Testing of lung function
introduction
As pulmonary function tests (short "Lufu", becomes common Spirometry used as a synonym) is a series of medical tests that check the function of the lungs. These tests determine how much air you can breathe in and out of your lungs, how fast you can breathe in and breathe out again, and how much oxygen from the air gets into your blood through your lungs.
There can be many different causes for a lung function test to be performed. Lung function tests are often done to determine the cause of a prolonged cough or shortness of breath.

In addition, lung function tests can be used to characterize a known disease of the lungs more precisely and to monitor its course. These lung diseases include, for example, asthma, chronic bronchitis or chronic obstructive pulmonary disease (COPD). In addition to checking for these diseases, the lung function test can also check how well a breath spray is working or whether the lungs are working well enough to survive an operation.
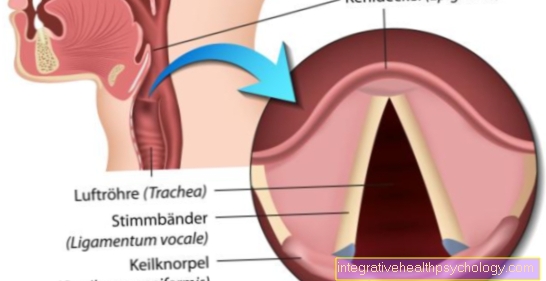
In order for a gas exchange to take place, the inhaled air must first pass through the Main bronchi and the Bronchioles in the Alveoli (Pulmonary alveoli) reach. Only there does the gas exchange between blood and air take place.
Please also read our page Diagnosing COPD and Diagnosis of asthma.
Course of a pulmonary function test
Since there are different tests for measuring lung function, there are also different processes. Pulmonary function tests are generally used to determine various pneumological parameters. Basically, the process for the patient is quite similar for many procedures. With so-called "Open" measurementssuch as spirometry, ergospirometry, the peak flow meter or the DLCO (carbon monoxide diffusion capacity), the test person must inhale test air through a mouthpiece or mask. Various measurements are then made Lung parameters. There are also closed procedures like that Full body plethysmography.
1. Spirometry:
In spirometry, the test person breathes in and out through a mouthpiece. Nasal breathing is interrupted by a nose clip. In addition to normal breathing, breathing maneuvers like a maximum inhalation and exhalation carried out. Different lung volumes are then measured and evaluated.
2. Ergospirometry: This procedure is used to diagnose the performance of the lungs and heart. The spirometry has been expanded to include an ergometer. In which Ergometer it is either a treadmill or a bicycle ergometer on which the patient has to perform. The load can be increased here as required. There will be both cardiovascular (e.g. blood pressure and heart rate) as well as pulmonary parameters are recorded. The latter are determined using the connected spirometer.
3. The peak flow meter:
This device measures the maximum exhalation and is mainly used to monitor the progression of bronchial asthma. The peak flow meter is a tube with a built-in resistor. Against this resistance, the patient exhales as hard as he can in one breath. The patient holds the device horizontally in front of him and breathes in as deeply as he can. Then he puts the mouthpiece firmly in his mouth and exhales with a maximum breath
4. The DLCO:
In this procedure, the subject breathes test air containing carbon monoxidewhich he then exhales through the device after briefly holding his breath. This test measures the ability of the lungs to take in oxygen and release carbon dioxide.
5. The blood gas analysis:
The patient does not need to be actively involved in the blood gas analysis. It is either capillary blood from the fingertip or whole arterial blood from the Radial artery or Femoral nerve taken, which is then examined automatically within a few minutes. It will be the Oxygen, carbon dioxide saturation, of the PH value and the Acid-base balance checked.
6. Whole body plethysmography:
This procedure is a closed procedure, in which the patient sits in an airtight cabin. The patient breathes normally to himself in the cabin. The pressure conditions in the cabin change, from which the breathing resistance, the total gas volume in the chest and the total lung capacity can be determined.
