Causes of water in the lungs
introduction
If there is an accumulation of fluid in the lungs, it is a serious clinical picture that urgently needs to be clarified.
Smaller amounts of fluid in the lungs tend to go unnoticed by the patient. Only when there is a large amount of water or fluid does the patient become symptomatic. He usually needs air and has a dry cough.

causes
One of the most common causes of water in the lungs is heart failure (Heart failure).
If the heart is so weakened for various reasons that it can no longer move the blood back and forth sufficiently in the body, a back pressure occurs that reaches into the lungs. Slowed-down blood causes fluid to spread and accumulate in the surrounding space.
Pressure-induced pulmonary edema is less common but just as dangerous. Here, low air pressure (e.g. in mountaineers) causes liquid to be forced out into the otherwise air-filled lungs.
In the broadest sense, water in the lungs is also in the so-called pleural effusion, i.e. water located at the edges of the lungs. Mostly inflammatory processes are involved here or there is a severe protein deficiency in the body.
Often a cause of water in the lungs is severe pneumonia or a malignant tumor in the lungs. A pulmonary embolism, i.e. an infarction of the lungs caused by a blood clot, can also cause water to accumulate. Also with tuberculosis, which has become rare today.
The causes listed are explained in more detail below:
- Heart attack
- Cancers
- chemotherapy
- lung infection
- Operations
- alcohol
More information on this: The protein deficiency
Heart attack
A heart attack causes damage to the heart muscles due to insufficient blood flow. The damage limits the ability of the heart chambers to pump. Most heart attacks occur in the left ventricle. The blood flows from the lungs into the left ventricle and is then pumped throughout the body. Due to the restricted pumping ability, the heart is no longer able to pump as much blood into the body as before.
The blood, which can no longer get into the body's circulation, backs up in the lungs. This increases the pressure in the pulmonary vessels and more fluid is pressed into the lung tissue. This creates pulmonary edema (water in the lungs). Pulmonary edema occurs acutely in a heart attack and then causes shortness of breath, among other things. The pulmonary edema regresses during therapy. The damage to the heart muscles heals to form a scar. Depending on the size of this scar, there may still be restrictions on the ability to pump the heart.
Similar topics you might be interested in: Life expectancy with water in the lungs
Cancers
In cancer, especially if the findings are advanced, water accumulates, mostly in the bilateral pleural clefts.
Pulmonary edema, i.e. an accumulation of water directly in the lungs, is less common. There are many reasons why pleural effusions occur in cancer. As a rule, e.g. In the case of lung cancer, the lungs no longer expand and collapse in the usual way.
This process enables good and even ventilation of the lungs in a healthy person. If parts of the lungs are no longer ventilated due to a tumor, there is an influx of fluid in these areas, initially in very small amounts that are not noticed by the patient, but later with larger amounts it can lead to severe discomfort and also shortness of breath.
Another cause of water in the lungs or in the pleural space in cancer are the smallest inflammatory changes in the area of the lungs and the pleural space. Inflammation always means inflammable liquid, so-called Exudate. If it accumulates in large quantities, it can cause shortness of breath. Furthermore, the cause are drainage disorders of the lymphatic fluid.
The lymphatic system runs through the entire body. It serves the immune defense and prevents pathogens from entering the body.
Numerous lymphatic vessels pass through the lungs. If a mass, such as a tumor, spreads in the body, it can also press on a lymph vessel and cause a congestion.
This congestion is noticeable by the leakage of lymph fluid into the surrounding tissue. A further complicating factor is that cancer patients experience an imbalance of proteins and electrolytes, which also favors an influx of water into the lungs or into the pleural space.
In the case of lung tumors, the lungs cannot be moved to the usual extent, which also leads to mostly inflammatory edema in the area of the lung borders. A pleural effusion can be recognized in the x-ray by the lightening of the otherwise deep black areas on both sides of the outer deep-lying areas next to the lungs. Sometimes, usually with larger amounts of fluid, a pleural effusion can also be recognized by an ultrasound scan.
