicylic acid in the body.
Salicylic acid is also contained in the well-known drug aspirin, which explains the aspirin-like effect of willow bark. Willow bark has anti-inflammatory, antipyretic and analgesic effects.
It is particularly suitable for the therapy of chronic back pain or headaches. It is not used for acute pain, as it can take a few days before the full effect is achieved.
Are you interested in this topic? You can find out more about this in our next article under: Willow bark
Psychological pain therapy
Psychotherapy and behavior therapy play a role that should not be ignored, especially in the treatment of chronic pain. Psychological patterns contribute significantly to the chronification of pain, which creates a vicious circle that is difficult to break out of.
In principle, pain is always assessed emotionally in the brain. This happens in the limbic system, a special part of the brain. This is where it is decided whether the patient has positive coping strategies in dealing with his pain or whether he reacts pessimistically, depressively or aggressively to his pain.
The patient's attitude to pain therefore plays a major role. Mental fixation on the pain and depressive mood contribute to the fact that the pain is perceived more intensely and disappears more slowly or not at all.
In addition, fear of renewed or stronger pain often develops, which leads to avoidance behavior and unconscious tension in the muscles. This leads to cramps and bad posture, which favors the development of new pain and worsening of existing pain.
It is therefore important to take countermeasures at an early stage, especially in the case of chronic pain, by showing the patient pain-relieving behavior. These include, for example, relaxation techniques such as progressive muscle relaxation, autogenic training or hypnosis.
Progressive Muscle Relaxation
With progressive muscle relaxation, the different muscle parts of the body are consciously tensed one after the other and then consciously relaxed again.
This should lead to the fact that the patient gets better body awareness and can actively relax. Hardening and tension in the muscles can be released in the long term, which reduces pain.
This procedure is also suitable for reducing stress and has a particularly positive effect on back pain.
You can find detailed information on this topic at: Progressive Muscle Relaxation
Autogenic training
Autogenic training also serves to improve body awareness. The patient learns to influence himself and his perception, which should lead to general relaxation.
As with progressive muscle relaxation, on the one hand tension in the musculoskeletal system can be released, but on the other hand the function of the organ systems can also be influenced.
Multimodal pain therapy
The multimodal pain therapy combines different pain therapy approaches in a common procedure. It particularly includes patients with chronic pain conditions or is intended to prevent chronification in patients with a high risk of chronification.
For this purpose, the patients are subjected to a seven-day to a maximum of five weeks treatment, which is cared for by various specialist departments. Multimodal pain therapy consists of psychological, psychosomatic, behavioral, but also occupational and internal treatment approaches. The patient is thus comprehensively cared for and, in addition to classic pain therapy, learns, among other things, Coping strategies for dealing with his pain, which can have a positive effect on the pain symptoms.
Multimodal pain therapy is indicated when the patient's pain cannot be managed in any other way, he develops increasingly severe pain, needs more medication, has to see a doctor more often and has comorbidities that make pain therapy difficult.
This principle has proven particularly useful for patients with back pain. If back pain persists for more than six weeks, it is essential to check whether the patient could benefit from multimodal pain therapy.
Also read our article: Pain therapy for the back
Which doctors do pain therapy?
In addition to emergency medicine, intensive care medicine and anesthesia, pain therapy is one of the four sub-areas of anesthesiology. Accordingly, the therapy of chronic pain is mainly carried out by anesthesiologists.Pain therapy is an integral part of anesthesiological specialist training and can be selected as a specialization in the field of anesthesia after completion of this.
Apart from that, in the treatment of chronic pain in the sense of the nowadays widespread concept of multimodal pain therapy, doctors from a wide variety of specialties, as well as other medical professions, always work together to develop an optimal therapy concept for the patient.
What is the procedure for outpatient pain therapy?
The first step of an outpatient pain therapy consists of a thorough anamnesis of the pain, among other things with regard to its timing and the frequency of the pain attacks, as well as a subsequent targeted physical examination. Patients are also often asked to keep a pain diary in order to supplement the information regarding the symptoms.
On the basis of this and on the basis of the diagnostics adapted to the individual complaints, a therapeutic procedure is then developed, which determines the further process. The outpatient pain therapy is based on the principle of multimodal pain therapy, which includes drug-based pain therapy as well as physiotherapeutic and physical measures, as well as relaxation techniques. All of this is done in cooperation with other medical specialties and professions with the aim of achieving the greatest possible freedom from pain for the patient and thus maintaining his mobility.
Also read the article on the topic: Pain diary
What is the process of inpatient pain therapy?
In principle, the process of inpatient pain therapy is similar to that of an outpatient. Compared to outpatient pain therapy, the mostly 10-14 day inpatient pain therapy can be viewed as more intensive. A large team from different medical specialties and various other medical professions is available to investigate the causes of pain and to develop the best possible treatment concept.
