Knee Pain - What Do I Have?
- Anatomy of the knee joint
- Front knee pain
- External knee pain
- Popliteal pain
- Pain that affects the whole knee
Synonyms in a broader sense
Knee pain, knee joint pain, meniscus damage, cruciate ligament tear, knee osteoarthritis
introduction
Knee joint pain can have very different causes. When looking for the correct diagnosis, the following are important:
- Age
- gender
- Accident event
- Type and quality of pain (stabbing, dull, etc.)
- Pain development (slowly, suddenly, etc.)
- Onset of pain (at rest, after / during exercise)
- Location of pain (inside, outside, etc.)
- external aspects (swelling, redness, etc.)
- and much more
The pain in the knee can be caused by problems with the joint itself or by clinical pictures that damage the tissues such as ligaments, tendons or bursa that surround the joint. In any case, knee pain is a very stressful symptom for those affected, which should be treated as adequately as possible. The treatment for knee pain always depends on the diagnosis.
Find out more about: Acute knee pain - that may be behind it

causes
In general, a distinction must be made between whether the knee joint itself has been damaged and therefore causes pain, or whether the knee pain has another cause, for example due to a previous infection. Knee joint pain can have very different causes, with some being more common than others. A few should be presented here. However, the attending physician must always make the individual diagnosis after a detailed examination.
One of the most common causes of knee pain is injury and associated damage to structures. The meniscus, the cartilage of the knee joint, is often affected. However, the ligaments can also be affected in the form of strains or ligament tears. A common sports injury is a torn cruciate ligament (usually the anterior cruciate ligament), or a tear in one of the collateral ligaments.
Another major cause of knee pain is inflammation. It is important to distinguish whether it is a bacterial or non-bacterial disease.
- If there is a bacterial infection, it is usually accompanied by the usual signs of inflammation. The knee joint is warm, reddened, swollen, painful and restricted in its function. The infection can also be accompanied by systemic fever.
- Non-bacterial inflammations can be roughly divided into knee osteoarthritis and rheumatism. Rheumatic inflammatory diseases of the knee joint are caused by the immune system's defense against the body's own tissue. The most common rheumatoid disease is rheumatoid arthritis, which can also affect the knee. But ankylosing spondylitis, psoriatic arthritis, lupus erythematosus and some other diseases also belong to this type. They all have in common that they can destroy the joint and even attack the bone.
Osteoarthritis is a symptom of wear and tear that most commonly affects the knee joint. Osteoarthritis can be divided into primary and secondary. Primarily, if the structure of the cartilage tissue wears out more easily than in healthy people, or secondarily if the wear and tear is due to mechanical stress or a metabolic cause (pseudogout, see chondrocalcinosis). In osteoarthritis, too, cartilage is initially damaged and the bones are attacked as the disease progresses.
Also read:
- Growing pains in the knee
- Periosteum inflammation on the knee

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Knee pain on the inside
Depending on the underlying disease, the pain felt by the patient can be seen on the knee either at the Outside or on the inside. In addition, pain in the knee can also be in the area of the Kneecap or in the Hollow of the knee occur.
Pain in the knee, which is mainly localized on the inside, can indicate damage to the Medial meniscus Clues. Under the term meniscus one understands a cartilaginous structure, which within the Knee joint serves for stabilization and pressure relief.
In the knee joint, a distinction is made between an inner and a External meniscus. In a comparison between the two menisci of the knee joint, damage occurs primarily in the area of the inner meniscus. An impairment of the inner meniscus manifests itself primarily through the sudden onset of pain on the inside of the knee. In addition, the affected knee can only move to a limited extent.
The most common conditions that cause pain on the inside of the knee are traumatic changes in the meniscus (for example the Meniscal tear) and degenerative diseases. The traumatic impairment of the knee joint is typically caused by a Twist of the knee in connection with a pressure load on the middle of the joint as well as rotational forces. A traumatic change in the knee joint that causes pain on the inside of the knee is often associated with one Torn anterior cruciate ligament on.
In contrast to the traumatic changes in the area of the meniscus, the pain on the inside of the knee is more likely to occur in the presence of a degenerative disease creeping on. The pain on the inside of the knee felt by the affected patient is mainly due to the fact that there is constant friction between the joint structures due to the broken meniscus. This friction leads to very quickly in most cases complex cartilage damage. In addition to the pain on the inside of the knee, the affected patients usually notice significant pain Swelling and Entrapment symptoms on the cartilage surfaces. The pain that is typical of damage to the medial meniscus is usually particularly evident in stressful situations (Exercise pain). However, as the underlying disease progresses, it can become more obvious Exercise pain occur.