Larger pleural effusions must be punctured.
Alternatively, a drainage tablet can be given to the patient so that he excretes more water. In general, however, the triggering factors must be eliminated and appropriate diagnostics carried out.
Read more about the topic here: Lung tumors
Metastases
If metastases form in the lungs - regardless of whether they come from lung cancer or from another organ, e.g. the chest - water retention occurs. This leads to the formation of a pulmonary edema.
Most of the time, the metastases do not cause any discomfort for a long time and the pulmonary edema is not very pronounced. Therefore, metastases are often only recognized in an X-ray. Lung cancer itself, like metastases, leads to water retention and thus to pulmonary edema. Advanced metastases also lead to other symptoms that also occur with lung cancer. These include cough with bloody sputum, shortness of breath, persistent hoarseness and chest pain. There is also general weight loss.
You may also be interested in this topic: Metastasis in breast cancer
chemotherapy
Chemotherapy puts a lot of stress on the body.
The toxins of chemotherapy, which are supposed to fight cancer successfully, also attack healthy cells in the body. This creates numerous side effects. How well chemotherapy is tolerated varies greatly from person to person. Different chemotherapy drugs have different effects on the lungs. Many lead to permanent inflammation of the lungs. Inflammation often causes water to collect between the lungs and the chest wall. One speaks of a pleural effusion. With a pronounced pleural effusion, there is difficulty breathing.
There are also chemotherapy drugs that typically cause pulmonary edema. This includes methotrexate. Methotrexate is a commonly used medicine. For example, it is used to treat breast cancer and acute leukemia.
You might also be interested in these topics:
- Side effects of chemotherapy drugs
- Side effects of methotrexate
lung infection
Pneumonia is usually caused by viruses in the air we breathe, and in rare cases also by bacteria.
Within a few hours or days, an inflammatory process occurs in the area of the lungs. The pathogens attach themselves to the sensitive mucosal epithelium of the lungs.
The body then begins to defend itself with an immune reaction, which also includes an inflammatory change in the epithelium. The purpose is to get the pathogen out of the body as quickly as possible. The inflammation ensures that the gas exchange is throttled at the corresponding point in the lungs and that a layer of mucus is formed as protection.
At first, the patient does not notice the reduced gas exchange, as the other areas of the lungs do the work. The increasingly thick mucus, however, increasingly ensures that the patient develops a cough, which is supposed to transport the mucus with the pathogens outside.
In addition to the inflammatory mucus production, the body also allows cells to migrate into the body that change the temperature setting in the body. The fever rises. In contrast to a lung tumor, an inflammatory temporary remodeling of the lung tissue occurs with pneumonia. The longer and more persistent pneumonia, the more the space in the lungs, which is otherwise filled with air, fills with mucus. This compression can be seen in the X-ray image by a strong lightening in the affected area. When listening to the lungs, one hears intensified breathing sounds. In this area, hardly any air can get into the blood because it is prevented from doing so by the mucous membrane.
In this situation, in addition to the fever and the increasing cough, the patient will also feel increasing shortness of breath. In places where not enough air can be exchanged and slowed down, there can also be an increasing accumulation of fluid.
However, water in the lungs as a result of pneumonia only occurs with very strong and late treatment. Pleural effusions can occur in any case. These are signs of the inflammatory process and restricted movement of the lungs.
Read more on the topic: Signs of pneumonia
Operations
Water retention in the lungs after surgery usually only occurs after major surgery. Pulmonary edema is common, for example after heart surgery. In most cases, the water in the lungs is harmless after surgery and disappears quickly. Usually it is only a small amount of fluid that the patient does not notice.
There are several reasons for water retention in the lungs after an operation. After major surgery, the body needs time to adapt. In addition, operations put a strain on the heart and kidneys. Patients who have previous heart or kidney diseases are particularly prone to pulmonary edema.