This always includes psychosomatic and psychological therapeutic approaches for cognitive management of chronic pain. All of this follows an individually adapted concept, which means that the exact course of treatment differs from patient to patient.
What is a pain diary?
In order to be able to develop an optimal pain therapy with few side effects for a patient with chronic pain, it is important to get to know the pain. The intensity of the complaints in the course of the day, the influence of various activities and drugs on the symptoms, as well as the side effects of the drugs used must be precisely observed and thus understood.
The so-called pain diary is suitable for this, as written documentation in which this information can be collected. Ultimately, it represents a simple but effective progress and therapy control, whereby the setting of the therapy can be improved and individually adjusted. In addition to personal information, it always contains a calendar with so-called visual analog scales, i.e. pain scales for recording the pain severity, as well as an overview of the current therapeutic measures and columns for other conditions and side effects of the therapy.
Read more on the subject at: Pain diary
What does back pain therapy look like?
Back pain is often the result of complex and chronic complaints. Both congenital deformities and acquired, degenerative processes of wear and tear contribute to the development of back pain. Treating the cause of the symptoms is therefore often difficult and frustrating, so that pain therapy is usually the focus. This is typically done as part of a so-called multimodal pain therapy - a collaboration between different specialist areas for the best possible treatment and prevention of pain.
What is essential here is first of all back-friendly behavior in everyday life, as well as moderate sporting activity - protecting the back and its muscles is counterproductive. However, exercise and sport are often only conceivable with medication-based pain therapy. Depending on the severity of the back pain, this can initially be done with non-opioid pain relievers. The focus here is on the so-called non-steroidal anti-inflammatory drugs (NSAIDs), which include ibuprofen and diclofenac. Severe pain may require the use of weak opiates such as tramadol.
In addition to this systemic medication-based pain therapy, infiltration therapies, physiotherapeutic and osteotherapeutic methods, as well as acupuncture, electrical massage methods and psychological approaches such as autogenic training are used for back pain.
What does pain therapy for fibromyalgia look like?
Like the therapy of other complex forms of pain, the pain therapy of fibromyalgia requires a multimodal approach. This is made up of various sub-areas, which in addition to drug pain therapy also include psycho- and physiotherapeutic methods as well as physical procedures, patient training and relaxation methods. As far as pharmacological therapy is concerned, antidepressants and anticonvulsants in particular play an important role - classic pain medication and opioids alone often do not achieve satisfactory pain relief.
Apart from that, the great value of cardiovascular training in terms of aerobic fitness for fibromyalgia patients has become clear. Regular practice of sports such as swimming and walking provides many patients with relief from their symptoms. In addition, full body heat therapy usually has a beneficial effect.
For more information, see: Therapy for fibromyalgia
What does pain therapy for osteoarthritis look like?
The treatment of arthritic pain is often not completely satisfactory even nowadays. This is due to the complex pain associated with osteoarthritis on the one hand, but also to the phased course of the disease on the other. Pain-free intervals alternate with painful ones. The same applies to the mobility of the joints.
Equivalent to other chronic pain syndromes, multimodal pain therapy has ultimately turned out to be the best method of treating arthritic symptoms. First of all, it is important to provide the patient with comprehensive information about the course of the disease and how it can be influenced. Topics such as behavior appropriate to diseases, as well as physical activity and physical strain in everyday life are also addressed.
In addition, different substance groups for anti-inflammatory and pain reduction play a role at the drug level. Especially the so-called nonsteroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids have a pain-relieving effect and improve the diagnosis.
Pain therapy can also be carried out using local anesthesia. The actual effectiveness of active ingredients such as chondroitin, glucosamine and hyaluronic acid, however, has not yet been clarified - different studies have come to different results here. On the other hand, physical procedures, as well as physiotherapeutic methods, electrotherapy, hydro- and balneotherapy are integral parts of pain therapy for osteoarthritis and often provide relief from the symptoms. The effectiveness of acupuncture for osteoarthritis-related pain in the knee joint has now been proven, so that it is now also being used in osteoarthritis therapy.
For more information, see: Osteoarthritis therapy
What does pain therapy for cancer look like?
Tumor diseases can lead to severe pain, especially in the end-stage. The pain can be of different quality, which is why different groups of drugs must be used to alleviate it.
There are basically three types of pain: Nozireceptor pain, which is caused by stimulation and damage to free nerve endings, can be relieved well with nonsteroidal anti-inflammatory drugs (NSAIDs).
Compression pain, on the other hand, which arises from the compression of pain-sensitive tissues and growing into them, can be treated comparatively well with opiates.
Finally, neuropathic pain is caused by direct damage to nerves and can hardly be controlled with classic painkillers. So-called co-analgesics such as antidepressants and neuroleptics are used here.
The pain medication is administered according to the WHO graded scheme and should be carried out in a fixed daily rhythm with the integration of adequate medication as needed for the treatment of cancer pain. Side effects should also be treated or prevented in good time.