COPD
introduction
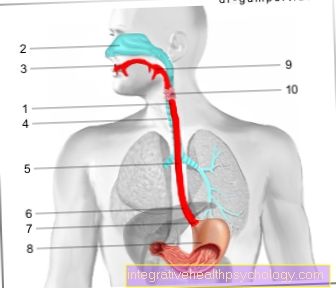
Chronic obstructive pulmonary disease is the most common respiratory disease in Germany. People with COPD suffer from chronic obstructive pulmonary disease. Chronic obstructive pulmonary disease).
This term describes a group of lung diseases, all of which are associated with an increasing narrowing of the small airways. COPD is favored by inhalation noxae, such as smoking cigarettes.

Symptoms of COPD
Those affected suffer from the two main symptoms:
- Cough (with expectoration) and
- Exercise-dependent shortness of breath
COPD is usually preceded by chronic bronchitis a long time before. During this time, those affected have persistent coughing with sputum (= coughed up secretion). This expectoration occurs mostly in the morning. However, if the amount of sputum appears to be very large ("a handful"), other lung diseases urgently need to be investigated.
In the further course, there is exercise-dependent shortness of breath, which then also leads to the diagnosis of COPD, as this reflects the irreversible changes in the lungs. The increasing shortness of breath due to the progressive changes in the lung tissue leads to further effects on other organ systems in the course of the disease. This is noticeable in a reduction in physical performance.
Read more on the topic: Symptoms of COPD
Breathlessness in COPD
Shortness of breath is the typical symptom of COPD. In addition, there is often a chronic cough, which many sufferers do not initially perceive as a serious symptom of the disease.
In almost all affected people, breathlessness initially only occurs during physical exertion and is therefore often interpreted as a lack of fitness and poor fitness.
If larger parts of the lungs are affected, however, those affected suffer from shortness of breath even at rest. Due to the obstruction (narrowing) of the airways, you are unable to breathe out enough air. A lot of oxygen-poor breathing air remains in the lungs, which is why the body can no longer absorb sufficient oxygen.
What is the general course of COPD?
As a rule, COPD begins insidiously and usually only becomes apparent after a certain period of time.
At the beginning of the disease, only a chronic cough is initially noticeable, which is caused by the permanent irritation of the airways. Later, sputum, which occurs mainly in the morning, is added to the cough. Then you notice shortness of breath, which occurs particularly during physical exertion.
How long it takes for the individual symptoms to become noticeable differs from person to person and depends on age, the pollutants inhaled and many other physical factors.
The longer the COPD persists, the stronger the symptom of shortness of breath becomes. At the beginning it is only noticeable during physical activity, but later it comes to permanent shortness of breath, which at some point has to be treated with oxygen.
The lack of oxygen causes further symptoms: so-called cyanosis, a bluish discoloration of the lips and the skin under the fingernails (comparable to blue lips when someone is cold).
With longstanding COPD, the heart is increasingly affected. There is a weakness especially in the right half of the heart.
In addition, the long-standing obstruction of the airways means that inhaled air increasingly remains in the lungs. This is, so to speak, “inflated” more and more with air. This condition is also called emphysema.
Read more on the topic: Course of COPD
Division of COPD into stages
COPD is divided into different stages, which are based on the severity of the disease.
One possible classification divides the disease into four different stages, which depend on the values of the lung function test. Stage 1 is the mildest degree of severity, stage 4 is the most severe form of the disease.
Alternatively, the classification is based on the severity of the shortness of breath. This classification divides COPD into severity levels 0 to 4.
In addition, there is the staging that is labeled GOLD A to D. Several parameters are used as a basis for this classification. This includes pulmonary function testing and clinical symptoms.
Read more on the topic: Stages of COPD
Stage 1
Stage 1 of COPD is characterized by a one-second capacity of less than 80% of the target value in lung function. For the one-second capacity test, the patient takes a deep breath and then has to exhale everything as quickly as possible. The proportion of air that can be exhaled within one second is measured and is decisive for determining lung function.
