leukemia
Synonyms in a broader sense
- White blood cancer
- myeloid leukemia
- lymphatic leukemia
- ALL (Acute Lymphatic Leukemia)
- AML (Acute Myeloid Leukemia)
- CLL (Chronic Lymphatic Leukemia)
- CML (Chronic Myeloid Leukemia)
- Meningeosis leucaemica
You can find more information under our topic: Diseases in the blood

definition
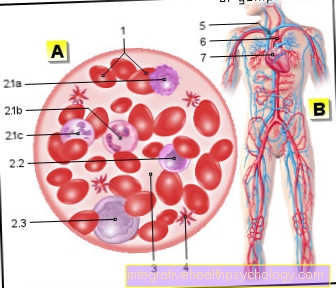
The white blood cancer (leukemia) is not to be understood as a single disease, but is a collective term for several diseases. This means a malignant (malignant) growth (proliferation) of the blood cell-forming system that is uncontrolled by the body. This leads to malignant growth of the affected cells in the Bone marrow or in the so-called lymphatic tissues, e.g. in the Lymph nodes. These degenerate cells are washed out into the blood. The uncontrolled growth or multiplication of these cells leads to a suppression of the "normal" blood formation and an impairment of the Immune system, because the healthy, non-degenerate cells are literally crushed by the rapid growth of the malignant cells.
The term leukemia means “white blood”. It was then Rudolph Virchow, a well-known German physician who analyzed the blood of an affected patient as early as the 19th century and saw in the test tube that the white blood cells were atypically increased and thus coined the term.
General symptoms
The symptoms are often very atypical. The illness can start with a fever, for example. In the course can Night sweats to be added. The duvets are then downright wet in the morning.
Bone pain is also often described. Children are often noticed by reluctance to play or generally by a change in their character; they lose interest in things that used to be very exciting for them, are rather lethargic and exhausted. The uncontrolled growth of the degenerate cells displaces the normal growth of the cells that are important for the immune system, so symptoms appear that relate to the increased susceptibility to infections are due, so more frequent Pneumonia for example.
In addition, the normal growth of red blood cells (erythrocytes) is suppressed. The consequence is one Anemia (anemia), but also Chest tightness (Angina pectoris) or Palpitations (Palpitations) are among the symptoms. If the increase in blood platelets (thrombocytes) is prevented or restricted, increased bleeding will result, even after minor activities such as Brush teeth for example. The reason is the central role of platelets in blood clotting. If these cells are too few (e.g. below 50,000 / µl), adequate hemostasis cannot be guaranteed.
Other symptoms can include enlargement of the lymph glands. The spleen can swell. Especially with ALL (acute lymphatic leukemia), the meninges (so-called. Meningeosis leucaemica) become infected.
The kidney can fail (Kidney failure), because it is literally overrun by the increased cell turnover and the accumulating waste materials that it has to dispose of and thus places it next to the Cerebral hemorrhage and serious infections are one of the main causes of death.
How do you recognize leukemia?
Leukemia is not always easy to spot. As a rule, there are no “typical” symptoms! All complaints can also occur in the context of significantly less dramatic, but more frequent clinical pictures.
They are therefore not proof of the presence of blood cancer. If symptoms persist, you should still consult your doctor for clarification.
The following symptoms can help identify leukemia:
-
Flu-like symptoms, such as weakness, fever, body aches, etc.
-
Night sweats, weight loss, fatigue
-
Increased tendency to infection
-
Signs of bleeding, such as frequent bruises, bleeding from the mucous membrane, nosebleeds or punctiform skin bleeding
-
paleness
-
Bone pain without a clear localization
-
Headache, flashes of light, visual disturbances
-
Upper abdominal pain
- Neck stiffness
Read more on this topic at: How do you recognize leukemia? and bone marrow aspiration
Is Leukemia Curable?
In principle, the question of the curability of leukemia is not that easy to answer. For one, there is a lot many different shapes of leukemia. They differ both in therapy and in their curability. On the other hand, many individual factors decide how Patient age or genetic changes, about a therapeutic success.
Basically, however:
Acute leukemia can in principle be cured. Nowadays, acute lymphoblastic leukemia, or ALL, has very good prospects of a cure, especially in children.
Chronic leukemia however, are usually only curable by a bone marrow transplant. Chemotherapy alone is not enough here. Nevertheless, they are usually less aggressive than acute forms, so that those affected can live well with the disease even without a permanent cure.
In addition, there is constant change in leukemia therapy due to modern studies!