In the long run, the damage to the medial meniscus can even lead to the formation of a arthrosis favor. In addition, the pathological changes in the Pressure distribution provoke the formation of a cyst at the base of the meniscus within the knee. The Diagnosis if there is pain in the inside of the knee involves several steps. In addition to performing an extensive Doctor-patient conversation, in which the present complaints should be described as precisely as possible, the examination of the knee joint also plays a role Side comparison a crucial role. In the presence of a meniscal tear, various Testing help to secure the suspected diagnosis. They are also common imaging procedures (especially X-rays and Magnetic resonance imaging) arranged. Depending on the underlying disease, appropriate treatment should be initiated immediately after the diagnosis has been completed. The main goals of this treatment include both relieving the pain on the inside of the knee and correcting the compromised meniscus.

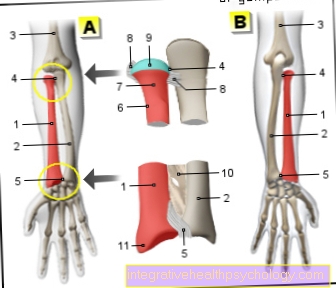
A - Right knee joint from the front
- Inner thigh muscle -
Vastus medialis muscle - Femur -
Femur - Kneecap -
patella - Inner meniscus -
Meniscus medialis - Inner band -
Ligamentum collaterale tibiale - Internal calf muscle
Gastrocnemius muscle,
Caput mediale - Shin -
Tibia
a - Inner ligament injury
(Inner ligament tear)
b - tear of the medial meniscus
c - medial
(internal) knee osteoarthritis
You can find an overview of all Dr-Gumpert images at: medical illustrations
Knee pain on the outside
Knee pain, which is mainly external, can have various causes. With such pain symptoms, both the knee joint and its ligaments, as well as the cartilage or the tendons can be affected. Pain in the knee, which is mainly felt outside, is often caused by excessive strain. Above all, the so-called "runner's knee" (tractus syndrome) plays a decisive role in this context. In the affected patients, there is a significant overstrain in the area of the fascia strip that pulls down from the iliac bone on the outside of the thigh. The development of the runner's knee, which leads to pain on the outside of the knee, is favored by a misalignment of the leg axis (bow legs). In addition, a weakness in the pelvic stabilizers can encourage the runner's knee to appear. The affected patients typically experience sharp pain, which is mainly felt on the outside of the knee. The symptoms caused by the runner's knee are often so pronounced that running becomes almost impossible. In many cases this pain occurs primarily in stressful situations. Since the fascia plate affected by this disease extends to the outside of the head of the tibia, the pain on the outside of the knee usually radiates to the head of the tibia.
The runner's knee is treated with what is known as "cryotherapy" (Cool) and anti-inflammatory ointments. In addition, the affected patients should stop any sporting activity until the symptoms have completely subsided. Furthermore, damage to the tendons or osteoarthritis can lead to pain on the outside of the knee. The technical term for osteoarthritis of the knee is "gonarthrosis". This term is understood to mean a slowly progressing, non-inflammatory change in the knee joint that leads to increasing destruction of the cartilage structures. Osteoarthritis of the knee is one of the most common causes of pain on the outside of the knee and affects around 30 to 60 percent of people over 60 years of age. The reason for the development of knee osteoarthritis is in most cases excessive or improper loading that has persisted for years. In addition, inflammatory processes in the knee joint and overweight (obesity) are among the most important risk factors.
Affected patients feel pain in the knee even with less pronounced forms of knee osteoarthritis, which mainly occurs on the outside. In addition, knee osteoarthritis manifests itself in many cases as a significant restriction in the range of motion of the affected knee. The pain mainly occurs when walking down or down stairs. In addition, the structural changes within the knee joint lead to pronounced instability. As the disease progresses, the stress on the individual joint parts often leads to the development of knee joint effusions.
