Treatment of pulmonary embolism
Treatment of pulmonary embolism
In case of a acute pulmonary embolism must first clot to be resolved. In order not to aggravate the symptoms, the patient will in a sitting position stored and using a nasogastric tube oxygen provided. In addition, the patients sedated and the pain through Morphine administration treated.

To the Embolus to dissolve, 5,000 to 10,000 units of heparin are administered intravenously. Injections into the muscle must be avoided at all costs. In the event of cardiac arrest due to a grade 4 pulmonary embolism, cardiopulmonary resuscitation with chest compressions and intubation must be initiated immediately. The specific therapy for clot dissolution offers various options.
In stage 1 and 2 of the embolism, the Embolus treated with heparin. Heparin activates the inhibiting factors that inhibit clot formation in the body and potentiates their effects. This means that heparin is primarily the prophylactic agent of choice, provided there are no contraindications.
In addition, the lung even a spontaneous one fibrinolytic Activity, and can thereby dissolve the embolus itself within days to weeks. in the Stage 3 and 4 pulmonary embolism becomes one Fibrinolysis therapy used. This is done using Streptokinase the body's own Plasmin activated. This serves the resolution of clots and can thus both the Embolus, as well as the original thrombusdissolve, for example in the leg veins.
Besides these drug methods of clot dissolution you can also operative or mechanical interventions are used. The main indications for invasive clot dissolution are contraindications for fibrinolysis.
These include especially
- previous major operations in the past 3 weeks,
- a previous stroke of unknown cause,
- known bleeding tendencies and
- Bleeding of the gastrointestinal tract in the past few months.
in the Stage 3 or 4 an embolism, if contraindicated for a Fibrinolysis, the embolus by means of a Catheter about the right heart removed. The pulmonary embolectomy is the last resort to resolve a embolism. Here the patients are sent to a Life-support-machine closed and the affected arteries opened under sight. This is how the embolus can be sucked out of the artery. However, since this procedure is associated with a mortality rate of 25%, this measure is only taken if the other therapy attempts have failed.
Heparin for pulmonary embolism
Heparin is the lead substance of the non-oral anticoagulants, which means that this substance has to be injected for administration.
There are a number of different heparins that differ in their chemical structure and can therefore have different lengths of action, application routes and side effects.
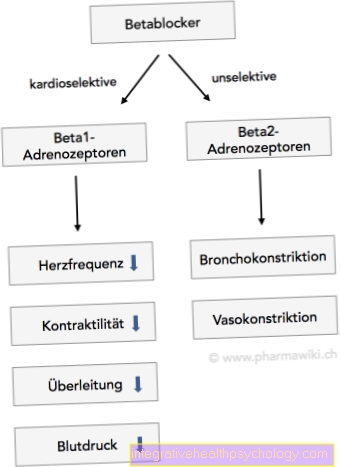
The main mechanism of action is the same for all heparins, namely the inhibition of various levels of the body's own blood clotting.
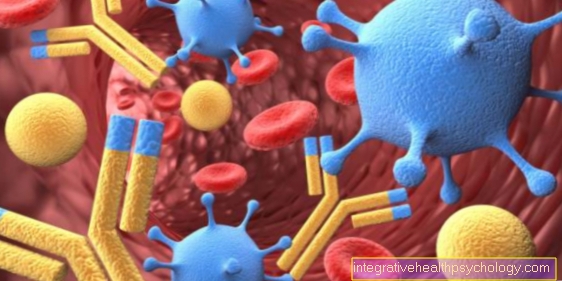
A rare but important side effect, especially of unfractionated heparins, is heparin-induced thrombocytopenia (HIT for short). This can lead to the formation of antibodies, which can result in a massive decrease in blood platelets.
It is therefore important to check the blood values regularly when administering heparins in order to be able to identify and avert further complications at an early stage.