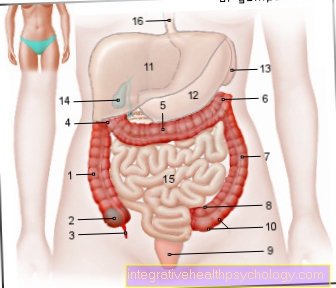
Classification of leukemia

The human blood formation system is structured hierarchically. From a so-called stem cell, several rows of cells develop in several intermediate stages, until the mature white blood cell (leukocyte) or the mature red blood cell (erythrocyte) emerges. As with a "normal" tumor, e.g. Breast cancer or colon cancer, which is based on degenerate cells, can also degenerate these cells in the various stages of development or intermediate stages and uncontrolled, i.e. not adapted to the needs of the body, they grow and thus displace other cell lines. These excessively produced cells are unable to function.
The maturation of a cell is called differentiation. Leukemia are i.a. classified according to their distinguishing features. The degenerated cells can come from a so-called myeloid or a so-called lymphatic precursor cell. The myeloid cell series (starting from the bone marrow) contains the precursor cells of the red blood cells (erythrocytes), the blood platelets (thrombocytes) and the granulocytes, which play an extremely important role in the defense against pathogens such as bacteria and owe their name to the property that they have so-called granules in their cell bodies, which contain substances necessary for the defense. The term lymphatic means that the cells of the affected leukemia are degenerate precursor cells of the mature lymph cells (lymphocytes).
Another classification system is the degree of maturity of the affected cells, i.e. whether mature (late developmental stages) or immature (early developmental stages) cells are degenerate. It is also important for the classification whether the disease shows an acute course, e.g. appeared and got worse within a few weeks or months, or whether it was more of a chronic, slow course. However, the latter classification is no longer used frequently. Nevertheless, this classification is very helpful for understanding, because the acute leukemias usually start from immature cells, which are then all the more ineffective, while the chronic leukemias originate from mature cell precursors. The most common and well-known leukemias are ALL (acute lymphatic leukemia), AML (acute myeloid leukemia), CLL (chronic lymphatic leukemia) and CML (chronic myeloid leukemia).
Acute myeloid leukemia (AML)
AML is an abbreviation and stands for acute myeloid leukemia. It is the most common form of leukemia in adulthood. In Germany, 3.5 new diagnoses per 100,000 inhabitants are made every year. This makes the AML one of the rare diseases.
Their origin finds the disease in the blood-forming cells of the bone marrow. Normally, our blood cells are formed there in complicated steps and sequences. In AML, the process gets out of balance and individual, "degenerate" cells multiply in an uncontrolled manner. As a result, the blood becomes flooded with immature, dysfunctional leukemia cells. If Cells from the myeloid series degenerate, one speaks of AML. These cells include the red blood cells (Erythrocytes), Platelets (Platelets) and parts of the white blood cells (Leukocytes). The cause of the disease is largely unclear, but radiation exposure and individual chemical substances play an important role.
In addition to rather nonspecific, flu-like symptoms, suffer from an increased susceptibility to infections, chronic fatigue, weakness or paleness. Often, an accumulated number of bruises, nosebleeds and small skin hemorrhages can be observed. In principle, however, the leukemia cells can attack all organs and accordingly cause various symptoms. The leading finding is the presence of leukemia cells, also called blasts, in the blood and / or bone marrow. Often times, platelets and red blood cells are severely low at diagnosis.
Like all acute forms of blood cancer, AML is one very aggressive disease. Thus is a immediate start of treatment is essential! To achieve a complete destruction of the leukemia cells, various Chemotherapy drugs combined with each other. One then speaks of polychemotherapy. In certain cases a Bone marrow transplant increase the prospect of healing.
Numerous occur under therapy Side effects on. These can include nausea, vomiting, hair loss, inflammation of the oral mucosa or infections.
The Healing prospects the AML vary and are i.a. depends on the stage of the disease, form and age of the patient.
Chronic lymphocytic leukemia (CLL)
CLL stands for chronic lymphocytic leukemia. Around 18,000 people in Germany suffer from the disease. Typically get sick elderly to CLL. The mean age for diagnosis is between 70 and 72 years.
The cause of CLL lies in the uncontrolled growth of B lymphocytes, a subgroup of white blood cells. In contrast to healthy white blood cells, the diseased B-lymphocytes have a significantly longer survival time. As a result, the functionless leukemia cells “flood” the blood system and infiltrate organs, especially lymph nodes, spleen and liver.