Stage 1 is comparable to the GOLD A classification. In this case, shortness of breath is only present during intense physical exertion, when walking quickly and when walking uphill. The clinical symptoms (cough, sputum, sleep quality) are hardly or only slightly restrictive in everyday life.
Stage 2
In stage 2 there is a one-second capacity of 50 to 79%. This means that in the one-second capacity test, those affected were able to exhale significantly less air than other healthy people.
During exercise, there is increased shortness of breath, which is why those affected walk more slowly than their peers. In addition, breaks are required when walking normally. In the GOLD classification, stage 2 corresponds to GOLD B.
The main difference to the first stage lies in the significantly increased noticeability of cough, sleep and quality of life, which is associated with a restriction in everyday life. In both stages, exacerbations (derailments) of the disease occur no more than once a year.
Stage 3
In stage 3, lung function tests show a one-second capacity of 30 to 49%.
When walking, affected people have to take more breaks. By definition, these breaks take place after about 100 meters of walking and last a few minutes. The stage is comparable to GOLD C. These people have two or more exacerbations per year, and here too the clinical symptoms are conspicuous, so that they restrict everyday life, although many everyday tasks can still be managed normally.
Stage 4
Stage 4 is the most severe stage of COPD. The one-second capacity in the lung function is only 30% of the target value in stage 4. In addition, people with a one-second capacity of less than 50% and an additional oxygen deficiency that requires treatment (oxygen pressure 50 mm Hg) are classified in this stage.
In most cases, those affected can hardly leave the house due to the severe shortage of air, they are often no longer able to take care of themselves.
Stage GOLD D is comparable. Here, too, more than 2 exacerbations per year are to be expected, the clinical symptoms are very restrictive in everyday life.
What does the end stage of COPD look like?
End-stage COPD is determined by severe limitations in everyday life. Those affected often suffer from such severe shortness of breath that they are barely able to leave the house. Usually they can no longer look after themselves independently.
In addition, there is an increased susceptibility to infections, especially in the end stage. A simple cold can quickly derail and lead to life-threatening deterioration.
The narrowing of the airways causes a lot of air to remain in the lungs that cannot be breathed out. This so-called air trapping leads to an overinflation of the chest. In addition, the air remaining in the lungs is not very rich in oxygen. This not only results in a lack of oxygen throughout the body, it also constricts the blood vessels in the affected lung sections.
In the end-stage of the disease, this vascular narrowing can lead to increased pressure in the lungs. The heart has to constantly pump against this. If the heart muscle cells can no longer compensate for this increased requirement, cardiac insufficiency also occurs. This particularly affects the right half of the heart.
More on this: End-stage COPD
Consequences of COPD
Pulmonary emphysema describes a progressive remodeling and breakdown of the lung tissue with a decrease in the gas-exchanging surface. The reason for this lies in the narrowing (= obstruction) of the airways. This leads to difficult exhalation with only slightly impaired inhalation. This leads to overinflation of the lungs and damage to the tissue that forms the alveoli.
Their number and area then continuously decrease as the disease persists. In addition, inhaled poisons (e.g. cigarette smoke) lead to direct changes in the lung tissue and further remodeling of the lungs occurs. Due to the reduced gas exchange area, less oxygen can be absorbed and less carbon dioxide can be released from the blood and this leads to chronic oxygen deficiency in the blood. In return, harmful carbon dioxide accumulates.
Changes in the tissue also affect the vessels in the lungs, which can lead to pulmonary hypertension.
You can read how dangerous this can be in our article: Pulmonary hypertension - that's how dangerous it is
Therapy for COPD
The main therapy for COPD is to quit smoking or avoid other triggers such as toxic fumes. There is also physical training and activity. This promotes physical performance and can at least slow the progression of the disease. (However, a consultation with the attending physician is necessary here, since in the case of advanced cardiac insufficiency, excessive exercise can again be harmful!)
In training courses, those affected learn how to deal with their disease and measures are taught that help those affected to deal with the shortness of breath, e.g.
