Cardiac asthma
definition
As asthma cardiale (Cardiac asthma) denotes the appearance of the symptom complex of
- Shortness of breath (Dyspnea), attacks of severe shortness of breath, which improve in an upright position (Orthopnea),
- nocturnal cough and other symptoms typical of asthma resulting from left heart failure with pulmonary congestion.

Causes: How does cardiale asthma come about?
The cause of cardiac asthma is left heart failure (weakness of the left heart to support the blood volume required by the body in a required time) with backward failure and pulmonary congestion.
This means that the pumping weakness of the left heart causes the blood to back up in the lungs in front of it, which increases the pressure in the vessels of the pulmonary circulation. There is an escape of fluid and blood components (Transudate) from the pulmonary vessels into the alveoli. Secondarily, the bronchi may narrow (Bronchial obstruction) and the symptoms of asthma cardiale.
A further increase in pressure in the pulmonary circulation leads to the formation of further transudates, which are coughed up as a foamy, reddish-colored liquid; acute pulmonary edema occurs.
Symptoms of cardiac asthma
The main consequences of pulmonary congestion are nightly coughs and shortness of breath (Dyspnea) and severe shortness of breath with improvement in an upright position (Orthopnea) on. The symptoms occur more intensely at night or when lying down, as this, in contrast to the upright posture, increases the pressure in the pulmonary circulation due to gravity. Therefore, patients can put their upper body on pillows at night to relieve symptoms.
In extreme cases, cardiac asthma can turn into acute pulmonary edema with extreme shortness of breath, a feeling of suffocation and foamy sputum.
Shortness of breath
In addition to coughing attacks, as many people know from bronchial asthma, one of the main symptoms of cardiac asthma is shortness of breath. This becomes particularly strong and restrictive when coughing at night ("heart cough") or under great stress.
The severe heart disease, which usually underlies all cardiac asthma, leads to a backlog of blood in the pulmonary circulation. This increased blood volume in the lungs can enter the lungs as a result of the changed pressure conditions and ensures reduced lung ventilation and less oxygen exchange.
Learn more at: Shortness of breath
to cough
Cough is one of the main symptoms of both bronchial and cardiac asthma. Originally, coughing was a protective reflex of the body in order to throw out foreign bodies that could hinder ventilation when the lungs are not ventilated.
In cardiac asthma, the backflow of blood into the pulmonary circulation causes fluid to constantly pass into the lung tissue. This fluid irritates the lungs and leads to the protective reflex of the cough.
Find out more at: Why does a cough occur when the heart is weak?
water in the lungs
Pulmonary edema is the accumulation of water in the lungs. This can be caused by many different diseases, with diseases of the heart being one of the most common causes of pulmonary edema.
Due to the reduced pumping function when the heart is weak, blood backs up into the pulmonary circulation. Here, the increased blood volume increases the pressure on the small blood vessels that lie directly against the lungs and are responsible for the exchange of oxygen. This increased pressure causes fluid to pass from the bloodstream into the lungs, causing pulmonary edema.
Read on below. Pulmonary edema
Differences between bronchial and cardiac asthma
A few examinations are necessary to reliably differentiate cardiac asthma from bronchial asthma.
Basically, however, it can be said that bronchial asthma is a disease that usually occurs in early childhood and remains in varying degrees into old age. Cardiac asthma, on the other hand, is a disease that only occurs in the course of a serious underlying disease of the heart and thus more of a disease of old age.
However, an examination of the lungs and heart is required for a reliable differentiation. The lungs are examined with the help of a lung function test and also subjected to a provocation test, which is supposed to trigger a mild asthma attack. If this test is negative, bronchial asthma is almost always excluded.
The heart, on the other hand, can be examined with a series of examinations for cardiac insufficiency that leads to cardiac asthma. The means of choice here are the EKG and the ultrasound examination of the heart and the heart valves. If there are changes here, cardiac insufficiency can be reliably proven.
Therapy for asthma cardiale
Since cardiac asthma arises from heart failure, the therapy is based on that of heart failure. Elevating your upper body at night can help alleviate nighttime symptoms.
Emergency response
A severe cardiac asthma attack is often based on the decompensation of the heart disease, which is why an ambulance should be called as soon as possible.
Causes for this can be, for example, the occurrence of new cardiac arrhythmias, acute pulmonary edema or a heart attack.
Until the rescue services arrive, the patient should have their upper body elevated and, if available, be given oxygen. Quickly preparing old doctor's letters, findings and an up-to-date list of medication is very helpful for the emergency doctor to quickly get an idea of the situation and save important time.
Medication for asthma cardiale
In contrast to bronchial asthma, the cause of cardiac asthma is not primarily due to the lungs, which is why most common asthma medications only slightly improve the symptoms.
All medications that support the heart and blood circulation help to improve the symptoms
- ACE inhibitors
- Beta blockers
- Aldosterone antagonists
- Diuretics
Diagnosis of cardiac asthma
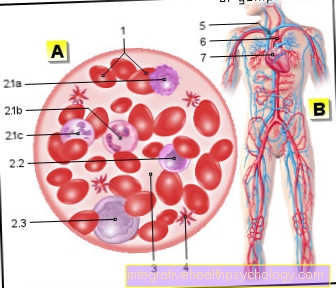
The pulmonary congestion as a result of the heart failure can be confirmed by detection of the so-called heart defect cells (scavenger cells in the lungs that take in red blood cells that have escaped through the congestion) in the Berlin blue color.
These cells are found in the sputum (coughed up secretion) of the patient. Otherwise, the clinical picture of the heart failure is decisive, see also heart failure.
Read more on the topic:
- Cardiac failure EKG
- Life expectancy with heart failure
Circulatory anatomy
The oxygen-poor blood is carried from all parts of the body to the heart via the veins. The entire venous blood ultimately flows through the upper and lower vena cava into the right atrium and from there into the right ventricle, also called the right ventricle.
The right atrium and right ventricle together form what is known as the right heart. From the right heart, the still oxygen-poor blood is pumped to the lungs in order to enrich it with oxygen (so-called pulmonary circulation). The oxygen-enriched blood now flows into the left heart (first into the left atrium, then into the left ventricle) to be pumped from the left ventricle via the arteries back into the various parts of the body.
The heart always pumps the amount of blood volume required by the body per unit of time into the body (so-called. Cardiac output or cardiac output).
Recommendations from the editorial team
You might also be interested in:
- Heart failure
- Therapy heart failure
- Heart failure symptoms
- Cardiac failure EKG
- Isoket®
All topics that have been published in the field of internal medicine can be found under: Internal Medicine A-Z