Premature placental detachment
What is premature placental detachment?
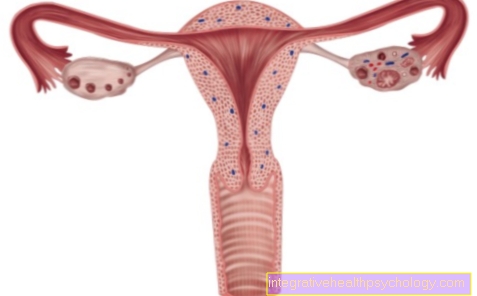
Premature placenta detachment is understood as the total or parts of the placenta loosening of the placenta from the uterus, which takes place while the child is still in the mother's womb. Usually the placenta does not come off until the baby is born. The premature detachment of the placenta can be completely symptom-free and harmless if only slightly dissolved. However, if most or all of the placenta has detached itself from the uterus, this leads to an interruption of the child's blood and oxygen supply, as the placenta is no longer connected to the maternal blood vessels. Furthermore, the maternal vessels separated from the placenta bleed into the uterus and the mother loses blood. Depending on the extent of the detachment, the condition can become life-threatening for both mother and child.

Reasons for premature placental detachment
There can be several causes and contributing factors for premature placental detachment. A trauma to the uterus, such as the force exerted on the abdominal cavity in the event of a fall, fight or accident, can lead to a hematoma of the uterus due to the rupture of the mother's vessels. A bruise causes blood to accumulate between the placenta and the uterus; this is known as a retroplacental hematoma. If the bleeding is heavier and the bruise is getting bigger and bigger, more space is required so that the gap between the placenta and the uterus widens and fills with blood. This congestion of blood can lead to partial or complete detachment of the placenta.
Smoking and increased maternal age and premature placenta detachment in pre-pregnancy are possible risk factors. In the case of a multiple pregnancy, the birth of the first twin can lead to the placenta becoming detached and thus putting the second twin at risk. Premature placenta detachment can also result from medical maneuvers if an attempt is made to adjust the child to a position where the child can be born if the unborn child is in an inappropriate position.
High blood pressure during pregnancy also represents an increased risk of premature placenta detachment and premature birth or miscarriage. High blood pressure during pregnancy can lead to preeclampsia or gestosis, which can have further serious consequences for mother and child .
Read more about this under:
- Pregnancy Hypertension - Is It Dangerous?
- Placental insufficiency
What role does smoking play?
Smoking is one of the risk factors for premature placenta detachment. Nicotine influences the mother's blood flow and thus also the blood supply to the placenta, which is guaranteed by the mother's vessels. The placenta in turn has the task of supplying the unborn child with blood, oxygen and nutrients. Therefore, smoking can affect the child's blood supply. So, consuming nicotine increases the likelihood of early release of the placenta from the uterus. This can put mother and child at risk. In order to reduce the risk of premature placenta detachment, you should therefore refrain from smoking during pregnancy and ideally also during breastfeeding.
Read more about this under: How dangerous is smoking during pregnancy?
Diagnosis of premature placental detachment
A quick diagnosis of premature placenta detachment is vital, especially in severe cases. Therefore, continuous monitoring of the vital parameters and the CTG (cardiotocography) display of the child's heart sounds are necessary. Palpation of the abdomen and uterus is used to assess the height of the uterus and its tone.
The position of the placenta can be checked via the ultrasound and the child's activity can also be displayed via its movements. A possible bruise and the trigger for premature placenta detachment can also be recognized in this way. In addition, a blood sample is taken, in particular to assess the coagulation parameters, which can increase sharply in the event of premature placenta detachment. The hemoglobin level is also determined to estimate the extent of bleeding.
What do you see in the ultrasound?
If premature placenta detachment is suspected, ultrasound is an essential diagnostic procedure. Ultrasound can determine the location and position of the placenta. You can also look for a hematoma, i.e. a bruise, between the placenta and the uterus, as this is one of the possible causes of premature placenta detachment. The activity of the fetus can also be recorded by displaying its movements using ultrasound. In addition to monitoring the child's heart activity using a CTG device, children's activity is an important means of assessing the health of the fetus.
The ultrasound method can also be used to identify diseases of the placenta. Calcification of the placenta is a common disease. Read more on the subject below: Calcified placenta
Read more about this under: Ultrasound in pregnancy
Symptoms of premature placental detachment
Premature placenta detachment is not always associated with symptoms. In 20-30% of cases, the solution of the placenta remains completely symptom-free and can only be detected with the ultrasound device.
