Therapy prostate cancer
Synonyms in the broadest sense
Therapy prostate cancer, prostate CA, prostate tumor
introduction
The type of treatment is determined not only by the tumor stage and the degree of malignancy of the tissue (differentiation), but also by the general condition and age of the patient concerned.
Localized prostate cancer is usually treated locally, i.e. H. it is operated or irradiated. An advanced stage calls for systemic (affecting the whole body) treatment, such as hormonal (antiandrogenic) therapy (see below).
Controlled waiting
If it is a very small, well-differentiated tumor (T1; G1 = low degree of malignancy) in a very old, symptom-free patient whose life expectancy is already significantly reduced due to other pre-existing illnesses, therapy can be dispensed with, as those affected are very likely will not die of the consequences of prostate cancer, but of other pre-existing diseases (e.g. heart failure, coronary heart disease, etc.). In addition, treatment with all sorts of side effects might further reduce the life expectancy of prostate cancer.
Radical removal of the prostate (prostatectomy)
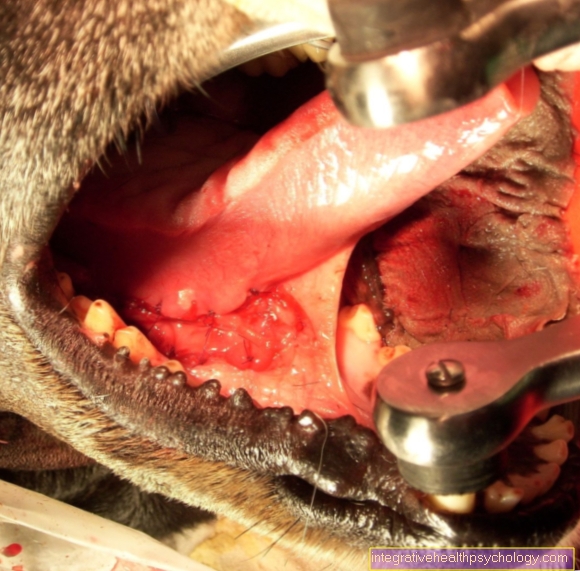
The complete removal of prostate, including its capsule and the adjacent seminal vesicles, is the therapeutic gold standard in Germany for locally limited and well-differentiated prostate cancer. However, it should only be performed if there are no distant or lymph node metastases and the tumor is still limited to the prostate. The surgical access is above the pubic bone or directly at the pelvis. An intervention in the "keyhole technique" (laparoscopy) is also being tested in studies.
There are two main risks associated with this surgery. The first is that Urinary incontinence, so the impossibility of "holding the water". Temporary urinary incontinence is common immediately after the procedure. The regression of this symptom is possible in the further course. In the worst case, however, incontinence can persist.
Second is that erectile dysfunction to name, i.e. the inability to erect. Libido (feeling of pleasure) and the ability to orgasm are not affected. The ejaculation is lost, but it is the stiffening of the limbs that is most often affected (in 50% of cases). Nerve-sparing surgical procedures try to avoid this and to maintain potency.
Rarer complications are bleeding, strictures (scarred constrictions) or inflammation of the Epididymis.
Irradiation
Radiation therapy for prostate cancer can be carried out in all localized stages of the disease. Using modern techniques today, high doses of radiation can be achieved in the tumor region. As a result, a cure rate and disease prognosis equivalent to that of prostatectomy can be achieved. Erectile dysfunction and urinary incontinence are typical side effects here, too, but occur less frequently and less pronounced than after a protatectomy. In addition, reactive inflammation of the mucous membranes of the bladder and rectum can occur.
Find out all about the topic here: Radiation for prostate cancer.
Hormone therapy (antiandrogen therapy)
It has been proven that the prostate needs certain hormones to function. When these substances are withdrawn, not only does the gland itself shrink, but also any tumor that may be present. Conversely, the administration of male hormones (testosterone) leads to a growth spurt. In the case of existing prostate cancer, it must therefore never be administered for the treatment of erectile dysfunction.
Hormone therapy is used for proven lymph node or distant metastases and, depending on the aggressiveness of the tumor cells, also as an additive before or after surgery or radiation therapy.
Read more on the subject at: Hormone therapy for prostate cancer
Methods:
- Orchiectomy: Exfoliation of the hormone-producing testicular tissue. The capsule and epididymis are left in place. The testosterone level is reduced to 10% of the initial level. Treatment is inexpensive and doesn't require prolonged follow-up exams.
- GnRH analogues: These are artificial hormones that intervene in the control loop and, via a constant blockage of receptors, lead to a drop in testosterone levels. The effect is equivalent to that of orchiectomy. Initially, however, there is an increase in testosterone (flare up phenomenon), which can be counteracted with antiandrogens in the first 3 weeks of therapy.
- Estrogens: They work by inhibiting the superordinate hormones in the pituitary gland (pituitary gland). However, there is a risk of cardiovascular complaints. Therefore, long-term therapy is rarely carried out. However, there is the possibility of treating advanced stages with a combination of estrogen and a cytostatic (cell growth inhibitor).
The antiandrogenic treatment usually wears off after 2 to 3 years. A complete hormone blockade should now be carried out using a combination of antiandrogens and GnRH inhibitors. If this is not feasible, you can think about adding chemotherapy drugs. 60% of patients respond to it initially, but in the long run, objective improvement is rare.
One should think hard about whether the hoped-for benefit is worth the expected side effects.
- Antiandrogens:
- Cyproterone acetate: This drug inhibits testosterone production and action at the same time. Impotence, gynecomastia (breast growth) and gastrointestinal complaints can occur.
- Nonsteroidal antiandrogens (flutamide and the like): They inhibit the absorption of testosterone and its active forms in the cell by preventing them from binding to their receptors. This does not interfere with the formation of testosterone. The blood level remains constant for a while, so that the potency is still somewhat maintained.
Here you can find out everything about the topic: Hormonal preparations
Aftercare
Follow-up care is about recognizing a recurrence or progression of the cancer at an early stage.
The person concerned should consult a doctor at regular intervals and report any bone (metastasis) or flank pain (urinary obstruction) that may be present. Medically, something can also be done against the side effects of hormone therapy.
A digital rectal examination (palpation examination of the prostate) should also be carried out regularly for control purposes. An ultrasound examination can also help in the search for urinary obstruction or lymph node metastases.
Since the PSA value should no longer be detectable after a complete prostate removal, every new increase is to be assessed as a recurrence of the disease. Then a subsequent radiation or hormone treatment should be considered. The PSA level should be checked every six months.
Find out here what role the PSA value plays in aftercare: PSA level in prostate cancer
More on this: What are the chances of a cure for prostate cancer?




.jpg)