The jaw cyst
definition
A cyst is a cavity in tissue that is filled with a fluid. This fluid is most often the result of inflammation, but it is not pus. They are surrounded by a connective tissue membrane that gives them stability. This allows them to grow without the liquid spreading.
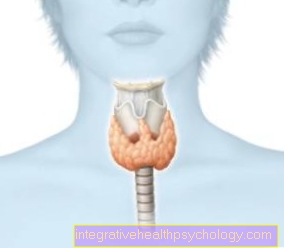
Jaw cysts are specifically those that are located in the jawbone, in the mouth or in the soft tissues such as ligaments and muscles in the jaw area. These displace neighboring structures such as bones or even tooth roots. Usually it does not cause pain, which is why it remains undetected for a long time. There is often palpable swelling in the mouth, but this does not cause any pain. Even larger cysts only cause pain if, for example, they press and move neighboring teeth. However, if bacteria come into play, which leads to inflammation, this also leads to pain.

Causes of a jaw cyst
There are also different causes for different types of cysts. One distinguishes odontogenic and non-odontogenic Cysts. So cysts caused by the tooth or not caused by the tooth.
The simplest cause is the inflammation of the nerve in the tooth. If the pulp (the inner life of the tooth) is inflamed, it swells. Since the nerve canal is limited in one direction by the tooth, there is only the possibility of emptying the pus through the opening at the tip of the root. A rounded cavity then forms around the tip.
Another cause is developmental. With wisdom teeth in particular, problems often arise during maturation in the bone. Wisdom teeth have their roots very close to the nerve canal so that the tips of the roots can press on the nerve. In response, the body reacts by creating a cyst.
More rarely, a small injury to the gum leads to inflammation of the gums and also small cysts. However, these are very small and initially only in the soft tissue.
A foreign body can also be the cause of a cyst. This foreign body could for example be a Titanium implant be. But that only happens very rarely. Mostly they are small fragments of bone or tooth root remnants that have somehow dispersed in the jaw area. They are recognized as foreign by the body and trigger an immune response.
Learn more about this under:
- Root inflammation
- Inflammation of the wisdom tooth
Symptoms
A paradox symptom is that you don't notice anything at first. As long as the cysts are small, there are no symptoms for the time being. There is accompanying pain when larger cysts push the tooth roots to the side. There is then a feeling of pressure. Patients describe the feeling as if the tooth was being pushed out of the tooth socket.
It is not uncommon for headaches to occur because of the close connection between the jaw and the head. If the cyst does not press against a tooth but against the nerve, for example in the lower jaw, typical nerve pain occurs. The region there is very sensitive to touch, the cheeks may be reddened and warmed up, as with an inflammation.
If the jaw cyst is accompanied by bacteria and inflammation, the signs of inflammation are more obvious: Dull pain, swelling, redness, warmth and Malfunctions. For example, you can no longer chew. An abscess in the jaw can also occur.
Swelling in and outside of the mouth can lead to numbness of the skin and mucous membranes as they pinch off the nerves there.
An accompanying symptom with radicular cysts is the pulsating pain of a tooth region, this is due to an acute pulpitis.
What pain do jaw cysts cause?
The cyst shows a tendency to spread and fills more and more with secretion, which leads to an increase in pressure. Symptomatic of this is severe pressure pain.
Sometimes the patient has the feeling that the tissue around the tooth is throbbing and heated. There may also be severe swelling with reddening. The tooth and the tissue are very sensitive to touch and biting open can lead to severe pain as the tooth presses into the cystic tissue.
The pain of the cyst can also radiate into anatomically close structures, which can lead to neck pain, headaches and also ear pain.
If the cyst does not start directly from a tooth or is not in the vicinity of a nerve, it can also grow completely painless and only be noticed as an incidental finding on X-rays.
You can read more here: Toothache
Inflammation of the jaw cyst
A preexisting cyst in the jaw can become infected due to bacterial infection. The tissue around the cyst is already heavily stressed and irritated, so that microorganisms can easily cause an inflammatory reaction. As part of the pus formation of an encapsulated inflammation, an abscess develops, so that the boundaries between abscess and cyst in the jaw become blurred.
The other way around applies: Cysts in the area of the jaw are mostly triggered by chronic inflammation of the teeth. The main cause is the inflammation of the nerve tissue. This can cause the so-called radicular cyst, which is accompanied by swelling, tenderness and reddening of the surrounding tissue. The tooth is sensitive to knocking and can cause pain when chewing.
However, it is more likely than a cyst to develop an abscess around the tip of the root of the infected tooth.