- Posture when breathing is difficult (Coach seat)
- Use of the so-called lip brake (breathing technique that prevents the alveoli from collapsing)
- Training of the auxiliary respiratory muscles (not used during normal breathing, can be activated if necessary and additionally support the breathing movements of the chest)
More information on this topic: Therapy of COPD
Medication
The treatment options with drugs are now very diverse. The administration of different drugs can be designed depending on the stage and concomitant illness in order to create an optimal therapy plan for each patient. However, these drugs are not able to cure the disease. So far it is only possible to slow the progression of COPD.
Basically, the therapy usually includes basic medication that is taken daily and usually has a long-term effect (Basic medication). There are also drugs that only have to be taken when needed (Reliever medication). These are particularly suitable for short-term attacks of shortness of breath and usually only have a short effect. The drugs attack different mechanisms that lead to COPD.
Drugs that widen the muscles of the airways, so-called bronchodilators, are particularly important. These medications relax the muscles in the airways, making them wider and allowing more air to flow through them. So-called sympathomimetics and parasympatholytics are used for this. Most of these drugs are administered by inhalation because this way they get directly into the lungs and are ideally distributed there.
Both groups of drugs are available in both a short-acting and a long-acting form. Usually you start the therapy with one of the drugs. These include salbutamol, fenoterol, ipratropium bromide, salmeterol, formoterol, tiotropium bromide.
Depending on the severity of the disease, reliever medication from other drug classes can also be prescribed. A basic combination therapy with the drugs is also possible.
Steroids and anti-inflammatory drugs are also prescribed to counteract the chronic inflammation associated with COPD. Inhaled steroids include budesonide, fluticasone, and beclometasone. Roflumilast is prescribed for repeated derailments, but is very rich in side effects. By inhibiting a certain enzyme called phosphodiesterase, the inflammation is contained on the one hand, and the vessels in the lungs are widened on the other.
Theophylline is very rarely used. However, this drug has the most side effects and should only be used in exceptional cases.
Read more on the topic: Medicines used to treat COPD
When do those affected need oxygen therapy?
Oxygen therapy for COPD can take different forms depending on the symptoms of the person concerned. With COPD, the body is no longer able to take in sufficient oxygen from the air.
Reference values for determining the oxygen content in the blood are the partial pressure of oxygen and the oxygen saturation.
The oxygen partial pressure is a measure of the amount of dissolved oxygen in the blood. It is given in the unit mmHg (historical unit: a mercury column was previously used for measurement). The critical value from which oxygen therapy would be initiated would be <60 mmHg.
The oxygen saturation is given as a percentage and indicates what percentage of the red blood cells are saturated with oxygen. The reference range here is 92-99%. The critical value here is a saturation below 90%.
Therefore, people who have an oxygen pressure <60 mmHg in their blood should be provided with an oxygen device. In the late stages of COPD, long-term oxygen therapy of at least 16 hours per day is usually necessary.Often, however, it is advisable to start oxygen therapy beforehand. For example, many people sag with their oxygen saturation in their blood when they sleep and therefore need oxygen therapy at night.
Equipping with oxygen at an early stage often makes sense even with physical exertion and sport.
Find out more about the topic here: The oxygen saturation
Administration of oxygen
As the disease progresses, the effectiveness of breathing decreases. If too little oxygen is absorbed into the blood in the lungs and too little CO2 is released into the air, this process must be supported by oxygen therapy.
The oxygen is then usually administered for at least 16 hours a day. For this purpose, the patients receive a mobile oxygen device and a nasal cannula or mask that continuously delivers the oxygen to the patient. If the drops in satiety occur mainly at night and during sleep, there are various forms of therapy for the night.
These can also be helpful during the day in the event of acute deterioration. Masks that keep the airways open to support the patient's own breathing and make it easier to breathe out are now widespread. (so-called non-invasive ventilation). A stay in a sleep laboratory is necessary to initiate this therapy.
You may also be interested in this topic: Breathing exercises for COPD
Does an operation help with COPD?
Surgery is not a common therapeutic measure for COPD. The primary problem in this condition is the airways. These cannot be operated on in such a way that they are less narrowed.
