Water in the stomach
introduction
Water is found in almost all of the human body.
It makes up a large part of human weight.
In many organs too, water is a normal component.
In addition, water can also be found in the free abdominal cavity, i.e. outside the organs.
In this case it is a deviation from the normal state and the cause should be looked for, as it is often serious illnesses that lead to water retention in the abdomen.
If there is an accumulation of water, one speaks of a water belly.
In medical terminology, this is called ascites.
However, this is not a disease in itself, it is simply a symptom of another underlying disease.

That could be the cause
There are many different causes that lead to a water belly.
On the one hand, malnutrition can lead to water leaking into the free abdominal cavity.
This is especially the case when not enough protein is consumed with the food.
The condition is known as hypoalbuminemia. This phenomenon can often be seen in third world countries.
The most common cause of abdominal fluid retention is chronic liver disease, such as cirrhosis.
Here the liver is very restricted in its function due to a strong remodeling of the connective tissue.
The blood in the large blood vessel that supplies it, the so-called portal vein (Porta vein) is jammed and high blood pressure occurs.
In technical terms, this is portal hypertension called. The increased pressure forces water out of the blood vessels into the surrounding tissue, where it collects in the abdominal cavity.
Heart disease can also cause blood to accumulate in the liver and cause a water belly.
This is often the case with heart failure of the right heart.
Kidney disease is another possible cause.
Renal insufficiency can cause water to accumulate in the free abdominal cavity.
Even if there is inflammation of the abdomen, such as peritonitis or inflammation of the pancreas, water often accumulates in the abdomen.
The reason for this is that the inflammatory reaction increases the permeability of the blood vessels.
Here water can easily escape into the abdominal cavity.
Infections, such as tuberculosis, can also lead to a water stomach.
In the course of a tumor that affects the abdominal cavity, the peritoneum is often infected by cancer cells (peritoneal cancer) and this also leads to a water belly.
This can result from colon cancer, pancreatic cancer or ovarian cancer, for example.
In this case, when a malicious (malignant) Is the underlying disease, one speaks of malignant ascites.
Water in your stomach as a result of a cyst
A local ascites, colloquially "water in the stomach", can occur as a consequence of a ruptured cyst.
A cyst is generally understood to be a cavity made of cellular epithelia embedded in the tissue of the surrounding organs.
The inside of the cyst is filled differently depending on the origin of the cause.
In addition to pus, blood, urine, mucus or air, cysts can also contain tissue fluid.
Cysts either exist from birth or form reactionary as a result of infectious events, chronic diseases or injuries.
Often, cysts of the abdominal organs are:
- Liver cyst
- Kidney cyst
- Ovarian cyst
In most cases, these will not show any symptoms.
They only become symptomatic in the form of severe pain in the event of excessive growth and burst envelope structures.
Bleeding can also occur. A ruptured cyst is harmless as long as no blood vessel is injured.
If this is the case, however, immediate action must be taken and an emergency operation carried out.
Water in the abdomen from cancer
In around a third of all cancer patients, ascites, an accumulation of fluid in the abdomen, develops as the disease progresses.
There are various causes for this symptom, which is usually associated with a distended stomach.
Increased pressure on the surrounding organs and complaints due to decreased protein synthesis on the part of the liver are complications to be taken seriously, but they do not threaten the patient's life directly.
If tumor cells settle on the peritoneum, this is called peritoneal carcinosis.
The daughter tumors (Metastases) produce fluid that collects in the abdomen.
The liver is more rarely the cause of the ascites that develop.
If the liver is affected by a few metastases, the blood from the abdominal organs can no longer flow unhindered via the portal vein into the liver.
The blood backs up and the pressure on the vessel walls increases. One speaks of portal hypertension. or portal hypertension.
The increase in pressure causes fluid to be pressed into the abdominal cavity, which is reinforced by the body's own regulatory mechanism of the circulation.
Another, even rarer cause is the tumor-related impressions of the largest lymphatic drainage path.
It is the thoracic duct that transports the lymph to the left vein angle.
A physical examination can objectively determine an amount of ascites of around one liter. Puncture alleviates discomfort and serves to clarify the cause.
Therapy depends on the cause and, in addition to relieving symptoms, can also include the administration of medication.
Pancreatic cancer
Pancreatic cancer is a tumor of the abdomen that is often discovered late.