7. The helium washing method:
The patient breathes a certain amount Helium gas one that has the property of spreading only in the parts of the lungs that take part in exhalation. The test can therefore show whether there are larger areas, e.g. Emphysema, are in the lungs that are no longer involved in exhalation.
Spirometry
Spirometry is the most commonly used lung function test.
This test can usually be carried out by your family doctor.
In spirometry, the patient must first breathe in as deeply as he can and then breathe out again as quickly and firmly as possible into a tube. This tube is connected to a spirometer via a hose.
The spirometer measures exactly how much air can be inhaled into the lungs and how much air is then exhaled again (Vital capacity, FVC). In addition, it can be measured how much air can be exhaled with maximum force within one second (One second capacity, FEV1).
During the test, the patient can be given certain medications via a spray and then breathe into the spirometer again.This makes it possible to see whether these drugs are of benefit to the patient, for example whether the asthma spray really leads to improved ventilation of the lungs.
For chronically ill patients who have to regularly check their lung function, for example to find out how much of a drug they need to take, there are also small digital lung function tests for use at home or on the go. A disadvantage of spirometry is that the measured values are heavily dependent on the patient's cooperation. This means that the test result is easy for the patient to manipulate. In addition, young children or people who are particularly sick cannot do this test.
Diffusion capacity
This lung function test examines the ability of the lungs to release the inhaled gases, especially oxygen, into the blood and then to filter them out of the blood again and release them into the ambient air.
In this test, the patient inhales a certain gas and then exhales it again into a tube. This makes it possible to determine how much of the inhaled gas is exhaled again and thus the ability of the lungs to transfer oxygen or other gases into the blood and filter them out of the blood again.
The cause of a disruption of gas transmission in the lungs can be a blockage of a vessel in the lungs (pulmonary embolism) or an overinflation of the lungs (Emphysema) be.
Whole body plethysmography (body plethysmography)
This lung function test measures exactly how much air fits into the lungs (Total capacity, TLC) and how much air remains in the lungs after exhaling.
This remaining air cannot be exhaled and is used to prevent the lungs from collapsing after each exhalation. This volume remaining in the lungs is called Residual volume. With some diseases of the lungs there is less air in the lungs, with other diseases, however, more air than a healthy test person.
In the Full body plethysmography the patient sits in a glass case that looks like a telephone booth. Because the amount of air in the glass case and the pressure of the air are known, a pressure difference in the glass case can be used to precisely measure how much air the patient has in his lungs when inhaling and exhaling and how much the chest is stretched or pressed when breathing The latter value is called the airway resistance (Resistance). In this lung function test, too, the test person has to inhale and exhale through a tube connected to a measuring system. Often, whole-body plethysmography is combined with spirometry in order to get more parameters for the evaluation.
Arterial blood gas determination
In the case of arterial blood gas determination, the blood is examined directly.
To do this, blood must first be taken from an artery from the patient and then analyzed in the laboratory.
The amount of oxygen in the blood can also indicate the function of the Lungs but can also be influenced by other factors.
evaluation of results
The results of the various lung function tests are shown in Dependency from gender, Age and physical constitution of the patient and thus assessed in an objective framework.
Of particular importance are those Vital capacity, which represents the amount of air that can then be exhaled by the patient after maximum inhalation, and the One second capacity, which describes the amount of air that the patient can forcefully exhale in one second after maximal inhalation.
The Vital capacity is an indication of the extensibility of the lungs and Rib cage. As a guideline, for a younger man you can get a man of normal height and weight about 5 liters accept.
The vital capacity decreases the older you get, because the lungs are then no longer as flexible and therefore not as much air can get into the lungs. In addition, the so-called Dead space to be determined.
The dead space volume is the amount of air that is inhaled but does not participate in the gas exchange with the blood vessels, i.e. the air that does not get into the alveoli, but into the Bronchi remains.
The dead space increases when parts of the lungs no longer participate in gas exchange, for example as a result of a vascular occlusion artery within the lungs.