The diagnosis of pain on the outside of the knee takes place in several steps. Already during the doctor-patient conversation (anamnese) the patient should describe the symptoms he is experiencing as precisely as possible. Following this doctor-patient conversation, the knee joint is examined from the side. During this examination, an indication of the underlying disease can usually be obtained. Further diagnosis of pain on the outside of the knee is carried out using various imaging methods. Both the production of X-rays and the implementation of a magnetic resonance tomography can help to secure the suspected diagnosis. The treatment of a patient with pain on the outside of the knee depends primarily on the underlying disease.
In this context, possible risk factors (for example being overweight) to clear out.
Read more about this topic at: Pain on the outside of the knee
Fig. External knee pain
Knee pain in the front
Pain in the knee, which can mainly be seen in the front, both through a direct damage of the anterior parts of the knee, as well as by a continuation when other structures are impaired. Possible causes for the development of front knee pain can be in the area of the Kneecap to be found.
A typical clinical picture that leads to pain in the front of the knee in the affected patient is the so-called Kneecap arthrosis (Retropatellar arthrosis). In this disease the symptoms are immediately referred to as Pain behind the kneecap perceived.
In this case, the cause of the discomfort is damage in the area of the Cartilagewhich leads to friction between the individual joint parts. Kneecap arthrosis is not uncommon. In people around the age of 50, it is often associated with a general knee osteoarthritis on. Younger patients, however, often develop such cartilage damage as a result of injuries or a Congenital cartilage weakness. With this disease, the pain in the front of the knee is perceived as sharp and bright increase in intensity after exercise. Above all, the affected patients find going down stairs or downhill to be particularly painful.
Another cause of the development of front knee pain is the so-called Jumper knees (Patellar tip syndrome). In this condition, the point of greatest pain is right at the lower end of the kneecap. Cause of the occurrence of patellar tip syndrome inflammatory processes and or Overloads the patellar tendon. The pain in the front of the knee in patients with patellar tendinitis does not occur suddenly but rather more creeping on. In addition, the so-called pes anserinus attachment tendinosis, an inflammatory disease of the tendon attachments of various thigh muscles, can lead to pain in the front of the knee.
In many patients who suffer from pain in the front of the knee, a Bursitis (Prepatellar bursitis, infrapatellar bursitis) can be determined. In these cases, the greatest pain is felt just above the kneecap or along the kneecap. In addition, the symptoms caused by the inflammatory processes show one sharp, stabbing pain character and are accompanied by swelling and / or overheating of the affected knee. Usually the bursitis does not go through bacterial pathogensbut by permanent Irritation evoked.
The Diagnosis pain in the front of the knee is mainly based on the symptoms described by the patient concerned. Already during an extensive Doctor-patient conversation (anamnese) should describe these complaints as precisely as possible. In addition, the examination of the knee joint in Side comparison provide important information about the underlying disease. The further diagnosis of pain in the front of the knee is carried out by various means imaging procedures (for example roentgen or Magnetic resonance imaging of the knee). The most suitable treatment method can only be determined after a successful diagnosis. Affected patients should, however, make sure that the painful knee as possible immobilized becomes.
Knee pain in the hollow of the knee
The possible causes for the development of pain in the back of the knee can include both age-related and sport-related overload. In young patients in particular, pain in the back of the knee (pain in the hollow of the knee) is a sign of excessive exercise. In the case of older patients, however, it can be assumed that there is likely to be a wear and tear disease.
The so-called "Baker's cyst" is one of the most common signs of wear and tear in this context. The main cause of such a Baker's cyst is the increased production of synovial fluid (Synovial fluid) in the knee joint. This phenomenon can mainly be observed in people who suffer from osteoarthritis or an underlying inflammatory disease (e.g. rheumatoid arthritis). In addition, a Baker's cyst with pain on the back of the knee is particularly common in people who have had a long-standing meniscus damage. Patients who suffer from a Baker's cyst usually feel recurring pain at the back of the knee (pain in the hollow of the knee), which can radiate into the calf. In some cases, however, there is no pain, just a feeling of tension at the back of the knee. The pain in the back of the knee perceived by the affected patient may already be present at rest. Typical for the presence of a Baker's cyst, however, is the increase in complaints when the knee joint is stressed. The reason for this is the fact that the Baker's cyst swells a lot while walking and running and thus leads to increasing symptoms.