CLL runs in about half of the cases unnoticed for a long time and without symptoms. Often the disease is discovered only by chance! Possible, rather unspecific complaints Fatigue, fever, weight loss, or night sweats be. Painless lymph node swellings, chronic itching or hives can be observed in many patients. Most serious, a disease-related restriction of the immune system can be. Severe bacterial or viral Infections can be the result.
Diagnostic A sustained increase in lymphocytes and the typical appearance of leukemia cells under the microscope are groundbreaking. Further examinations, such as an ultrasound of the abdomen or a biopsy of the lymph nodes, may support the diagnosis.
As far as we know today, CLL cannot be cured without a bone marrow transplant. The tumor cells divide very slowly, which is why the disease progresses slowly. It is therefore sufficient to begin with regular check-ups. In advanced stages one comes medication for use. It consists of a combination of chemotherapy and antibodies.
Basically, the patient's age and general condition determine the type of therapy. This is how symptomatic CLL is always treated. If the diagnosis is made by chance and those affected are symptom-free, treatment can be dispensed with.
Chronic myeloid leukemia (CML)
Chronic myeloid leukemia, or CML for short, is one rare form of blood cancer. So every year only 1-2 people / 100,000 inhabitants fall ill.
In principle, people of any age group can get sick. Nevertheless, there is an accumulation between the 50 and 60 years of age observe.
Interestingly, the CML is based on a typical genetic change. Because in almost all CML patients the so-called "Philadelphia chromosome“Prove.
Like all forms of leukemia, CML has its origin in the blood-forming cells of the bone marrow. Typically, the disease causes one uninhibited reproduction of granulocytes, a subtype of white blood cells.
In contrast to acute leukemia, the CML proceeds slowly and begins with creeping complaints. Overall, the course can be seen in 3 phases subdivide:
- Chronic phase: The diagnosis is often made in this phase. It is often "silent" and can last up to 10 years. Typical symptoms can be chronic fatigue, weight loss or night sweats. Patients often complain of upper abdominal pain, which can be explained by a strong liver and spleen enlargement.
- Acceleration phase: This leads to a deterioration in the blood count. Affected people can suffer from anemia, bleeding tendencies and heart attacks.
- Blast crisis: The blast crisis is the end stage of CML and resembles the severe symptoms of acute leukemia.
First and foremost, the massively increased number of granulocytes leads to the symptoms of CML. As part of the therapy, therefore, the aim is to lower these blood cells. Both come Chemotherapy drugs, as well as modern ones antibody for use. After diagnosis, mild cytostatics are often sufficient, so that patients rarely have to expect serious side effects.
In order to closely monitor the blood count changes, CML patients must closely controlled become. If the disease progresses, a Bone marrow transplant should be considered.
causes
Ionizing rays: After the nuclear bomb attacks in Japan and after the nuclear reactor accident in Chernobyl, an increased incidence of ALL (acute lymphatic leukemia) and AML (acute myeloid leukemia) was observed.
Smoking: It is primarily a risk factor for AML (acute myeloid leukemia)
Benzene: It is also a risk factor for the development of leukemia. It is also found in cigarette smoke.
Heredity (genetics): In Down syndrome (trisomy 21 syndrome), an increased number of new cases of leukemia can be observed.
You can find more information about trisomy 21 under our topic Down syndrome.
Chemotherapeutic agents: When chemotherapeutic agents have been used for many years to treat other types of cancer, the risk of developing blood cancer increases, as the substances used also severely impair the blood formation system and can thus trigger degeneration in the cells.
Viruses: The so-called HTLV (Human t-cell leucaemia virus, German: Human T-cell leukemia virus) I and II viruses pose an increased risk of the development of certain types of leukemia, especially in regions such as the Caribbean or Japan. In addition, the so-called EBV (Ebstein Barr Virus) is a possible trigger for certain forms of leukemia.
Irregularities in the gene carriers in the cell (chromosomal aberrations): One of the most well-known irregularities in the gene carriers (chromosomes), which can lead to leukemia, especially CML (chronic myeloid leukemia), is the atypical connection (translocation) of chromosomes 9 and 22. The so-called Philadelphia chromosome is created. A certain protein molecule (tyrosine kinase) then, due to this atypical connection (translocation), causes the affected cells to multiply uncontrollably.
Find out all about the topic here: The tyrosine kinase.
therapy
The therapy that is tailored to the patient must be created for each patient. The exact treatment options for the individual forms of leukemia are dealt with in the relevant sections. General therapy options for leukemia are presented here.
