What is triple negative breast cancer?
definition
Tumors in the breast can develop certain receptors, i.e. docking points for hormones and growth factors, for example. The tissue of the breast tumors is examined for the formation of three different receptors. If the tumor does not develop any of these three receptors, it is called triple negative, i.e. triple negative.
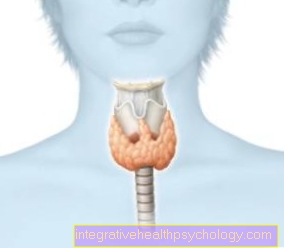
The tumor is considered triple-negative if it does not develop any of the three classic hormone receptors, estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor (HER2), i.e. less than 1% of these receptors are present. 15 to 20% of all breast cancers (Breast cancer) are triple negative.
In the case of breast tumors that have these receptors, antibody or hormone therapy that attacks precisely these receptors and is intended to prevent the tumor from growing can be useful. This therapy option does not apply to triple-negative tumors, i.e. tumors negative with regard to these receptors, since these points of attack are not present in the tumor tissue.

Accompanying symptoms in triple negative breast cancer
Most breast cancer symptoms are confined to the breast.
This can lead to a palpable lump and also to skin changes, such as orange peel. Retraction of the skin and changes in the shape of the breast up to asymmetry are possible. In rare cases, there may be bleeding from the chest. In general, signs of inflammation such as swelling, redness and overheating can also occur if the tumor is of an inflammatory nature.
As the disease progresses, there are enlarged lymph nodes in the armpit and above the collarbone. There is then already a local metastasis (formation of daughter ulcers) in the lymph nodes. The chest wall can rarely be affected.
General symptoms only appear in the late stages of breast cancer, when the tumor has already formed subsidiary ulcers. This can lead to fatigue, exhaustion and listlessness. You can also lose weight, and you may experience a fever and increased night sweats.
Read more on this topic at: How can I recognize breast cancer?
Metastases
Breast cancer can metastasize to many different places, that is, develop malignant daughter ulcers in other parts of the body. The first metastases usually appear in the lymph nodes, especially in the armpit. The metastases can lead to lymphedema (water retention due to disruption of the lymphatic drainage) in the affected arm.
Another place where metastasis can occur is in the bones. Here the patients mostly complain of bone pain.
The tumor can also spread to the lungs, causing those affected to complain of coughing and shortness of breath. Further metastases can occur in the liver, which can lead to yellowing of the skin and eyes and impairment of liver function up to and including liver failure.
Finally, breast cancer can also metastasize to the brain. Depending on the location of the tumor, neurological deficits can occur here.
Read more on this topic at: Metastasis in breast cancer
diagnosis
Most tumors are palpated by the patients themselves. Since the tumor can grow very quickly, normal breast cancer screening usually fails to detect it if it develops in the intervening time.
Since mainly younger patients are also affected, mammography (X-ray image of the breast) is usually not very suitable, as the glandular tissue of the breast is still very dense in these patients. In the Sonography (Ultrasound) the tumor usually does not look like a classic malignant tumor, but rather like a benign change, which is why it can be misjudged.
Magnetic resonance tomography is the most sensitive method (up to 100%) for the detection of a triple-negative tumor in the breast, but here too the tumors can look like benign lesions, for example Cysts, represent.
However, the diagnosis is primarily made using mammography and ultrasound; if the findings are unclear, an MRI of the breast is connected. A breast biopsy (tissue sampling) must then always be performed to confirm the diagnosis by a pathologist.
Tissue sample
The tissue sample is necessary to differentiate between the various types of breast cancer, which is also crucial for therapy. In triple-negative breast cancer, immunohistochemistry (this is a special procedure for staining certain structures and proteins under the microscope) does not reveal any relevant expression of the hormone receptors (Progesterone receptor and estrogen receptor) and the receptor for human epidermal growth factor.
However, the growth patterns can vary greatly within the tumor form, which is also relevant for the prognosis. Therefore, an examination by the pathologist is crucial for the further course of action.
Read more on this topic at: Importance of the biopsy for breast cancer diagnosis
Therapy for triple negative breast cancer
Therapy for triple negative breast cancer consists of several parts.
Usually a biopsy is done first (Tissue sample) taken from the so-called sentinel lymph node to determine whether the lymph nodes are already affected. The breast cancer is then provided with clips so that you can still know where the tumor was. This is used because the tumor mass can be reduced significantly after system therapy with chemotherapeutic agents.