One problem associated with COPD is the reduced exhalation of air from the lungs. In this way, a lot of oxygen-poor air remains trapped in the lungs and the organ overinflates. In such cases, the installation of so-called lung valves can help.
A lung transplant is also an option for some people with COPD as a last resort.
Operational measures
Surgical measures can also be considered for a small group of sufferers.
The bronchoscopy (lung specimen) is a procedure that can be used. A tube with a camera at the tip is inserted into the windpipe and the doctor can assess the airways on a screen. This method is very suitable for inserting valves that can reopen narrowed airways. These valves allow air to escape from over-inflated sections of the lungs. In this way, sections that were previously over-inflated become smaller and healthy sections of the lungs can expand better again.
A lung transplant can also be performed if COPD is very advanced. The transplantation of a lung can significantly improve the quality of life, but it is also associated with many risks and lifelong use of strong medication with correspondingly many side effects.
The prognosis and complications of COPD
The narrowing (obstruction) of the airways is usually progressive and leads to increasing physical limitations. The remodeling of the lung tissue puts a strain on the heart, as it now has to pump against the changed lung tissue. This reacts with an enlargement of the muscle tissue which leads to an increased risk of diseases of the cardiovascular system.
This compensation cannot be sustained forever and heart failure occurs later (first the right, later also the left part of the heart fails). This means that the heart can no longer pump the required amount of blood. There is also increased shortness of breath rattle (Pulmonary edema), Swelling of the liver and spleen, and water retention in the legs
The enlarged heart caused by lung disease is called the "cor pulmonale" (lung heart). Restrictions due to the reduced gas exchange and the effects on the cardiovascular system add up.
Further concomitant symptoms in later stages are weight loss due to increased exertion in breathing, muscle weakness and / or osteoporosis.
Over time, the body gets used to a lower level of oxygen in the blood. Nevertheless, it is increasingly difficult for him to compensate for infections, so that acute worsening of respiratory distress often occurs, which often leads to earlier antibiotic therapy, hospital stays and additional oxygen or ventilation therapy.
Warning signs of an acute worsening of everyday symptoms (=Exacerbation) are:
- Increasing shortness of breath
- increased cough and sputum
- Discoloration of the sputum
- Breathing faster
Clouding of consciousness and tightness in the chest are absolute warning signs and a doctor should be consulted immediately. The clouding of consciousness can indicate a so-called "hypercapnic coma". This is a coma due to massive buildup of carbon dioxide from a lack of exhalation. Exhalation can be assisted by various methods and the patient can be stabilized.
Can you cure COPD?
By definition, COPD is incurable. COPD stands for a chronic obstructive pulmonary disease and is characterized by the fact that damage to the lungs occurs that is irreversible.
Medicines can reduce the lung's response to this damage and, in some cases, also help the lung tissue to regenerate. However, a total cure is not possible.
Smoking is primarily known to be the triggering pollutants for COPD. If an affected person quits smoking, the symptoms often improve for a long time, but damage has almost always occurred from which the lungs cannot recover. Thus, COPD is not considered a curable disease.
So far, it has only been possible to stop the progression of the disease with drugs and other therapeutic options. Depending on the stage of the disease at which the COPD is recognized, the symptoms of the disease can be withheld for a long time. The earlier the diagnosis is made, the more promising the options.
In addition to drug therapy, a lung transplant is an option for some people. In principle, this can cure COPD, since the disease only resides in the lungs, but it is associated with many risks and the use of new drugs with side effects.
Life expectancy in COPD
Life expectancy with COPD is significantly limited compared to people who are not ill.
As the disease progresses, those affected increasingly suffer irreversible damage to the lung tissue. In particular, people who consume nicotine continuously must expect the disease to progress rapidly. In the final stage, so-called exacerbations (acute deterioration) often occur, which are usually triggered by minor respiratory infections.
The disease increasingly results in weak breathing, which can be improved with various drugs and aids, but a causal therapy of the disease is not possible.
This can delay the progression of the disease, but not prevent it. Life expectancy with COPD is heavily dependent on the severity of the disease. The age of the person concerned and additional illnesses also play a role.