In the context of a pulmonary embolism, mostly unfractionated heparin is initially used in a high dose, which has to be given intravenously via an infusion. Thereafter, the therapy can be switched to low molecular weight heparin. This is injected subcutaneously, i.e. under the skin, and is dosed differently depending on body weight and kidney function.
Lysis in a pulmonary embolism
Depending on the extent to which pulmonary vessels are obstructed by the thrombus in a pulmonary embolism, the clinical picture can vary in severity. If it is a comparatively large thrombus (blood clot), which blocks large parts of the pulmonary circulation, the pulmonary embolism may lead to the need for resuscitation.
In such a case, there is usually an acute stress on the right heart because the blood accumulates in front of the thrombus and the cardiac output can no longer adequately compensate for this. One then speaks of hemodynamic instability, which, in addition to the obligation to resuscitate, is an indication for lysis therapy.
For this a substance is usually called Alteplase used, which acts as a tissue plasminogen activator. The tissue plasminogen is an endogenous molecule that helps to dissolve thrombi again. This process is called fibrinolysis.
As part of a lysis therapy, this is imitated pharmaceutically in order to be able to expose the blocked vessel to the blood flow again as far as possible. At the same time, anticoagulation (inhibition of blood clotting) with heparin should take place in order to prevent the formation of a new thrombus.
Lysis therapy is always associated with an increased risk of bleeding, which is why it should only be carried out under inpatient conditions. There are also a number of contraindications to lysis therapy. As soon as there is an obligation to resuscitate, however, these cease to apply, as the patient's life is in acute danger.
Surgery for a pulmonary embolism
Surgical intervention for pulmonary embolism is rarely carried out and is usually the last treatment option. Only when other therapeutic measures such as lysis, anticoagulation and resuscitation fail can an operation be considered.
This in turn is associated with a high own risk of further complications and usually requires a good previous general condition of the patient. In order to be able to surgically remove the thrombus, the cardiopulmonary circulation must be temporarily removed from the body and taken over by a heart-lung machine. During this time, the surgeon can try to remove the thrombus either mechanically using a catheter or by local lysis.
Guideline
There are several guidelines from different professional associations for the treatment of pulmonary embolism. These are merely a decision-making aid for the treating physicians, without being legally binding.
They summarize the current study situation and incorporate it into the respective therapy scheme. Depending on the clinical picture, they then provide guidelines for the further procedure.
The advantages and disadvantages of various therapy options can also be found in the guidelines in order to take this into account when making an individual decision for the respective case. As a rule, these guidelines are renewed and updated every few years so that the current state of research can be recorded.
For special groups of patients such as older people or pregnant women, the most important instructions for their therapy are recorded in the guidelines, so that nothing is overlooked in "exceptional cases".
The AWMF, the working group of the scientific medical professional societies e.V. is an amalgamation of numerous professional societies in Germany and one of the largest platforms for guidelines. On the subject of “pulmonary embolism”, for example, the current guideline was published in the lead by the German Society for Angiology at the end of 2015 and can be viewed free of charge on the Internet.
Anticoagulant anticoagulants
Anticoagulation is an anticoagulant therapy. After a pulmonary embolism, medication should be used to counteract a new thrombus in order to prevent a pulmonary embolism or to dissolve the existing thrombus.
Anticoagulation is suitable as a therapy option, which can be carried out with the help of various substances. In most cases, anticoagulation for at least three months is necessary after such an event.
The preferred substances are Marcumar®, new oral direct anticoagulants such as Xarelto® or low molecular weight heparins such as Clexane®. They all inhibit the body's own blood coagulation cascade in different ways and can therefore show different interactions and side effects.
You might also be interested in: What are the chances of survival with a pulmonary embolism?
Marcumar®
Marcumar® is the trade name for phenprocoumon, a substance that inhibits the function of vitamin K in the body. Vitamin K is necessary for the production of various components of the coagulation cascade in the liver - if there is no functional vitamin K, the coagulation factors cannot be formed and blood coagulation is disturbed.