Read more on the topic: Inflammation of the jaw
therapy
There are two ways to treat a cyst. Once by means of a Cystectomy and once by one Cystostomy.
In a cystectomy, the cyst is completely removed, i.e. cut out. In the cystostomy, one cyst wall is removed and the others are left in place. The cyst bellows are also retained. This cyst cavity is left open so that everything that is reproduced can drain away again. In this way the cavity can grow over again with bone and gradually reduce it. If this opening is missing, the cyst will begin to grow again.
This cannot happen with cytectomy. The disadvantage here is that any neighboring structures are also removed.
Therefore, the complete removal of large cysts by means of cystectomy is not possible. The risk of a broken bone would be too great. In the case of cysts in the lower jaw, a cystostomy is also used so as not to endanger the large nerve. The same happens with cysts in the anterior region. To protect the nasal floor, all you have to do is window the cyst and leave the rest of the cyst, including the cyst bellows.
More information can be found here: Cystectomy on the tooth
When do you need an operation?
Any cyst should normally be treated. Depending on what you call it, every dental procedure that uses a knife is a minor operation. It is difficult to generalize, however, when you need an operation with general anesthesia. Such operations are carried out by very well trained oral and maxillofacial surgeons. Every doctor has different preferences and experiences, so different doctors make different decisions.
Major surgery is necessary if the area around the cyst cannot be numbed by local anesthesia and therefore general anesthesia is necessary. This should also be used if access to the cyst is so difficult that neighboring structures have to be paralyzed. In the majority of cases, however, local anesthesia is sufficient.
Learn more about: General anesthesia at the dentist
How does the operation work?
The operation of a jaw cyst differs depending on the surgical technique and size of the cyst.
Small cysts are treated by a cystectomy, which means that the entire cyst, including the cyst follicle, is removed and the bone is peeled off. The cyst contents and all of the cystic tissue are sent to pathology for a confirmed microscopic diagnosis.
The now existing hole in the jawbone must be filled. This can be done either with bone substitute materials or with a so-called obturator.
The obturator is a plastic cover made on the model that serves as a placeholder. Because the soft tissue heals faster, it can happen that the wound is superficially closed by the oral mucosa, while in the depth no bone has yet formed and a cavity remains. The obturator prevents this by being continuously reduced in size by the dentist so that pieces of bone can be reproduced.
It is extremely rare for a cyst to be so small that the cavity does not need to be filled after removal.
This surgical technique cannot be used with large cysts, as otherwise the bone defect is too large. For large cysts, a cystostomy is done first. This means that the cyst is being windowed. The secretion drains, the cyst shrinks and the pressure drops. In addition, medical inserts are inserted so that the cavity is disinfected.
In a second therapy step, the reduced cyst is now cystectomized. If the tooth was the cause of the cyst and, due to the size of the cyst, it no longer has an anchorage, this must also be removed.
An obturator can also be useful for a cystostomy.
Duration of the operation
Surgery on a cyst can be done either under local or general anesthesia.
A cystostomy is usually done under local anesthesia and takes about half an hour.
With cystectomies, the duration can vary. While small cysts can also be removed under local anesthesia in half an hour to three quarters of an hour, the procedure for large cysts takes longer. These can then be removed under general anesthesia. The procedure can then take one to two hours, depending on the size of the cyst and the type of reconstruction.
How long are you on sick leave after an operation?
After surgery to remove the cyst, the body has to recover from the procedure. A sick leave is usually issued between two and seven days and the patient has to come in for a daily check-up. The swelling and the healing process are checked in order to quickly identify any complications that may arise in the healing process. If the wound healing is impaired, the sick leave will be extended.
Patients with a physically demanding job can also be on sick leave for up to two weeks so that early stress does not negatively affect healing.
Homeopathy for a jaw cyst
There is little in homeopathy to treat a jaw cyst. Homeopathic Advisor recommend Potassium Chloratum in potencies D6 and D12. However, it is not possible to remove the cyst with globules alone. Unfortunately, cysts have to be surgically removed or cut open. There is no such thing as a globule preparation that removes a liquid by piercing a membrane.
Homeopathics are recommended for additional therapy. Either to relieve pain or to calm down. Arnica globules are supposed to reduce pain at the dentist's after the operation, allow the inflammation to heal more quickly and accelerate the healing process. There are also homeopathic remedies for prevention that are supposed to prevent inflammation or improve oral hygiene.
Prognosis and healing of a cyst
Since cysts are benign in origin, the prognosis for healing is very good. Depending on how the cyst is treated, it can relapse.