The diagnosis “Baker's cyst” with pain in the back of the knee can usually already be made by looking at the medical history, the symptoms and a short physical examination. In addition, an ultrasound examination of the hollow of the knee can help confirm the suspected diagnosis. The treatment of Baker's cyst can be non-surgical (conservative), as well as surgically. However, complete healing can almost be ruled out in patients who refuse surgical treatment of the Baker's cyst. Surgical removal of the Baker's cyst is the only measure that relieves the pain behind the knee in the long term.
Another cause of back knee pain is damage to the inner or outer meniscus. Typically, the symptoms occur when the meniscus is damaged either on the right or left rear of the knee. The pain in the back of the knee caused by a meniscus damage takes on a pulling or stabbing character and increases in intensity, especially when turning movements. Furthermore, pain at the back of the knee may be related to what is known as "biceps tendon tendinosis". Biceps tendon tendinosis is an inflammatory disease of the biceps tendon. In this case, the pain on the back of the knee perceived by the affected patient is typically load-dependent and takes on a pulling character. In addition, a thrombosis in the area of the pelvic vessels or the legs can lead to pain that radiates to the hollow of the knee. Treatment for back knee pain depends largely on the underlying condition.
Please also read: Drawing in the hollow of the knee and pain in the calf and hollow of the knee
Clinical pictures
Gonarthrosis

Gonarthosis describes the wear and tear of the cartilaginous parts of the knee joint and is also known under the term 'knee arthrosis'.
The most common cause is the limited 'shelf life' of articular cartilage: with age, the elasticity of the cartilage decreases and the joint surfaces shrink. Over time, bone changes can occur so that the original joint structure no longer exists. It is estimated that around 6% of all retirees are affected!
Axial misalignments of the legs (O / X legs), previous joint damage, e.g. In the context of meniscus or cruciate ligament injuries or being overweight are among the reasons for gonarthrosis at a young age.
Initially, patients complain of movement-dependent pain in the knee joint, which worsens over the course of the day. Furthermore, there is a so-called starting pain in the morning or after long breaks from sitting.
In the course of the disease, the symptoms gradually increase, so that in advanced cases knee pain occurs even at rest.
A significant swelling of the knee is very common. Those affected also report a 'cracking' or crunch in the joint, especially during certain movement sequences (e.g. when crouching down).
The cause and severity determine the individual therapy for gonarthrosis. The possibilities are diverse:
Physiotherapy can be used to maintain or improve mobility. Relief agents, as well as pain and anti-inflammatory drugs or ointments, provide additional relief. In severe cases, a joint prosthesis ('artificial knee joint') may be indicated.
You may also be interested in this topic: Chronic knee pain
Chronic polyarthritis
Chronic polyarthritis is a rheumatic joint disease. Due to various causes (e.g. genetic predisposition, bacteria, viruses), the joint mucosa becomes inflamed (synovitis) and swells. In addition, joint effusions are found repeatedly, i.e. Fluid collects inside the joint.
Also read on this topic: Inflammation of the synovial membrane
At this stage the knee joint is painfully swollen and overheated. The presence of a 'dancing kneecap' speaks in favor of a joint effusion: If the kneecap (patella) is pressed from the front, you can clearly feel a kind of 'springing back', also known as a rebound. Characteristic is the relapsing occurrence of complaints, including Morning stiffness.
In the course of advanced polyarthritis, the joint cartilage is destroyed. Ultimately, the joint capsule and the ligaments are also attacked. Considerable pain can limit the mobility of the knee joint to the point of total inability to walk!
There are numerous therapy options, depending on the pathogen and stage of the rheumatoid arthritis. This includes medication against the underlying rheumatic disease, physiotherapy (e.g. mud packs, thermal baths), rest, cooling and bandages. If the painful swelling does not go away despite the above measures, the inflammatory joint mucosa can be removed in an operation (synovialectomy). In the case of advanced cartilage damage, there is the possibility of a knee joint endoprosthesis.
Baker's cyst
Baker's cyst is a firm, fluid-filled tumor in the hollow of the knee, often accompanied by chronic joint effusion (e.g. in the case of chronic polyarthritis or activated knee osteoarthritis).
Those affected complain of pain and pressure in the hollow of the knee, especially when the knee is bent. When the cyst has reached a certain size, there is also the risk that vessels and nerves will be pinched off. It can become dangerous as soon as a vein comes under pressure: In the worst case, a blood clot (thrombosis) develops!