Pulmonary Function Test Values

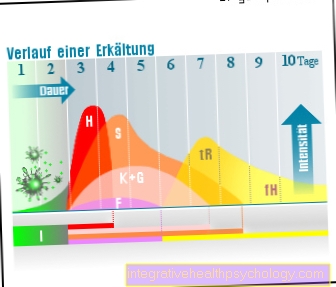
The function of the lungs is usually determined using a spirometer. In this lung function test, certain values are analyzed. One of those values is that Breathing volume, i.e. the volume that is inhaled and exhaled with every normal breath without strain or exertion. With normal breathing, this volume is approximately 0.5 l per breath.
If the patient now inhales maximally, this is the value of the inspiratory reserve volume. This volume can still be mobilized during physical exertion and should contain around 2.5 liters of air per breath. The tidal volume and the inspiratory reserve volume are summarized Inspiratory capacity together. Next, the patient must exhale to the maximum. This maximum exhalation corresponds to that expiratory reserve volume, the value should be around 1.5 l per breath.
The inspiratory reserve volume, the tidal volume and the expiratory reserve volume are summarized Vital capacity together. This value is determined in a lung function test and provides information about how much volume a patient can inhale and exhale during maximum exertion. Overall, the vital capacity should be around 5 liters. Since the volume can be mobilized, this value is determined using the spirometer.
The so-called Residual volume (about 1.5l) cannot be mobilized, but is always in our lungs and is therefore only available with one Full body pletysmograph determinable. Vital capacity and residual volume together are called Total lung capacity designated.
Other values are determined with the help of the lung function test. This includes the One second capacity. The patient inhales as deeply as possible and then exhales everything as quickly as possible. The volume that is exhaled within one second is the so-called one-second capacity. This procedure is also called Tiffeneau test designated.
The relative one-second capacity is given as a percentage and indicates what percentage of the vital capacity can be exhaled within 1 second. This value should be 70-80%. If a patient can breathe out less in one second and the percentage is lower, this indicates an increased resistance in the bronchi (for example due to asthma). This resistance is another value that is determined using a lung function test. This resistance is called the airway resistance (Resistance). The resistance depends on many factors, including the size of the bronchi. The further these are, the lower the resistance for the air. In asthma, on the other hand, the bronchi narrow, which leads to increased resistance and the air more difficult to reach the end of the lungs, the alveoli.
Another value that is determined in the pulmonary function test is maximum expiratory flow (MEV). This determines how strong the patient's respiratory flow strength is when he has already exhaled 75% of his vital capacity, or when he has exhaled 50% of the vital capacity or when he has exhaled 25% of the vital capacity.
Another value of the lung function test is that Breathing limit. This value indicates the maximum number of liters of air a patient can inhale and exhale within a minute. To do this, the patient breathes in and out as hard as possible for about 10-15 seconds (Hyperventilation). The volume that was breathed within this time is then extrapolated to one minute. The normal range here is 120-170 l / min. Values below 120l / min indicate an increased resistance in the bronchi (increased resistance), for example in bronchial asthma.
Finally, the so-called peak flow (breath) is measured, which is particularly important for self-control in asthma. A pneumatograph is used to measure the maximum number of liters a test person can exhale. The value of a healthy patient should be around 10 l per second.
Breathing disorders
A general distinction is made between two types of breathing disorders (Ventilation disorders).
In the obstructive pulmonary dysfunction there is usually a foreign body in the airways, for example a swallowed Lego brick tumorthat presses on the airways or the lungs or diseases such as asthma and chronic bronchitis.
These events increase airway resistance. Due to the disruption of the ventilation, the patient cannot exhale as quickly as healthy subjects, so the One second capacity is increased.
In the restrictive ventilation disorder the vital capacity of the lungs is reduced. Mostly this is caused by the ability to stretch (Compliance) the lungs are no longer large enough as a result of an illness. As a result, the patient can no longer breathe in as well as healthy subjects and a larger amount of air always remains in the lungs.
These complaints often occur in the case of adhesions in the area of the lungs, as this limits elasticity and ductility, or in diseases that limit the mobility of the lungs, such as scoliosis.