In general, it can be said that COPD reduces life expectancy by around five to seven years. Acute infections and prolonged smoking worsen the prognosis. Respiratory therapy and lung exercise, on the other hand, can improve life expectancy.
Read more on the subject at: Life expectancy in COPD
Care level for COPD
A care level can be applied for if someone is no longer able to meet their basic needs (personal hygiene, nutrition, mobility) independently due to an illness.
Depending on the severity of the disease, the person concerned is assigned to a care level. Care level I means that someone needs help for at least 90 minutes a day. With care level II it is at least 3 hours a day and with III. Care level someone must be dependent on at least 5 hours of help a day. A nurse may need help, especially in the later stages of COPD.
Is COPD Contagious?
COPD is not contagious. Since the cause of the disease lies solely in the person concerned, the disease cannot be passed on to other people.
In contrast to many infectious diseases, no pathogen is the cause of COPD. Rather, the trigger is pollutants that get into the lungs of the affected person. In principle, a smoker who constantly smokes in the presence of other people can also contribute to the development of COPD in you. However, this is not a form of infection with a disease.
Which sport is cheap for COPD?
Throughout Germany there are special lung sports groups that specialize in physical training with lung patients. Asthma and COPD are particularly common among lung diseases, so that many pulmonary sports groups have specialists in sports for COPD.
The aim of lung sport is on the one hand to strengthen the respiratory muscles through specific gymnastic exercises. In addition, special breathing techniques can be learned as part of this sport group, which make breathing easier in the event of acute shortness of breath.
In addition, endurance and flexibility are trained. These not only help the lungs to perform better, they also make the entire body fitter. This makes many everyday activities easier for those affected. Movement sequences and coordination skills are also improved.
The great advantage of these lung sports groups is that specialists can design the training individually for each individual. In this way, everyone affected is picked up at their fitness level and benefits from the training.
In general, for people suffering from COPD, training that can improve their condition is recommended. Beginners in particular benefit not only from long jogging laps but also from short walks. However, if you have not done sport for a long time, you should only start training after consulting your doctor and follow his instructions.
Disease emergence
There are essentially three mechanisms involved in the symptoms of chronic obstructive pulmonary disease (COPD). Chronic inflammation means permanent irritation of the airways.
The irritation leads to:
- Swelling of the mucous membrane of the bronchi due to fluid retention (bronchial edema)
- Contraction of the bronchial wall muscles
- Increase in mucus production
The simple chronic inflammation is characterized by a thickened mucous membrane in the lower airways and an increased production of mucus. In healthy people, small cilia in the lower respiratory tract ensure that the mucus and other particles are carried away in the direction of the larynx, i.e. out of the lungs. In the case of permanent inflammation, this transport of the ciliated epithelium is also disturbed, the mucus remains in the airways.
The recurring inflammation leads to an over-excitability of the tissue with constriction. If this is not treated consistently, there is a risk that the chronic obstructive pulmonary disease (COPD) will continue into the alveoli. The alveoli can stick together and are destroyed. The result is an overinflation of the lungs, a so-called pulmonary emphysema with impaired breathing.
Causes of COPD
The term COPD primarily encompasses chronic inflammation of the airways (chronic bronchitis) and the reconstruction of the lung architecture (pulmonary emphysema). Many factors contribute to the development.
The most common cause of chronic inflammation and narrowing of the airways is long-term inflammation and increased mucus production in the airways (chronic bronchitis). This manifests itself as a long-lasting cough with shortness of breath, which is not dry, but is associated with sputum (i.e. mucus). Factors that favor COPD can be:
1. Smoking
At 90%, smoking is the number one cause of COPD. It doesn't matter what type of tobacco you smoke or whether you smoke passively. While smoking is often the cause of COPD, only 20% of smokers will develop COPD at some point, suggesting that other factors may also play a role. Furthermore, the constant irritation caused by the toxic substances in the smoke leads to increased mucus production.
Even in young smokers, the narrowing caused by the inflammation and the increased mucus is clearly measurable, but it is often still reversible. However, permanent damage leads to irreversible damage to the airways, which can manifest itself as a smoker's cough, and the manifestation of COPD.
