Therapy of shoulder dislocation
How is shoulder dislocation treated?
The Diagnostic survey of the Shoulder dislocation has important consequences with regard to the form of therapy that is adopted following the diagnosis.
Depending on the form and severity of the shoulder dislocation, a distinction is made between conservative therapy and Shoulder dislocation surgery. At this point, however, it should be mentioned that a designated Shoulder dislocation in any case that joint repositioned as soon as possible (= adjusted again) should be. Failure to do so can cause serious damage cartilage and soft tissues (especially the Rotator cuff) arise.
Since repositioning causes severe pain, the doctor will first give the patient a pain reliever. This also achieves the necessary muscle relaxation, which generally only allows shoulder movements again.

There are several ways to get one Shoulder joint to reposition.
One differentiates:
- The reduction according to Arlt:
The elbow is bent 90 degrees, the poor is placed hanging over the back of the chair while sitting. The doctor applies a longitudinal pull. - The reduction according to Kocher:
It takes place lying down with the patient's upper body slightly straightened. Here, too, the elbow is bent at 90 °. The doctor carries out the repositioning in three steps. - The reduction according to Manes:
This reduction option is particularly used in patients over the age of 60. The doctor pulls on the patient's arm and at the same time moves the humeral head to its original position. Here, too, the elbow is bent at 90 °. - The reduction according to Hippocrates:
This reduction option is also used particularly in patients over the age of 60. The patient lies down, the doctor pulls on the outstretched arm. The doctor's heel serves as a pivot (support) point for the lever.
Repositioning should only be performed by an experienced doctor. Improper handling can lead to serious damage. The measures described above are only intended to describe how a reduction is performed. In no case are they descriptions for the self-performed reduction.
The reduction according to Hippocrates shows that shoulder joint dislocations have been occurring for a long time. In fact, repositioning, for example, by Hippocrates, was carried out more than 2000 years ago.
However, this does not mean that repositioning will always succeed. If the shoulder dislocation cannot be repositioned manually, it is repositioned as part of an operation.
After repositioning, it should always be repeated X-ray in two levels that Shoulder joint to be controlled. In addition, motor skills, blood circulation and sensitivity must be checked. Depending on the extent of the injury, therapy is carried out by immobilization using a shoulder bandage of varying duration. When assessing the length of the immobilization, the severity, but also the age of the patient, are decisive.
A simple dislocation of an elderly patient implies immobilization for about a week, while in other circumstances immobilizations of up to 6 weeks can be conceivable.
Important questions to ask are:
- Classification of shoulder dislocation
- Assess pain
- If a reduction has already taken place, how was it carried out? (spontaneous, automatic, external repositioning)
- To what extent is there a functional restriction (effects on: mobility, strength (dead arm sign))
- Is there a feeling of instability?
- Can neurological failures or circulatory disorders be detected?
- Which sporting activities are practiced? (This question is particularly important with regard to the therapeutic measures; see below)
- Right / left handed?
- Age?
- Which shoulder stressful activities are carried out (professional / private)?
- Are there any previous damage? Previous therapy?
The form of therapy for shoulder dislocation must always be decided individually and must therefore be based on the different circumstances and, of course, the requirements of the patient. A young, sporty ambitious patient has different demands on his shoulder joint than, for example, an older patient without sporting ambitions who can be happy without surgery.
Differences in the field of therapy must of course also take place with regard to the classifications (see above). A traumatic shoulder dislocation is treated differently than a habitual shoulder dislocation, as a result of which the shoulder joint, for example, already dislocates during normal movements.
The declared aim of therapy is primarily the reduction (see above) and, moreover, the achievement of a stabilization of the shoulder joint so that stress becomes possible again.
The form in which this goal can be achieved varies from person to person.
As already mentioned, the classification plays a big role in the treatment. The therapeutic measures take into account certain principles, the so-called treatment principles. Although the doctor may differ in his treatment form in individual cases, the principles listed below generally apply.
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
Treatment principles
1. Traumatic shoulder dislocation:
- The following are usually treated surgically:
with anterior - lower first dislocation - Conservative therapy is usually given with increasing age and with reduced sporting and physical activity.
2. Post-traumatic recurrent shoulder dislocation
- The following are usually treated surgically:
- with anterior - lower first dislocation
- with unidirectional, front instability
- in younger, physically active patients (due to the high rate of dislocation)
- Conservative therapy is usually given with increasing age and with reduced sporting and physical activity.