Pulmonary function test in asthma

With the help of Pulmonary function tests can one possible diseases such as for example bronchial asthma determine. To do this, you let a patient through you Spirometer (Device for measuring the air volume, etc.) breathe. In asthma, it is especially difficult to breathe out because the resistance in the bronchi (the Resistance) is increased and thus also the volume that the patient cannot exhale (Residual volume). It is difficult for the patient to exhale as much volume as possible in a second, so the relative one-second capacity decreased (below 80%).
Breath and Breathing limit are also degraded. One therefore speaks of a obstructive pulmonary disease. In order to determine at the doctor whether it is a patient with asthma, a provocation test is carried out during the lung function test, which means that the patient inhales a light dose of the contained substance histamine. Since there is already a lot of histamine in the lungs of an asthmatic, he reacts to it more strongly than a healthy patient. An exercise test is also possible, as stress often leads to an asthmatic attack.
In a patient with an asthma attack, the airway resistance (the Resistance) in the bronchi is increased, because due to increased muscle activity (contraction) the bronchi become narrowed. This is due to the messenger substance (Neurotransmitters) Histamine. This is released from the mucous membrane in the bronchi and then causes an asthmatic attack. Since the bronchi are severely narrowed by the histamine, not enough air with new oxygen arrives in the alveoli.
The Alveoli are the final stop in breathing and ensure that oxygen is absorbed and carbon dioxide (CO2) is delivered. Because of the constriction, not enough air is getting into the alveoli and the patient tries to do this by increasing, rapid breathing (Hyperventilation) but makes the situation worse. At the same time, not enough CO2 comes out of the lungs because the bronchi become too narrow. It is therefore important to avoid an asthmatic attack.
A lung function test, the so-called Peak flow meter, be. After inhalation (inspiration), the patient exhales through this with maximum force. Here the patient can measure himself at home how well he can still breathe out. If his values worsen, the patient knows with the help of the lung function test that the asthma can come back again. Because the bronchi become narrower due to inflammatory substances such as histamine or also Leukotrienes or Prostaglandinswhich have the same effect as histamine. This makes it harder for the patient to exhale, which may not be apparent to him at first, but which can easily be determined using the peak flow meter.
Thus, an asthma attack can be prevented with the help of the lung function test. The patient can now for example Atropine take, which dilates the bronchi and thus counteracts an attack.
Pulmonary function test in the child
There are several ways to check lung function in children too. The basic problem that arises with toddlers and babies in particular is the lack of or even impossible cooperation. Some tests require the active participation of the young patient and can therefore be made more difficult by a lack of attention or understanding. Reliable results in a wide variety of lung function tests can often only be expected from the age of 6. A trained practice or ward team can achieve good results with a lot of experience and patience, but even with 2-3 year olds. Procedures that are already used in small children are e.g. whole-body plethysmography, flow-volume measurement, pulse oscillometry and treadmill asthma provocation. Newer methods, such as the ultrasonic test, allow easier measurements in preschool children. The test does not require active participation. It is a gas exchange process in which the child inhales a gas mixture through a mask or mouthpiece, which enables the size and ventilation of the lungs to be measured. The children breathe in and out of the device in a relaxed manner and do not have to perform any breathing maneuvers. The test is also used in babies. This early detection measure should be of great importance, especially for the early treatment of childhood cystic fibrosis. For babies there are also very sensitive devices that can record lung function, so-called infant pneumotachographs. The baby breathes into a mask while sleeping so that spontaneous breathing is analyzed and a volume-flow diagram can be drawn up. This complex measurement is important for the detection and treatment of early childhood asthma and other lung damage.
Side effects of the lung function test
Frequent inhalations and exhalations can cause patients dizzy is or reinforced to cough have to. In addition, deep breathing in and out can lead to a slight feeling of pressure in the abdomen and chest area. In the case of arterial blood gas determination, infections, slight pain at the injection site or minor pain can occur during the blood sample bruises (Hematomas) come.