After an ultrasound, the diagnosis can usually be made with certainty. Mild discomfort can be eliminated with a pressure bandage, whereas large cysts have to be removed by surgery.
Read much more information on this topic at: Baker's cyst
Osteochondrosis dissecans
In osteochondrosis dissecans, parts of the joint surfaces are rejected. This creates small fragments, also known as the articulated mouse or dissector. What remains is a joint defect, also known as the joint bed.
It is assumed that circulatory disorders or numerous small cartilage damage lead to the death of the bone (aseptic necrosis). In addition, there seems to be a connection between ongoing loads on the knee joint, e.g. to survive in competitive sports.
In the early stages, the disease is often largely symptom-free. Movement-dependent and pressure-dependent pain only occurs as the disease progresses. If a fragment now loosens, the joint can block and a 'joint lock' occurs.
Treatment depends on age, exact location and progression of the osteochondrosis. In affected children, immobilizing the knee in a flexed position using a brace may be sufficient, provided that no fragment has loosened. In contrast, adult patients usually have to undergo an operation to ensure permanent freedom from pain.
Sinding-Larsen's disease and Osgood-Schlattter's disease are also increasingly found in children.
Bacterial gonitis
Bacterial gonitis or knee joint inflammation can lead to complete destruction of the knee joint without treatment. The germs are often brought in through unsterile work with knee joint punctures! Patients whose immune system is weakened are particularly affected, e.g. as part of chemotherapy.
In addition to swelling and pain in the knee, the inflammation leads to a general feeling of illness with fever, tiredness and an increase in white blood cells.
Therapeutically, cleaning the inflamed knee with subsequent removal of the synovial membrane is recommended. Once the pathogen has been identified, antibiotic treatment should also be started.
Meniscal tear
The meniscus tear is a common consequence of sports accidents. The meniscus is overstretched and tears due to shear forces (rotation in the knee joint, with the lower leg stationary). Particularly affected are e.g. Skier, because your foot is rigidly fixed by the ski boot.
Most of the time, the inside tears away from the two menisci, because it is firmly fused with the inner ligament and therefore has no alternative in the event of rotary movements. Typical for a meniscus tear is immediate shooting pain at the affected joint space. Furthermore, the resilience is greatly reduced, so that sporting activity has to be stopped. Patients report a kind of 'snapping' over the joint, in the worst case mobility can be blocked.
X-rays are normal for recent injuries, an MRI for a V.a. however, a tear in the meniscus or a knee examination can provide clarity.
In addition, the doctor carries out specific examinations to determine the pain provocation through the meniscus in the knee.
These meniscus tests are also called Böhler test, Payr test or Steinmann I and II test.
Read more about this topic under: Meniscus test
Surgical intervention is carried out depending on the severity of the injury. If feasible, the two ends are sewn together again using a meniscus suture. However, the standard therapy is partial removal of the injured meniscus. The entire meniscus only needs to be removed in the event of extensive injury. However, this total menisectomy should be viewed critically, as it can cause osteoarthritis in the knee joint at a young age.
Physiotherapy can begin after about seven days of rest.
Anterior cruciate ligament tear

Similar to a meniscus tear, an injury to the anterior cruciate ligament is often preceded by a sports accident: the cruciate ligament tears when the lower leg rotates violently with the foot stationary.
Shortly after the accident, those affected feel different degrees of pain in the knee. The ability to move is not immediately impaired, injured football players may under certain circumstances. stay on the field for some time! However, due to the good blood circulation, a considerable swelling quickly develops and the resilience drops considerably.
Sometimes an injury to the anterior cruciate ligament is not immediately recognized and treated. In such cases, instability (frequent twisting) in the knee joint can be clearly observed after a few weeks.
When examining the damaged knee, the doctor will find typical signs of an anterior cruciate ligament tear. These include e.g. the front drawer phenomenon and a positive front laughing man sign. An experienced examiner can identify various cruciate ligament injuries. There is also the option of showing the defect by means of a magnetic resonance scan (MRI) or a knee examination.
In general, the following applies: the higher the instability and the higher the demands on the functionality of the knee, the more likely it is that the anterior cruciate ligament will be restored. In such reconstructions, the destroyed cruciate ligament is replaced by an endogenous tendon using different techniques. As a substitute e.g. the middle third of the patellar tendon, the tendon of the gracilis or semitendinosus muscle.