3. habitual shoulder dislocation:
- In the case of rare dislocation and in cases in which there are no significant functional restrictions, as well as in older patients, conservative treatment is usually used.
- Physically active patients who have frequent recurrent dislocations are usually treated surgically.
- All in all, the therapeutic measure depends on the number of dislocations, the sporting activity and the extent of the subjective and objective impairment.
Conservative therapy for shoulder dislocation
The treatment forms in the context of the various forms of shoulder dislocation were already referred to in the last section. Various therapeutic measures are presented in the following section. If your attending doctor advises you to undergo conservative therapy for shoulder dislocation, he will usually also tell you about special behaviors for everyday life, but also - if necessary - for work and sport. You should know that continuous self-exercises for muscle strengthening and joint stabilization are particularly important and can only be carried out by you beyond conservative therapy. You yourself are significantly involved in the therapy and should take this fact seriously.
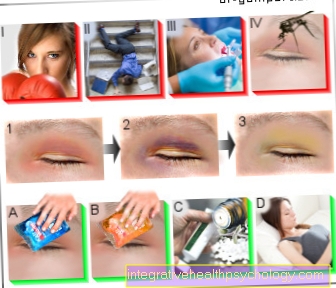
1. Drug therapy:
Medicinal therapy can relieve pain and reduce swelling. To reposition the shoulder, pain can be relieved and tense muscles loosened up so that repositioning is easier (= symptomatic administration of painkillers). So-called NSAIDs (= non-steroidal anti-inflammatory drugs) can also be given orally. Diclofenac, Celebrex, ibuprofen etc. may be mentioned here as examples.
2. Orthopedic technology:
The degrees of severity have already been discussed above. Of course, these degrees of severity also differ in their therapeutic approach. The application of orthopedic technology is also different in the three degrees of severity. The following is intended to show when, for example, the different orthopedic techniques are used:
- Gilchristverband
- Chest abduction splint or pillow
- Antiluxation orthoses
3. Physical therapy:
After the immobilization after repositioning has been overcome, an attempt should be made to strengthen the shoulder girdle muscles as part of physical therapy. Especially those muscle groups that counteract the direction of dislocation are of great importance. Muscle strengthening exercises must - as already described above - always be continued independently. The initiative is therefore an essential aspect. Your physiotherapist will show you joint-centered exercises for muscle strengthening. Other physical therapy measures, depending on the point in time and the stability achieved, include, for example:
- Local cooling (in the acute stage)
- Movement exercises etc. a. to strengthen the muscles
- Exercise bath
- Special physiotherapy techniques (e.g. PNF)
-> Continue to the topic of shoulder dislocation surgery
physical therapy
Physiotherapy must take place at the right moment of treatment. As a first measure, the shoulder joint is immobilized so that it can recover, injuries can heal and the pain can be reduced as far as possible. Only then should physiotherapy be used to maintain freedom of movement in the joint, accelerate healing and strengthen the shoulder girdle so that further shoulder dislocations are prevented.
First of all, the muscles must be loosened and stretched. To do this, bend over and let your arms hang down. The muscles can then be loosened using small circular movements. Physiotherapy then teaches you not only to strengthen your muscles with certain procedures, but also to better perceive and influence your own movements. Awareness of certain movements, for example an upright posture without a hump, is an important step in combating faulty, harmful movements. One such method is PNF, proprioceptive neuromuscular facilitation, in physiotherapy. Here, too, the main focus is on analyzing previous movements and correcting and practicing motor sequences that are as precise as possible.
bandage
A bandage is an elastic piece of fabric that is supposed to completely surround the affected joint region and is adapted to the shape of the body. Various models can be considered for treating shoulder dislocation. A tight bandage can connect the upper arm to the trunk in order to immobilize and protect the joint in the acute initial phase. Modern elastic bandages surround the shoulder joint and are fixed across the chest under the opposite arm. The principle of these bandages is to transfer the weight of the arm completely to the chest and thus relieve the affected shoulder. These bandages restrict freedom of movement only slightly, but stabilize, guide and splint the shoulder joint. In contrast to the tape dressing or the kinesio tape, they completely enclose the shoulder and can guarantee adequate stabilization.
Kinesio tape
The Kinesio tapes are elastic adhesive bandages. The kinesio tapes represent an alternative medical treatment method, which is mainly used in sports medicine and orthopedics, but also in the treatment of internal diseases.