The first thing that often occurs is unspecific upper abdominal pain and painless yellowing of the sclera (the white of the eye) and the skin.
Nausea, vomiting and loss of appetite can also be present.
In more advanced stages, the cancer cells most often spread to the liver.
The accumulation of water in the abdomen usually indicates an advanced stage of cancer and can indicate either the pancreatic cancer itself or liver involvement.
Ovarian cancer
Ovarian cancer is a condition that typically affects older women.
The disease often falls within a period in which menstruation is no longer regular anyway (menopause or after), so that ovarian cancer initially does not cause any noticeable symptoms.
It is therefore often only discovered when it has grown so large that the mass becomes visible through the abdominal wall.
Usually, ascites only develop in very large ovarian cancer.
The presence of water in the abdomen in ovarian cancer suggests that the disease is advanced.
Alternatively, the spread of the tumor cells into the liver, for example, can also cause these complaints.
Water in the abdomen after an operation
After an operation in the abdomen, the peritoneum is usually damaged for some time.
Just as it happens in other surgical areas, the body begins a defensive reaction to remove the tissue damage caused by the operation.
This typically manifests itself as swelling and water retention.
Depending on the size of the surgical procedure in the abdominal cavity, a pronounced accumulation of water is possible.
Therefore, most abdominal surgery is attempted laparoscopically (only using small incisions and instruments inserted through these incisions), as this is less traumatic for the abdominal area.
In very large operations, the water in the abdomen cannot be bypassed, which is why the abdominal wall is occasionally left a little open in one place so that there is no uncontrolled increase in pressure in the abdomen.
The frequency
In 80% of cases, water accumulation in the abdomen can be traced back to liver damage, i.e. to advanced liver cirrhosis.
Conversely, almost half of the patients with cirrhosis of the liver have ascites as a symptom.
The second most common cause is a tumor.
10% of the cases can be traced back to this.
Concomitant symptoms

In most cases, the fluid slowly builds up in the free abdominal cavity.
For this reason, it remains symptom-free at first.
Only when a large amount of fluid has accumulated does the person concerned notice that their abdominal girth has increased.
This is usually first noticeable in the trousers that are becoming tighter.
If symptoms then occur, it can be assumed that a large amount of fluid has already accumulated or that the amount is increasing rapidly.
A feeling of fullness and pain in the abdomen may occur.
Loss of appetite, nausea and vomiting due to the increasing pressure in the abdomen can also occur.
If the pressure in the abdomen is very high due to the water retention, shortness of breath can also appear as a symptom.
This is the case when the lungs can no longer fully unfold due to the high pressure in the abdomen during inhalation and therefore cannot absorb enough air.
You can also read about the other causes behind a feeling of fullness followed by pain:
Upper abdominal pain and flatulence - what's behind it?
Pain from water in the abdomen
Water in the abdomen is not necessarily painful at first.
There is a lot of space in the abdomen in which the fluid can spread without causing damage, so there is initially no pain reaction.
Only when the skin is tightly stretched due to the accumulation of water or the peritoneum has to hold too much volume, this can cause pain.
Often, however, there are already symptoms related to the cause of the water in the stomach.
Liver diseases can cause pain in the right upper abdomen, diseases of the pancreas make themselves noticeable as belt-shaped pain.
If the accumulation of water becomes so large that it presses on structures such as nerves, vessels, muscles and organs, pain can also be caused.
These are either produced directly on the nerves themselves or can usually be explained by a lack of blood flow and the resulting insufficient supply of blood, oxygen and other nutrients.
This is how the diagnosis is made
If there is a large accumulation of fluid of over a liter, this can be determined by the doctor during a physical examination.
The doctor holds his hands on the right and left sides of the abdomen of the patient lying down and taps against it with one hand. This sets the water in motion and sloshes like waves to the other side, where this movement can be registered by the other hand.
Targeted tapping (percussion) of the abdomen, it can be determined whether there is any fluid in the free abdominal cavity.
In addition, fluid accumulations in the abdominal cavity can also be detected using ultrasound or computer tomography.
To be sure that this is water retention, however, a sample must be taken using a puncture, which is then examined in the laboratory.
Read more on the topic: Ultrasound of the abdomen
How can I recognize water retention in my stomach myself?
Although there is no clear indication of ascites or ascites, some symptoms can be interpreted as pointing the way.
In particular, patients with a known underlying disease such as cirrhosis of the liver should be sensitized.