2. Dirty air
In principle, any type of air pollution can cause irritation. Miners or other professional groups with years of fine dust pollution often develop COPD. Inhaling toxic fumes is also irritating to the lungs and can lead to COPD.
3. Development of the lungs
Factors that inhibit lung development in childhood and which can be associated with later COPD should also be mentioned. These include
- low birth weight and
- frequent respiratory infections in childhood
4. Gene defect
A genetic defect can rarely be detected. This defect in the genetic code leads to a lack or complete lack of enzymes that accelerate various processes in the lungs. If these enzymes are missing, if they work incorrectly or if they are present in insufficient concentrations in the blood, these processes in the lungs can no longer take place properly and functioning lung tissue is destroyed.
The best-known example is alpha1-antitrypsin. Any patient diagnosed with COPD before the age of 50 should have a blood test checked for the presence or activity of these enzymes.
Also read: Consequences of smoking
Diagnosing COPD
The diagnosis is based primarily on pulmonary function tests. These also enable a differentiation between bronchial asthma, which is often associated with similar symptoms. These tests can be used to measure different volumes in the lungs.
1. Spirometry
So-called spirometry plays a major role in COPD. Here you breathe in and out through a mouthpiece in which a measuring sensor is attached. A spirometer measures the amount of air that is exhaled and inhaled.
2. Measurement of the one-second capacity
In addition, one measures within the so-called Tiffeneau tests the maximum amount of air that can be exhaled in one second. This value is called the forced expiratory capacity (FEV1).
This value indicates the percentage of the total inhaled volume that can be exhaled within this first second with maximum effort.
This value is also used to determine the severity of the disease. The lower this value, the more severe the disease or breathing restrictions.
The disease is classified according to the GOLD scheme. The disease stages in this scheme include the following stages:
- I Mild (FEV1> 80%)
- II moderate (FEV1 50-80%)
- III severe (FEV1 <50%)
- IV very severe (FEV1 <30%)
Read more on this topic at: Stages of COPD
3. Body plethysmography
Another test determines the amount of air that remains in the lungs after exhaling. Since this volume remains in the lungs during simple breathing, it cannot be measured by spirometry, as this method only measures moving air currents. Since COPD, as described above, leads to overinflation of the lungs, other procedures are required here. To measure this remaining volume (= Residual volume) the measurement is carried out in a closed chamber, the so-called body plethysmograph.
Further information on this: Diagnosing COPD
Frequency of COPD
The Chronic bronchitis is the most common chronic lung disease. Approx. 20% of all men have it. Women are significantly less affected. For every sick woman there are 3 - 4 sick men. One reckons with around the world 44 million Sick people. In Germany around 15% of those over 40 years old are ill. There are twice as many among those over 70. Most of those affected are Smoker or Ex-smoker.
What is the Difference Between COPD and Asthma?
COPD and asthma are two very different diseases, which, however, can cause similar clinical pictures, as both lead to complaints due to an obstruction (unification) of the airways.
While COPD is a disease that tends to occur in the second half of life, children and adolescents are mostly affected by asthma. With them, the symptoms often improve in adulthood.
COPD is an obstruction of the airways that has a chronic cause.Most of the time, the airways are damaged by inhaled pollutants. Asthma, on the other hand, is in most cases a reaction to allergic substances that result in an acute narrowing of the airways. For this reason, asthma occurs mainly episodically and attack-like, there are symptom-free phases. In contrast, COPD is often insidious at the beginning, so that it is not particularly noticeable and only shows a clear deterioration in the course. Due to the unnoticed beginning, the damage in COPD can no longer be reversed. The obstruction is therefore referred to as persistent (= permanent).
In asthma, on the other hand, the obstruction can be temporarily resolved with medication. As soon as the substance to which the affected person is reacting is no longer in the body, the asthmatic symptoms also improve.
You might also be interested in these articles:
- Asthma symptoms
- This is how asthma is diagnosed













.jpg)