Read more on this topic at: Anterior cruciate ligament tear
Posterior cruciate ligament injury
The posterior cruciate ligament tears rather seldom and mostly in combination with other structures of the knee joint. Direct force, e.g. in the context of a traffic accident is one of the most common causes.
The symptoms resemble a tear in the anterior cruciate ligament. However, the investigation reveals a back drawer phenomenon and a laughing man's sign.
Posterior cruciate ligament reconstructions are rarely used. Instead, knee stability can be restored through targeted strength training of the thigh muscles (especially M. quadriceps femoris). Surgery should only be considered if the symptoms persist.
Injury to the collateral ligaments
A strain (distortion) of the inner ligament (see also: Inner ligament stretch in the knee) is one of the most common knee injuries and occurs when loads cause the knee joint to bend to the side (valgus trauma).
Typically, knee pain occurs immediately after the accident, while resilience is not restricted. As a rule, a distortion heals without complications. Cold packs and relief of the knee joint support the healing process.
If the inner ligament is completely torn, those affected often describe a sharp-pointed pain. From a therapeutic point of view, immobilization using a splint can be sufficient, in severe cases an operation must be performed.
If there is a varus trauma, i.e. if the knee joint kinks inwards due to excessive force, the outer ligament can tear.
Unhappy triad
Unhappy Triad is a serious injury to the knee joint. The medial meniscus, medial ligament, and anterior cruciate ligament are affected at the same time. Due to the considerable loss of stability, the knee can no longer be loaded. There is a distinct, painful swelling.
Most therapy consists of surgical repair of the knee defects.
Patellar fracture
A patellar fracture is a bony injury to the kneecap. Mostly it arises from direct violence, e.g. in a violent fall on your knees.
It is characterized by severe pain from movement and pressure in the area of the kneecap, as well as swellings and hematomas. Due to the massive pain, many patients can no longer walk independently.
After taking X-rays, the patellar fracture can be divided into different forms (e.g. longitudinal fracture, type A). If the fragments have not shifted (undislocated), a plaster cast is sufficient for 4-6 weeks. On the other hand, more complicated fractures must be operated on and then e.g. be fixed by wire systems.
While jogging
Pain in the knee that does not exist at rest and only when jogging occur, are not uncommon. In medical terminology, this phenomenon is called "Runner’s knee“ (Runner's knees) designated. There can be a multitude of causes for the development of knee pain, which occurs especially when jogging. In most cases, the occurrence of such knee problems can be attributed to one permanent overload the lower parts of the musculoskeletal system. This overload can be caused by a unfavorably changed leg axis (for example in the presence of Bow legs) are favored. In addition, a pronounced weakness in the pelvic stabilizers can increase the risk of developing a runner's knee. In the affected patients the unloaded hip sinks. As a result, there is one excessive tension on the tendon plate of Thigh and knee pain, which is mainly felt when jogging. Furthermore can also Misalignments the normal Foot axis (for example the so-called over-supination), Leg length differences or a shortened one Musculature promote the occurrence of knee pain in the area of the outside of the thigh.
Especially people who just started jogging tend to develop a runner's knee. The reason for this is the fact that these people tend to put excessive strain on their bodies at the beginning. In addition, a wrong running technique and or unsuitable footwear cause knee pain when jogging. Patients who suffer from the so-called runner's knee often feel when jogging sudden shooting pain in the knee. This pain can be so severe that it makes walking impossible. Even normal walking is almost impossible for those affected during a pain attack. The pain experienced in the runner's knee typically projects onto the Knee joint and the Outside of the tibia head.
However, the clinical picture of the runner's knee can be diagnosed relatively easily by a specialist. Already by describing the perceived Symptoms by the affected patient, can help to make an initial suspected diagnosis. In addition, people who suffer from knee pain while jogging have imaging tests such as roentgen or Computed Tomography (CT) for use.
diagnosis
In order to properly assess the cause of the knee pain, the knee must be examined by a doctor. The specialists in this subject are in most cases the Specialists in orthopedics or general medicine.
First, the anamnesis is taken, whereby it is especially important to mention whether a certain movement or an accident preceded the pain. Then follows the physical inspection and the investigation. This is on Swelling, redness, pain, and warming the affected area respected. Certain tests can also be used to examine the restricted mobility, if any. It is important to find out which movements cause knee pain. From this information, the attending physician may be able to determine or make a guess what the reason for the knee pain is. To secure the diagnosis are usually still further investigations arranged. These examinations consist of imaging tests (roentgen, CT, MRI, Sonography), which can provide information about the exact reason and location of the cause of the pain. If all of these tests are unsuccessful, it may be necessary to have a Knee arthroscopy (Knee mirror) must be performed to confirm the diagnosis.