The kinesio tape is stuck on the outside of the skin over the affected area. This must be done by a physiotherapist or doctor or even after long practice and under professional guidance. The tape should have several functions at the same time. In the case of muscular injuries, it offers stability in the joint through external tension. At the same time, it is elastic enough not to restrict the freedom of movement of the joint. In this way, it strengthens the joint function against compressive and tensile stress and allows normal movement in the shoulder. Whether it provides sufficient stability to prevent shoulder dislocations in the shoulder is controversial. In this respect, the Kinesio tape is inferior to the normal inelastic tape dressing.
At the same time, however, the kinesio tape should have other functions. It is supposed to warm the glued area at the same time and stimulate the blood circulation, whereby injuries and inflammations are supposed to accelerate their healing. To do this, the body's own defense against pain should be stimulated, making the shoulder dislocation more bearable.
The Kinesio-Tape can be used both for therapy and to prevent shoulder dislocation. Especially in physiotherapy after a dislocation, the kinesio tape can influence muscle perception and promote muscle building.
Read more about this: Kinesio tape
Exercises to prevent recurrent shoulder dislocations
One of the major problems with dislocating the shoulder joint is preventing further dislocations and maintaining therapy. A single dislocation is enough to change the muscles and cartilage of the joint, and sometimes even damage them, so that the bone can very easily pop out of the socket again and again in the future. During the entire physiotherapy treatment, emphasis is placed on avoiding jerky, provocative movements. However, an important treatment method is strengthening the shoulder girdle muscles. Stronger, wider muscle bellies fix the bone in its joint and block the path in the event of a dislocation.
In a first exercise, the outer arm lifters are strengthened. To do this, stand upright and raise your straight arms sideways up and above head level until they touch above your head. In addition, the exercise with weights in both hands can be difficult. If dumbbells are not available, the exercise can also be performed with full water bottles.
The water bottle exercise can still be varied to target other muscles in the shoulder girdle. Instead of bringing the arms together above the head, they can touch in front of the body at head level and then be brought back as far as the movement of the shoulder blades allows.
Also while standing, the arms can be raised to head height in a further exercise. Then let your arms circle in a small radius, about 10cm forwards, downwards, backwards and upwards. In order to maintain balance, all exercises are done simultaneously on both sides.
Since these exercises are an important pillar of therapy, they should first be instructed by a doctor or physiotherapist. For better exercise, it is advisable to purchase fitness bands, weight cuffs or dumbbells so that the muscle training can be carried out individually.
Surgical therapy of shoulder dislocation
When do I need an operation?
After a shoulder dislocation, the ultimate goal is to reduce the position as quickly as possible. Otherwise, the misalignment can lead to soft tissue damage and circulatory disorders. If such a repositioning attempt is unsuccessful in a conservative way, those affected definitely need surgical treatment. In addition to this main indication, there are other constellations that require surgery to treat shoulder dislocation. Despite a successful conservative attempt at repositioning, an operation may still be necessary in special cases if the instability continues. In addition, traumatic dislocations can be operated on, regardless of whether it is a first-time or recurrent dislocation.
If those affected are young and active in sports, surgical treatment is also preferred. The reason for this is that afterwards there is an increased risk of a new shoulder dislocation if one treats purely conservatively. Surgery reduces this likelihood of recurrence. The general rule is that an operation is necessary when those affected want to fully load their shoulders again after recovery and the goal is to completely restore functionality. The decision to have an operation should generally always be made individually, taking various aspects into account. In addition to the factors already mentioned, such as age and level of activity, aspects such as pre-existing damage to the shoulder, the degree of instability or neurological deficits are therefore important. Additional injuries to bones, cartilage or nerve tissue caused by the dislocation are also an indication for surgery.
Procedure of the operation
The course of an operation in the presence of a shoulder dislocation can be differentiated with regard to the type of access route and the type of reconstruction. Nowadays, the arthroscopic variant is preferred to open surgery. For the open access route, a 10 cm long cut is made on the front. With an arthroscopy, the operation is carried out according to the keyhole principle. The instruments and a mini camera are introduced through three small incisions to treat injured structures. This can be the joint capsule, ligaments or the joint lip, the so-called "Glenoid labrum", be. In the case of more severe dislocations, bony structures may also have been affected, which can also be treated intraoperatively.