Since the production of these coagulation factors usually takes several days, Marcumar® as a drug is generally relatively difficult to control and requires regular monitoring of blood coagulation activity. For this purpose, the INR (International Normalized Ratio) is usually determined, a value that can provide information about the extent of the anticoagulation. After a pulmonary embolism, a value between 2 and 3 is usually sought in the long term.
In the case of long-term use of Marcumar, it should also be noted that there may be interactions between this drug and other drugs and even foods. These can lead to both an increase in the effect with an increased risk of bleeding and a weakened effect with an increased risk of thrombosis. And last but not least, Marcumar® should be switched to heparin in good time before surgical interventions due to its better controllability.
Xarelto®
Xarelto® is the trade name for a substance called rivaroxaban. This belongs to the group of new oral anticoagulants and inhibits the body's own blood clotting. In contrast to the conventional Marcumar®, Xarelto® can be controlled relatively well and does not require an injection, as this drug can be taken in the form of tablets.
Regular control of the individual coagulation parameters is usually not necessary with Xarelto®. However, this substance must not be given during active bleeding or during pregnancy and breastfeeding. Extreme caution is also required in the case of severe renal insufficiency and in combination with other anticoagulant substances, as this can result in an increased risk of bleeding.
After a pulmonary embolism, Xarelto® is usually taken twice a day for the first three weeks after the event, then only once a day until the drug is discontinued.
Also read:
- Xarelto® and alcohol
Clexane®
Clexane® is the trade name for enoxaparin, a low molecular weight heparin.
Like all heparins in this group, Clexane® must also be injected subcutaneously once or twice a day and is usually dosed according to body weight. Particular caution is required in the case of severe renal or hepatic insufficiency, where a dose adjustment is usually necessary.
Otherwise, this substance is usually well tolerated and is also used during pregnancy and breastfeeding.
Duration of therapy
Depending on the extent to which the pulmonary vessels are blocked by the clot, those affected have severe or less severe symptoms. However, pulmonary embolism is usually associated with acute shortness of breath and requires inpatient therapy. In the hospital, depending on various risk factors, anticoagulant therapy is usually initiated, which should usually be continued for three to six months in order to avoid recurrences.
The acute treatment in hospital usually lasts for one to two weeks, provided there are no further complications. An important reason for inpatient treatment is the monitoring of the heart function, which is necessary in most cases, since pulmonary embolism usually places an acute additional strain on the right heart.But imaging procedures and laboratory controls can usually only be carried out in an inpatient setting.
Treatment of pulmonary embolism in pregnancy
Due to numerous hormonal changes in the body of an expectant mother, pregnancy is in principle associated with an increased risk of developing a pulmonary embolism.
Depending on the source, a three to four fold increase in risk is stated. When diagnosing a pulmonary embolism in a pregnant patient, difficulties arise in that the unborn child does not want to be exposed to radiation, but CT is usually the gold standard.
In pregnant women, therefore, an ultrasound image of the deep leg veins is often used, the most common location for thrombi.
Anticoagulation should ensure that it is sustained for the entire duration of the pregnancy and is at least three months long. The agents of choice are low molecular weight heparins such as Clexane®
These can also be administered without any problems during pregnancy. Alternatively, fondaparinux, a synthetic heparin, can also be given. Marcumar® is actually contraindicated and should only be used under strict indications and if other therapy options have failed.
New oral direct anticoagulants such as Xarelto® are absolutely contraindicated during pregnancy. These should not be used on pregnant patients. If possible, lysis therapy should not be used, as this significantly increases the risk of bleeding for the mother and the unborn child and can lead to serious complications. Interventional procedures using catheters to reopen the affected vessel should be preferred in this case.
Read more on the topic:
- Pulmonary Embolism in Pregnancy
- Clexane® in pregnancy











.jpg)