An increasingly tense and arched stomach is not always noticeable.
Unseen, rapid weight gain and indigestion can be groundbreaking.
Other complaints are fullness and nausea.
Difficulty breathing occurs in more advanced stages.
What is the life expectancy with water in the stomach and cancer?
In most cases, a pronounced accumulation of water in the abdomen indicates a very advanced disease.
In the case of water in the abdomen and cancer (often liver cancer, pancreatic cancer, and ovarian cancer), liver cancer has the best prognosis.
Liver tumors are usually detected earlier than the other two types of cancer, so the cancer can be treated earlier.
In addition, ascites can develop early in liver cancer due to liver dysfunction, so that water in the abdomen does not necessarily indicate an advanced cancer disease.
Pancreatic cancer and ovarian cancer, on the other hand, are usually discovered very late due to their low symptoms.
Often the cancer cells have already spread at the time of diagnosis.
If there is already an accumulation of water in the abdomen, this indicates pronounced tumor processes, so that a low life expectancy can be expected.
What therapy options are there?
On the one hand, therapy can be carried out that only combats the symptoms.
This removes the free water from the abdominal cavity without treating the underlying disease.
For this purpose, drugs can be used that have a dehydrating effect, the so-called diuretics.
In addition, patients should ensure that they are on a low-salt diet.
However, if the medication is discontinued without treating the underlying disease, the fluid in the abdominal cavity will build up again after a relatively short time.
Another option is ascites puncture.
Here, a cannula is inserted into the abdominal cavity and the free fluid is drained from the abdominal cavity.
In general, it makes sense to treat the underlying disease.
If malnutrition is the cause, the fluid no longer collects in the abdominal cavity as soon as the patient's nutritional status is normal again.
In the case of advanced liver cirrhosis or a tumor disease, treatment is often difficult because the disease cannot be cured or can only be cured to a limited extent.
It makes sense to combine both therapeutic approaches. In other words, both treating the underlying disease and treating the symptoms with medicinal dehydration.
What complications can arise?
In patients with ascites due to blood congestion in the liver, intestinal bacteria often migrate into the abdominal cavity.
Serious bacterial peritonitis, i.e. inflammation of the peritoneum, can develop, which must be treated with an antibiotic as soon as possible.
If this does not happen or if it happens too late, it can be fatal.
That is the prognosis
As a rule, the presence of free fluid in the abdomen rather indicates a poor prognosis, since the most common causes by far are advanced malignant diseases, such as cirrhosis of the liver or a tumor.
Some or all of the water can be removed from the abdomen, but since the underlying disease cannot usually be remedied, it will form over and over again as the disease progresses.
The liver as the cause of water in the abdomen

The liver is the main cause of water retention in the abdomen.
If the liver is severely damaged by liver cirrhosis, the blood can no longer flow through it unhindered, accumulates and leads to high blood pressure in the portal vein.
As a result, water is pressed from the inside of the vessel into the free abdominal cavity and collects there.
But also other underlying diseases, e.g. Insufficiency of the right heart can lead to ascites via blood congestion in the liver.
in cirrhosis of the liver
As part of chronic damage to the liver tissue, fibrous scars develop.
One speaks of liver fibrosis.
If the transformation continues, the proportion of functionless connective tissue increases.
The liver can only insufficiently fulfill its tasks in detoxification and in hormone and protein balance. The process is irreversible.
Chronic alcohol consumption is one of the most common causes of liver cirrhosis.
Chronic viral hepatitis (hepatitis B, C and D), autoimmune liver diseases and damage from environmental influences are less common.
Since the early symptoms are very unspecific, the cirrhosis often progresses and leads to severe symptoms.
The connective tissue transformation of the liver tissue causes a more difficult blood flow.
The blood coming from the abdominal organs backs up into the hepatic vein and creates increased vascular pressure.
One speaks of portal hypertension.
In addition to the formation of bypass circuits via vessels in the esophagus and the abdomen, the portal hypertension leads to the development of ascites, water in the abdomen.
In addition, the reduced synthesis of protein, especially albumin, leads to a shift of fluid from the vessels into the adjacent tissue.
In this way, not only edema, accumulations of fluid in the tissue, but also in the abdomen.
Water in your lungs instead of your stomach
Ascites as a pathological accumulation of fluid in the abdominal cavity must be differentiated from the disease-related formation of fluid between the pleura and pleura.