The exact surgical procedure depends on which structures have been injured. Damage to the Labrums and the capsule can be operated on both openly and arthroscopically, whereby the labrum is more often treated arthroscopically. In the event of a capsule injury, capsule collapse or capsule shift, which is a capsule-shrinking procedure, can be performed. A shoulder dislocation can lead to a tear in the rotator cuff, which can also be reconstructed arthroscopically. Bony involvement sometimes manifests as an avulsion fracture of the Greater tuberosity of the humerus. In such a case, the fragment can be attached using a screw fixation or a suture anchor fixation. Which method is ultimately used is usually an individual decision. Overall, shoulder arthroscopy is preferred to open surgery because it is less risky.
Risks of the operation
In general, there are always general and special risks involved in operations. This also applies to surgery to treat a shoulder dislocation. The general risks of a shoulder dislocation operation include bleeding with hematoma formation, damage to surrounding nerves and soft tissue, infections, thromboses and pulmonary embolisms. Wound healing disorders of the scars also play a role later on. Depending on whether the operation was open or arthroscopic, the severity of the risks can vary. Wound healing disorders are less likely with an arthroscopic approach than with open surgery with a large skin incision. It is generally accepted that an arthroscopy is less of a risk if the shoulder dislocation is present than if one chooses the open access route to the operation.
The special risks of the operation include, for example, persistent restriction of movement up to stiffening of the shoulder joint. As a long-term consequence, surgical treatment of the shoulder can also lead to osteoarthritis, i.e. non-inflammatory, degenerative cartilage damage. The osteoarthritis in the shoulder joint is medically called Omartrhose designated. There is also the possibility that metal or foreign tissue introduced intraoperatively leads to complications. This includes, for example, loosening or infection of the material.
How long should I not do sports after the operation?
After a shoulder dislocation, those affected should orientate themselves on special guidelines, which specify how long one should not do sports after an operation or how strong the load may be. For the first 6 weeks, it is important to protect the shoulder as much as possible and not to stress it too much. A pure weight load is prohibited for the first 3 months. How long you are not allowed to do a certain sport varies from person to person. So-called "cyclical" sports such as jogging or cycling can be practiced again after 3 months. A 6-month break applies to sports such as swimming or playing tennis, as the shoulder is more stressed here. Sports with a high risk potential for the shoulder, such as handball or martial arts, should be paused for at least 9 months. As a general guide, those affected should be free of pain and that they should be able to cope with stress through therapeutic measures. Ultimately, the individual healing process can last for the duration of sports leave.
Duration of healing
The healing process can vary in length. Factors such as the severity of the dislocation, possible pre-existing damage to the affected shoulder as well as the personal constitution influence the recovery time. In any case, it is important that those affected adhere to individual follow-up treatment plans in order to enable optimal healing. After the operation or a conservative attempt at reduction, the arm and shoulder must initially be immobilized for several days to a few weeks using a special bandage, the so-called Gilchrist bandage.
The duration varies depending on whether the therapy was surgically or only conservatively. This is usually followed by physiotherapy treatment for several weeks. Certain movements of the shoulder joint such as external rotation or repositioning the arm should be avoided in the first few weeks. In general, the faster the shoulder can recover and heal completely, the better the person affected works with the physiotherapy or the more restricted movement is adhered to. Those affected should also attend the regular follow-up appointments. For example, the last check-up appointment is about six months after the day of the operation for surgical treatment.
How long will I have pain after the dislocation?
How long the pain lasts after a shoulder dislocation can vary from person to person. As is so often the case, factors such as the severity and type of dislocation and the therapeutic measures taken play a role. In the acute situation, those affected feel severe pain. This pain can be relieved well by giving painkillers. A conservative reduction can again be felt as particularly painful. After successful treatment, if the shoulder dislocation is uncomplicated and there are no accompanying injuries, the pain can persist for about 2-3 weeks. Those affected usually receive adequate pain therapy. The duration of the pain can be prolonged in the case of complicated shoulder dislocations or failure to comply with movement or load restrictions. If the pain symptoms remain unchanged after 3 weeks, a new medical evaluation is necessary, which can usually be done as part of the regular check-ups.
How long will I be on sick leave?
The length of the sick leave depends largely on the severity of the dislocation, the type of care and the job for which the sick leave is to be issued. People usually stay in the hospital for a few days after the operation. The clinic will issue a residence certificate for this period. The general rule is that movement is restricted for about 6 weeks. In the meantime, a physiotherapeutic treatment is already being considered. Afterwards, those affected can get back to work with office work. Those affected with physically demanding and active jobs can usually be on sick leave for longer. The sick leave can last up to 3 months.