Chemotherapy is recommended here because it makes the tumor easier to operate afterwards and chemotherapy can even lead to a pathological complete remission. This means that the tumor can then no longer be detected by the pathologist. If this happens, the patients have a very good prognosis after the subsequent operation.
The operation can be performed in two different ways. On the one hand, you can completely remove both breasts and then reconstruct them cosmetically. The results of the reconstruction are usually better here, since a symmetrical reconstruction occurs. This operation is mostly recommended for patients with hereditary breast cancer.
However, breast-conserving surgery can also be performed as an alternative. Here, however, the breast must also be irradiated and, if more than two lymph nodes are affected, the lymph node region must also be irradiated.
Radiation therapy reduces the risk of one Local recurrence (Recurrence of a tumor in the same place) by 50% and so many patients can be permanently cured.
In addition, removal of the ovaries is indicated in patients with the BRCA mutation (see: breast cancer gene), as this reduces mortality from breast cancer by 62% and from triple-negative breast cancer by 93% and of course also reduces the risk of ovarian cancer.
chemotherapy
The neoadjuvant chemotherapy (Chemotherapy before an operation to reduce the number of tumors) is strongly recommended for triple-negative breast cancer, as it is very aggressive and rapidly growing and therefore usually responds very well to chemotherapy.
The standard chemotherapy composition consists of anthracyclines and taxanes, either in combination or sequentially. This combination ensures a pathological complete remission in some of the patients (tumor can no longer be detected by the pathologist), which has an excellent prognosis.
The part of the patient who does not have a pathological complete remission has a worse prognosis. Therefore, new combinations of chemotherapeutic agents are currently being investigated for these patients. Above all, the additional administration of capecitabine or carboplatin has shown good results (improvement in remission from 30% to 50%).
However, more chemotherapy drugs also have more side effects and therefore the higher amount must always be weighed carefully.
In general, there are indications that in the future more patients will be able to achieve a good prognosis through extended chemotherapy.
Read more on this topic at: Breast cancer therapy
Immunotherapy and Antibody Therapy
There is currently no targeted therapy (antibodies or immunotherapy) for the triple-negative breast tumor. However, there are substances that are currently being investigated in clinical studies.
The first substance is the PARP inhibitor olaparib. PARP inhibitors inhibit the enzyme poly-ADP-ribose polymerase and are intended to prevent the tumor from repairing DNA damage that has occurred as a result of chemotherapy. It is intended to be used in patients with BRCA mutation and triple negative breast cancer after surgery.
Another substance is the antiandrogen enzalutamide. It should be used in triple-negative breast cancer with expression of androgen receptors (50%). Both are showing promising results in clinical trials and may become available in the near future as targeted therapies for triple negative breast cancer.
Chances of recovery in triple negative breast cancer
Triple-negative breast cancer is a disease that has a high risk due to its very rapid growth. If a pathological complete remission is achieved through chemotherapy, the chances of recovery are very good. If this does not happen, the prognosis is significantly worse, but it can be improved as much as possible by completely removing both breasts and then radiotherapy.
Read more on the subject at: Chances of recovery from triple negative breast cancer
Life expectancy
The 5-year survival rate for triple negative breast cancer is just under 80%. Of course, it depends heavily on the stage at which the disease is discovered. The less advanced the tumor, the better the chances of mastering it and healing the patient.
Read more on this topic at: Life expectancy in breast cancer
How high is the relapse rate?
The risk of relapse in triple negative breast cancer is highest in the first two to three years. Later recurrences very rarely occur.
Read more on this topic at: Follow-up care after breast cancer
Causes of Triple Negative Breast Cancer
A mutation in the BRCA1 gene is present in 50% of cases of triple negative tumors in young women. This is a germline mutation that occurs in all cells, including healthy cells, and is therefore inherited. This means that these tumors are inherited forms. The BRCA1 mutation is less common in older patients.
Read more on this topic at: The breast cancer gene
Other mutations are also common, such as the TP53 mutation. This is a gene that is responsible for the normal cell cycle. If this gene mutates, this leads to an increased rate of cell division. This mutation can also be inherited (Li Fraumeni Syndrome) or arise spontaneously through chemical substances such as cigarette smoke. In general, the disease often affects young women.