The diagnosis of individual knee pain depends on many factors and can vary widely. Due to the demographic change that comes with a proportionally large elderly population group entered, the symptom is knee pain to one Common disease become. Degenerative diseases play a major role in older patients. This means that because of the stress on the joints, the Wear also increases, and is particularly noticeable in this age group through pain. The consequences are joint diseases such as knee arthrosis. Risk factors are increased age, but also many other things that are associated with increased wear and tear on the joints. These include the presence of legs of different lengths, "X" - or "O" legs and excessive competitive sport. Other diseases too, like rheumatism or Varicose veins, should be considered for knee joint problems in elderly patients.
Diseases that are independent of age are often caused by a injury evoked, or are a Signs of infection. These include, on the one hand, muscle and ligament tears that often happen during sports, as well as Bursitis, which is also noticeable through knee pain.
It happens again and again that there is pain in the knee joint, but no definitive cause can be found. Often the problem here is that although the symptoms occur in the knee, the causes may be found elsewhere. For example, knee pain can occur if a hip joint osteoarthritis, a pseudoradicular pain syndrome (facet syndrome), or simply incorrect footwear is used in sports.
therapy
General pain therapy is usually indicated. Here, depending on the severity of the pain Acetylsalicylic acid, Ibuprofen and Diclofenac resorted to. Some knee joint diseases, and especially injuries, will treated surgically. These include, for example, meniscus and ligament tears, common diagnoses after an injury. The operation is mostly done by means of Arthroscopy (Mirroring, keyhole surgery) performed.
For the treatment of osteoarthritis, which is based on wear and tear of the joints, hyaluronic acid has recently been used as a therapy. Hyaluronic acid is also found naturally in the joint and acts as a lubricant between the joint cartilage. In therapy, it is injected into the joint space by means of syringes, thus providing pain relief. The drug does not regenerate the cartilage tissue, but it does prevent inflammation and make the joint easier to move.
Self therapy
Knee pain that is slow to make itself felt or that occurs after strenuous exercise Usually treated at home at the beginning become. Pain that occurs due to a minor injury should be observed and, under certain circumstances, you can also treat yourself. If you have mild knee pain, there are a few things you can do before calling in a doctor:
- Protection: Avoiding painful and strenuous movements can help the joint to regenerate. Here it is important that the knee not to keep very calm, but to resort to less stressful things that are painless. For example swim instead of to jog, or cycling instead of playing football. If pain persists, a doctor should be consulted and the knee should be spared.
- Cool: The knee every day for 15-20 minutes cooling can reduce the pain and swelling.
- Compression: An elastic bandage around the joint can control the swelling and give the knee the stability it needs.
- Elevate: Bringing the affected leg up helps that Lymph fluid to drain and thus prevents swelling.
- Medication: Over-the-counter drugs like aspirin, and Ibuprofen have anti-inflammatory and analgesic effects and can thus alleviate the symptoms. It can, however Stomach problems arise, which is why long-term self-medication is not recommended.
When to the doctor
A doctor should be seen if the discomfort occurs due to a major accident are or from large swelling, redness, warming around the joint, great pain and fever to be accompanied. The general rule is that if pain persists for a long time or has an influence on everyday movements, in any case Doctor informed should. Immediate medical attention should also be given in the event of very severe pain deformed joint, Immobility of the joint or if the knee accident was accompanied by a loud noise in the joint. If there are concerns as to whether or not a doctor should be consulted, it is generally recommended that a doctor takes care of the complaints and, in the best possible case, creates security not to have to worry. If it is possibly something serious, it is better for every illness to have one initiate early treatmentso that the chances of recovery can be optimized.