Due to heart failure, i.e. insufficient pumping capacity of the heart, the blood backs up in the lungs and water is forced into the lung tissue from the blood vessels. With renal insufficiency, the kidneys can no longer filter sufficient water out of the body. The excess water is deposited in the tissue. The lungs are susceptible to this, as they are usually down during an operation so that the water collects there due to gravity.
There can be massive accumulations of water in the lungs in multi-organ failure. Here the body is completely overwhelmed with the strain. Among other things, the kidneys are no longer able to transport water out of the body. Multiple organ failure can occur in very large interventions and very sick patients.
You might also be interested in this topic: Postoperative Complications
alcohol
Chronic alcohol consumption sooner or later leads to impaired liver function. The liver has, among other things, detoxifying tasks and also ensures that the body is supplied with sufficient proteins.
Long and harmful consumption of alcohol first leads to fatty liver disease, and then later to liver cirrhosis. At this point at the latest, the liver can no longer work in the usual way, which means that toxins can no longer be transported out of the body, but also that albumin is no longer present in the body in the usual amount.
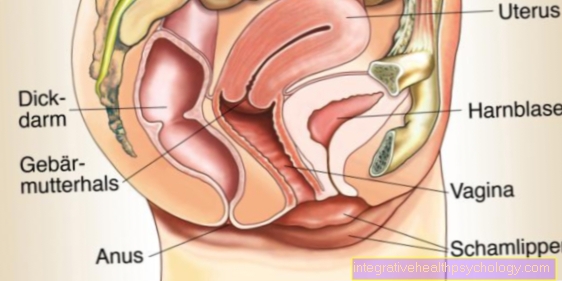
Furthermore, there is a backlog of blood from the liver, which leads to so-called ascites (abdominal fluid).
The ascites is nothing more than filtered fluid, i.e. fluid that is pushed out of the blood by backwater processes and that collects in the surrounding tissue.
In the vast majority of cases, the water collects around the liver, which causes the abdomen to expand and increases pressure on the abdomen.
In some, but rarer, cases, these congestion processes and the reduced amount of protein also lead to an accumulation of water in the lungs, which can lead to typical complaints such as coughing (initially during exercise then also at rest) and then to shortness of breath.
There are some medications that can be used to try to remove the ascites and water from the lungs. In addition to the flushing effect, these drugs also reduce the pressure in the body.
In cases where the drug does not work or where the water is already too large, the liquid must be punctured. In principle, it must also apply here to eliminate the triggering causes. Otherwise, the water will come back very quickly, whether in the lungs or in the abdomen.
Also read: Consequences of alcohol
Consequences of water in the lungs
The consequences of water in the lungs or in the margins of the lungs are varied. With smaller amounts of liquid, the patients usually do not notice anything.
The first symptoms show up with increasing amounts of water during exercise. If the patient complains about shortness of breath, e.g. When climbing stairs, which could previously be carried out without any problems, water in the lungs could be to blame.
As the amount of water increases, the patient becomes more and more short of breath, until the patient feels short of breath even at rest and can no longer easily carry out movements they are familiar with. In addition to shortness of breath, another phenomenon that occurs at least as often is the mostly dry cough.
The lungs try to get rid of the fluid that does not belong in the lungs, causing the urge to cough. Most of the time, very little to no mucus loosens. Sleep discomfort is very common with fluid build-up in the lungs. The patients describe that they can no longer sleep deeply at night and that they experience shortness of breath and a cough.When the headboard is raised upright, however, the symptoms disappear.
With advanced cardiac insufficiency, all patients complain of these symptoms. If there is a lot of fluid in the lungs, the patient will also feel short of breath when sitting. The water is so high in the lungs that it can no longer sink when you sit down to make room for other parts of the lungs for gas exchange.
The treatment should now be started at the latest. If this is not done, the patient dies of pulmonary edema. As a rule, a high-dose dehydration treatment leads to a rapid improvement in the symptoms after the urine production has been increased with medication.
How do you know if you have water in your lungs? Find out more here: These are the symptoms that will help you identify water in your lungs