It is a so-called pleural effusion.
The composition of the liquid depends on the cause and is analyzed as part of the diagnostic procedure.
Infectious events, tumorous diseases, changes in the composition of the blood, for example in the case of liver cirrhosis, and the consequences of medical intervention can be the reason for the pleural effusion. Those affected often complain of shortness of breath when it increases rapidly.
Ultrasound is the diagnostic tool of choice because it can detect even the smallest of volumes.
Therapy depends on the severity of the symptoms.
A chest drain conveys the fluid to the outside over a longer period of time.
If water occurs in the lung tissue itself, it is called pulmonary edema.
This can be attributed to heart failure, a disease of the lungs themselves or to a weakness of the kidneys.
You can find out what you should do about water in the lungs at:
This is what you should do against water in the lungs!
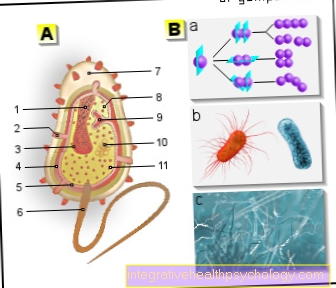
Water in the abdomen after an intracytoplasmic sperm injection
The intracytoplasmic sperm injection, ICSI for short, as a method of artificial insemination is associated with a certain risk of complications.
The ovaries are stimulated during the procedure and stimulated to produce egg cells. The ovaries increase in size due to increased follicle growth.
A certain overstimulation is therefore brought about consciously and is often associated with slight pelvic discomfort.
In rare cases, hyperstimulation syndrome can occur, in which the size of the ovaries increases sharply and is associated with the formation of ascites.
Those affected complain of difficulty breathing and a feeling of pressure in the stomach.
Treatment in the hospital, which sometimes involves puncturing the abdomen, is advisable.
Read more about artificial insemination here: Artificial fertilization
Water in the abdomen during pregnancy
For women with cirrhosis of the liver, pregnancy is an additional burden.
Ascites occurs in about every fifth woman at the end of pregnancy.
One of the reasons for this is that pregnancy has messed up the electrolyte balance and plays an important role in the distribution of fluids in the body.
If water is found in the abdomen during an ultrasound examination during pregnancy, this is initially no cause for concern.
To a certain extent this is quite normal.
It should only be observed further in the further course.
Also read how you can prevent edema during pregnancy:
Edema in pregnancy
Water in the abdomen after a caesarean section
An accumulation of fluid in the abdomen after a caesarean section can occur as part of the wound healing process and is noticeable by a non-decreasing abdominal circumference. If there is ascites that requires treatment, the tissue is relieved by drainage. The liquid can drain off.
Furthermore, with every caesarean section there is a risk of injuring neighboring organs.
If the urinary bladder is injured, a small amount of fluid also spills into the abdomen.
You can find out everything about the caesarean section in the following article:
Caesarean section - indications & risks
Puncture water in the abdomen
The puncture of water in the abdomen can be done for two different reasons.
On the one hand, the puncture is used for diagnostics, because the material obtained can be examined so that a cause of the ascites can be found.
In diagnostics, the number of cells in the liquid, the protein content and the possible presence of pathogens play an important role.
The color of the punctured ascites (bloody, cloudy, milky-cloudy) can also provide clues as to the cause of the disease.
The puncture is usually sonographically controlled (i.e. with the help of ultrasound), the needle can be seen in the ultrasound, so that a suitable position for removing the fluid can be found without injuring organs in the abdominal cavity.
The therapeutic component also plays an important role in ascites puncture.
Large amounts of water can be withdrawn from the abdomen.
If the amount is more than 5 liters, an infusion of fluid into the vein should then take place so that there is no sudden severe lack of fluid in the body.
Read more on the subject at: Puncture water in the abdomen
What are the alternatives to puncture?
Alternative treatments for the water in the abdomen initially consist of causal therapy.
Liver, pancreas, intestinal and ovarian diseases can initially be treated with medication.
Diuretic therapy (treatment with water tablets) can also reduce the abdominal fluid.
In addition, a fluid and salt restriction can prevent the absorption of more fluid, so that the water accumulation does not increase any further and the body absorbs the existing fluid back into the circulation.
Regular weighing is suitable for monitoring therapy, since a rough statement about the amount of ascites can be made via the weight curve.





















.jpg)