The cyst could refill. This is more likely to be the case if the cyst is incorrect "cystostomized“, That is, cut open and kept open. The process is then disturbed again and fluid continues to get into the interior of the cyst - that is, it grows again.
At a Cystectomy (Removal) the complete cyst with all structures is removed. At this point, this old cyst poses no new danger. So if small cysts are treated correctly and early enough, they will heal very well. Since they grow very slowly, they should be noticed during regular checks and recognized at an early stage. Even if they are larger, the damage is reversible, provided the neighboring structures are intact.
How dangerous can a jaw cyst get?
The risk of a jaw cyst should not be underestimated. Although they are benign growths, depending on where they are, they can displace, crush or similar other structures. As described above, they are cavities filled with liquid. These cavities are, however, newly created. So they develop where other structures should actually be. If such a cyst were in the lower jaw, it could press on the large conduction nerve and possibly damage it. Also, some cysts can cause bone damage if left untreated. The result could be a broken jaw. Another aspect is the inflammation that the cyst brings with it. This inflammation can spread and infect other jaw areas and teeth.
Read more about this under: Broken jaw
Can jaw cysts also be malignant?
In general, jaw cysts are benign. However, patients who have already had a cyst in their jaw are at greater risk of developing malignant changes.
There is also a form of jaw cyst called a keratocyst or KZOT (keratocystic odontogenic tumor), which is classified as a tumor due to its destructive and aggressive growth.
The keratocyst is the most common odontogenic tumor and affects patients between 10 and 30 and 50 and 70 years of age. It is characterized by the destruction of the surrounding bone and can also affect the surrounding soft tissue, but it is also one of the benign tumors. It is important to treat and remove jaw cysts as quickly as possible so that the tissue cannot degenerate and a tumorous structure can develop from the cystic one.
diagnosis
Very experienced dentists or oral surgeons can certainly feel a cyst manually. However, a clear diagnosis can only be made using an X-ray. Where exactly the cyst is located gives an idea of what type of cyst it is.
Only when it has been removed can the exact type be determined under the microscope. It is important that even with the slightest guess, a sample is taken and sent to the laboratory. This is to ensure that it is a benign cyst and not a possibly malignant tumor.
Is it a radicular cyst, which originates from an inflamed nerve canal, the sensitivity of the tooth is checked beforehand. If the tooth reacts extremely sensitively to the cold spray, this indicates pulpitis (inflammation of the tooth pulp). A small cyst at the tip of the root can be expected even without an X-ray.
X-ray cysts of the jaw
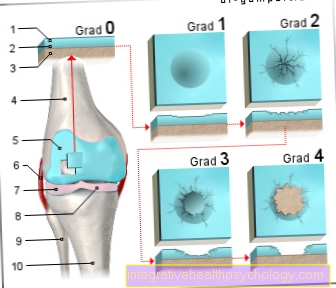
When it comes to cysts, the X-ray is the most important tool for the dentist. Cysts can only be detected at an early stage through imaging. In the X-ray image, those structures through which the X-rays pass are shown in black or dark. Since the cysts are cavities that may be filled with fluid, they usually appear sharply defined as a dark spot within the lighter bone structure.
Depending on the location, conclusions can be drawn about the type of cyst. A form of therapy can only be selected after viewing the X-ray image and assessing the size.
Learn more at: X-ray of teeth
What types of jaw cysts are there?
A main distinction is made between cysts that originate from the tooth itself or not from the tooth.
Non-tooth related cysts are for example nasolabial or nasopalatal cysts. They arise in the area of the palate and nose and consist of tissue remnants that have not completely disappeared during development.
Cysts that arise from the tooth are:
- Keratocyst: develops where the tooth should actually be formed
- Eruption cyst: on broken milk teeth
- Periodontal cyst: wisdom teeth erupting on the tooth support apparatus
- Follicular cyst: teeth not fully developed on the crown of the tooth
- radicular cyst: on inflamed tooth root tips
- Residual cyst: Leftover cyst after tooth extraction
- glandular odontogenic cyst: in the maxillary and mandibular bones, often recurring
- Pseudocyst: has no surrounding connective tissue membrane, its origin is not yet known exactly
Duration of creation
There is no clear time for the creation. Firstly, the different cysts have different origins and, secondly, the formation of a cyst depends on what tooth it is, what oral hygiene is like, or how the jaw is stressed.
It is clear that cysts grow relatively slowly and therefore remain undetected for a long time. So it can develop over years and only becomes visible when it is of a certain size.
Recommendations from our editorial team
- Cystostomy
- Cystectomy
- Lower jaw pain
- Upper jaw pain
- Abscess in the lower jaw