Risk factors
In the long run it can be the case for some Diseases of the knee joint, and especially in the case of osteoarthritis, that to reduce individual body weightto avoid the wear and tear of the Joint to prevent. Obesity can increase mechanical stress on the joints, even with normal, everyday things like climbing stairs. This in turn leads to wear and tear on the cartilage in the knee joint and, in the long term, results in osteoarthritis. Congenital problems like X- or If one, or one unequal leg length, can enormously increase the stress on a joint and thus cause wear and tear in the joint over time and cause pain. Different Sports are predestined for an injury to the knee joint. Which includes Skiing, soccer and jogging. A previous knee injury also increases the incidence of re-injury.
forecast
Generally one can say that the more pronounced the complaints are, the more negative the prognosis designed. It is important that if there are significant symptoms, a doctor is consulted and the knee is examined. Most illnesses should medication or surgery treated so that healing occurs. If action was taken in good time, the forecast is usually positive. The Follow-up care of an operated joint should be carried out according to the doctor's instructions, otherwise pain can persist for a long time.
In the following descriptions of diseases we will try to address as many characteristics as possible that make up a certain clinical picture.
Unfortunately there are a lot of deviations from the norm, so the assumed self-diagnosis does not necessarily have to be correct. But we hope through our Self-diagnostic just to be able to help the patient on the internet organ or symptom related look for a disease.
Ultimately, however, only a specialist examination and, if necessary, imaging procedures (X-ray image, MRI etc.) lead to the correct diagnosis.
Please note
In no case does the “self” diagnostic agent replace a visit to your trusted doctor! We also make no claim to the completeness of the differential diagnoses presented (alternative causes). We assume no liability for the correctness of the self-diagnosis you have made! We strictly reject any form of self-therapy without consulting your doctor!

Anatomy of the knee joint
- Thigh bone (femur)
- Medial meniscus
- External meniscus
- Fibula
- Shinbone (tibia)
.
To the diagnostic
Using our “self” diagnostic is easy. Follow the respective link offered, where the location and description of the symptoms best match your symptoms. Pay attention to the point of the knee joint where the pain is greatest.
Where are your complaints?
Medical terms related to the knee joint
For the exact anatomical assignment, we refer to the Anatomy Lexicon our page.
Here are some key terms related to knee pain:
- Head fibulae - fibula head
- dorsal- back
- Fibula - fibula
- Femur - thighs
- Femoral condyle - thigh roll
- Gon - knee, knee joint,
- Hoffa - Fat body of the knee joint
- lateral - outside, on the side
- Medial collateral ligament - inner band
- Ligamentum collaterale laterale - outer band
- Ligamentum cruciatum anterius - anterior cruciate ligament
- Ligamentum cruciatum posterius - posterior cruciate ligament
- medial - Inside
- Medial meniscus - medial meniscus
- Lateral meniscus - External meniscus
- patella - kneecap
- Patellar tendon - kneecap tendon
- popliteal - concerning the hollow of the knee
- Quadriceps tendon - anterior femoral tendon
- Tibia - shin
- Tibial plateau - articular surface of the tibia
- Tibial tuberosity - Elevation of the kneecap tendon attachment to the shin
- ventral - front

Front knee pain
Front knee joint pain primarily relates to the anterior knee joint area. They include pain in the area of the front thigh, the front lower leg, the quadriceps and patellar tendons of the kneecap, and the anterior knee joint space.
In addition to direct anatomical structural damage to the knee joint, problems in other areas remote from the knee joint can also be responsible for pain in the anterior knee joint.

External knee pain
External knee joint pain primarily relates to pain in the area of the outer part of the knee joint and thus includes pain in the area of the outer thigh and lower leg, the outer ligament, the surrounding soft tissues, the outer knee joint space and the head of the fibula.
In addition to direct anatomical structural damage to the knee joint, problems in other areas remote from the knee joint can also be responsible for pain in the outer knee joint.
Knee pain inside

Inner knee joint pain primarily refers to pain in the area of the inner part of the knee.
In addition to pain in the area of the inner thigh and lower leg, this also includes pain in the area of the inner ligament, the surrounding soft tissues and the inner knee joint space.
It cannot be ruled out that problems in other areas remote from the knee can also be responsible for pain in the area of the inner knee joint.

Popliteal pain
Popliteal pain primarily refers to pain in the area of the back of the knee.
In addition to pain in the area of the rear thigh and lower leg, this also includes pain in the area of the joint capsule and the surrounding soft tissues.
In addition to direct anatomical structural damage to the knee joint, problems in other areas remote from the knee joint can also be responsible for pain in the hollow of the knee.
Pain that affects the whole knee
Read more on the subject on the following page: Pain that affects the whole knee