The possible accompanying symptoms correlate with the degree of detachment. Grade 1 premature placental detachment is a very minor detachment that in most cases does not cause any symptoms. If one speaks of grade 2, it is a somewhat stronger detachment that can be accompanied by slight vaginal bleeding. The uterus remains soft in its consistency. The condition of the fetus is also mostly normal.
Grade 3 describes a very pronounced detachment of the placenta, which is associated with heavy bleeding and sometimes with intense pain on the mother's side. A state of shock can occur if the mother loses massive blood. This bleeding does not always have to exit vaginally; in some cases the blood seeps behind the placenta and is initially not noticed. The uterus is hard and tense during the examination, labor can also increase massively and a so-called 'labor storm' occurs. The child's heart activity is abnormally changed and it suffers from a lack of oxygen. Intrauterine fetal death, i.e. the death of the fetus in the womb, can occur. Particularly severe cases can lead to coagulation disorders in the mother and disseminated intravascular coagulation (DIC), whereby the consumption of factors important for the coagulation process increases the tendency to bleeding.
Read more about this under: Bleeding during pregnancy
Pain from premature placental detachment
Placental detachment is not always associated with symptoms. Therefore, the absence of complaints is no guarantee that the pregnancy will proceed normally and that the fit and function of the placenta are in order. In many cases, however, premature placenta detachment manifests itself in severe pain and increasing tenderness in the abdomen of the pregnant woman. Often the pain does not build up gradually, but begins very suddenly and with high intensity in the lower abdomen. A quick consultation with a doctor is strongly recommended.
Read more about this under: Abdominal pain during pregnancy
Signs of premature placental detachment
There does not always have to be signs of premature placenta detachment, as around a third of cases remain completely symptom-free. Therefore, the pregnant woman should always attend the recommended medical check-ups during pregnancy, where, among other things, the placental fit and its functionality are assessed. This allows changes to be recorded and acted on if necessary. Sudden vaginal bleeding during pregnancy can have several possible causes, although premature placental detachment must always be considered. Therefore, the pregnant patient should always consult a doctor as soon as possible in the event of bleeding and unexplained pain.
Read more about this under: Signs of miscarriage
Therapy of premature placental detachment
The therapy for premature placenta detachment depends on the degree of solution, the condition of the mother and the condition of the child. If the vaginal bleeding is minor and the condition of the mother and the fetus is normal, bed rest and check-ups will be carried out under inpatient conditions. This is especially the case when the pregnancy is in its early stages. Up to the 34th week of pregnancy, corticosteroids can also be used to induce lung maturity in the fetus. If the bleeding comes to a standstill and the condition of the mother and fetus remains stable, discharge from the hospital can also take place.
In severe cases, the primary goal is to stabilize the mother's circulatory system. Close-knit controls are necessary, with special attention being paid to the patient's coagulation in order to be able to intervene in the patient's coagulation process in the event of abnormalities. If necessary, oxygen and blood are given.
If the condition of the mother and child is at risk, immediate delivery by caesarean section is initiated, regardless of the time of pregnancy and even if the fetus may still not be viable. We also aim to give birth from the 37th week if the pregnancy is advanced. If the condition of the patient and the fetus is stable, a vaginal birth can be attempted, otherwise a caesarean section will also be performed.
Prediction of premature placental detachment
A higher-grade premature placenta detachment poses a threat to the life of mother and child. In severe cases, maternal mortality is around one percent, while infant mortality depends heavily on the week of pregnancy and the birth weight and varies between 10–50%. Depending on how quickly medical intervention is carried out, permanent or temporary damage to health can occur. These include, for example, childhood brain and developmental damage caused by the lack of oxygen.
Experienced premature placenta detachment also increases the risk of recurrence in a subsequent pregnancy.
How common is premature placental detachment?
Fortunately, premature placenta detachment is a very rare complication in pregnancy or childbirth. It occurs in approximately 0.5–1% of pregnancies. The likelihood may increase in certain patients who have multiple risk factors. In general, premature placenta detachment can be identified as the cause of the bleeding in around 30% of vaginal bleeding in the last third of pregnancy.
Can coughing cause premature placenta detachment?
Premature placental detachment due to coughing is extremely unlikely and cannot be found in medical literature. When coughing, the pressure conditions in the abdomen change, but the placenta is usually embedded strong enough to withstand such pressure changes caused by coughing. To trigger a premature detachment of the placenta, much stronger forces are required. This includes falls, accidents or blows to the stomach, although the examples mentioned do not necessarily and do not always have to lead to complications.