One of the most important therapeutic options is chemotherapy, in which growth-inhibiting substances (cytostatics) are used to stop the uncontrolled growth of the affected cells. The so-called high-dose chemotherapy is a further, special possibility of therapy, which is based on the following principle: The “normal” chemotherapy administered is limited in its dose, as it also destroys healthy cells of the bone marrow, because the drugs administered not only destroy the degenerate cells are destroyed, but all cells that divide very quickly, including healthy cells of the blood-forming system in the bone marrow.
In the procedure of the so-called allogeneic (foreign donor) bone marrow transplantation, the patient is first given a high dose chemotherapy, with the knowledge and of course the risk of destroying most of the healthy cells in addition to the malignant cells. At the highest level of isolation for the patient, who is now extremely susceptible to infection, suitable external donor stem cells from the blood-forming system are administered so that new, healthy blood cells can form again (see: stem cell donation). In some studies, the benefit of so-called autologous stem cell transplantation was examined, whereby healthy stem cells are taken from the patient even before the high-dose chemotherapy, which are then used again after the high-dose chemotherapy. It has the advantage that these are the body's own cells and would not be rejected. The disadvantage is the lack of clinical experience and knowledge as it is a very new procedure.
Radiation therapy plays a rather subordinate role in the treatment of leukemia.
In recent years more and more direct-acting drugs have been developed. These substances specifically target the cause of uncontrolled cell growth. The best-known drug of this type is imatinib (Glivec®), which specifically inhibits the product of the atypical connection (translocation) between the gene carriers (chromosomes) 9 and 22, the tyrosine kinase, and thus acts directly at the defective site and thus non-diseased cells does not attack.
With the introduction of the tyrosine kinase inhibitor, the prognosis of leukemia could be improved considerably. If you would like to find out more about this chemotherapy and are interested in its effects and side effects, we recommend our website: Targeted chemotherapy with tyrosine kinase inhibitors
Leukemia in children
With around 700 new cases per year, leukemia is the most common cancer in children and adolescents. The majority of children suffer from acute lymphoblastic leukemia, or ALL for short. In the vast majority of cases, the cause of childhood leukemia cannot be clarified. However, genetic changes and individual environmental influences, such as increased radiation exposure, increase the risk of disease. Children with Down syndrome are also significantly more likely to develop a certain form of leukemia (AML).
Leukemia has its origin in the blood-forming cells of the bone marrow. Normally, our various blood cells mature there in complicated processes. In leukemia, individual progenitor cells “degenerate”. As a result, they uncontrollably produce large quantities of functionless leukemia cells (Blasts). Increasingly, healthy blood cells are then displaced and the blood cancer cells infiltrated into various organs.
Similar to adults, the first symptoms in children are rather unspecific. Affected children are weak, tired and often listless. Smaller patients no longer want to play and sometimes behave. very affectionate. Parents often notice that their child is very paleness, as well as an accumulation of bruises or punctiform skin hemorrhages. Occasionally, profuse nosebleeds can be observed. Since the leukemia cells displace the immune defense cells (white blood cells), the children suffer from frequent infections.
If leukemia is suspected, specialized departments of children's clinics (Pediatric oncology / hematology) a bone marrow sample is taken. There the leukemia cells can be made directly visible under the microscope. In addition to bone marrow aspiration, other examinations also play a role, such as Blood collection, ultrasound or lumbar puncture (Cerebral fluid examination), an important role.
Since acute leukemia is very aggressive even in children, therapy should begin as soon as possible. In order to destroy as many leukemia cells as possible, a therapy combination of various chemotherapeutic agents is used.
The strong and aggressive therapy has numerous side effects (nausea, hair loss, vomiting, susceptibility to infection).
In special cases, a bone marrow transplant can increase the chances of recovery.
Radiation therapy is occasionally carried out. Fortunately, the chances of a cure for leukemia in children have improved significantly over the past few decades. The 5-year survival rate of the common ALL is between 80 and 90%.
Read more about this under: Childhood leukemia
frequency
The individual frequencies of the various forms of leukemia are listed in the corresponding sections. In general, it should be emphasized that some forms of leukemia occur more frequently in certain age groups. For example, the ALL (Acute Lymphatic Leukemia) especially in childhood, while it is a rarity in adults. The CLL (Chronic Lymphatic Leukemia) however, it is extremely rare in children and occurs mainly in older (over 60 years) patients. The AML (Acute Myeloid Leukemia) is the most common leukemia in adults and is also relatively common in children (after ALL, the second most common childhood leukemia).
You can find more information on this topic here: Leukemia in children