Tiptoe in the child
introduction
Tip-toe walking is observed in about 5% of preschool children.
Strictly speaking, the term tiptoe is not quite correct, as the children walk on the forefoot, with the toes lying flat on the floor and the rolling process largely absent. The term toe gait would be more appropriate.
Children with such a gait pattern are presented to the orthopedic surgeon more often. If a toe gait has been present for more than three months, it is referred to as "persistent" (persistent).

causes
Idiopathic toe walking
In many children, intensive diagnostics and questioning do not reveal any cause of tiptoe walking.
So there is no underlying physical or mental illness, the tiptoe occurs for unknown reasons. One speaks here of idiopathic (unknown cause) or habitual (habitual) toe-walking. The habitual tiptoe can be divided into 3 forms.
Type I.
Type I accounts for about 1/3 of the cases, the gait anomaly being caused by a shortened muscle. The children can therefore usually not stand on the entire foot surface and their balance is impaired.
Type II
In type II, tiptoeing occurs more often in the family, so it is based on a genetic component. This type 2 occurs in slightly more than half of all idiopathic tip-toe walkers. The children can then stand on the entire surface of their feet and, if requested, walk in the normal heel gait, although the hips must be rotated outward to do this.
Type III
Type III is called “situational tiptoe walking”. The children can walk with the heel without problems, only when they are under strain (in certain situations) do they involuntarily return to tiptoe. Type III patients also have difficulty concentrating and unusual behavior.
During childhood, many of these children develop perfectly normal gait without medical attention. Especially in children who are about to learn to walk, tip-toe gait often occurs, which usually turns into a normal gait pattern after 3 to 6 months. It is important that idiopathic tiptoe is always a diagnosis of exclusion, which means that other diseases must first be excluded in order to be able to make this diagnosis.
Shortened Achilles tendon
In idiopathic or habitual toe walking, the Achilles tendon shortened. In addition, the Calf muscles contracted (tense). There is disagreement among medical professionals as to whether these two symptoms are the result or the cause of walking toe.
Neuromuscular causes
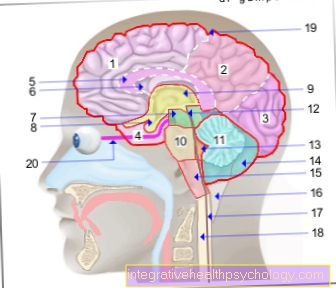
There are numerous neuromuscular disorders in which tiptoeing can appear as a symptom. The causal disorder can be found on all levels from the brain to the executing muscle.
Above all, the cerebrum, which gives the command for the muscle contraction, or the spinal cord, which forwards the commands, should be mentioned. The associated clinical pictures are e.g. spastic cerebral palsy or delayed maturation of the corticospinal tract (a strand of the spinal cord). Differentiation from idiopathic toe walking is often difficult.
In idiopathic toe walking, even with the knee bent, the foot is so bent as if the child were standing on toes. In spastic cerebral palsy, on the other hand, when the knee is bent, the foot often goes back into an extension position (toe tips point towards the nose).
The delayed maturation of the corticospinal tract occurs more frequently in some families, here the tiptoe gait usually changes into a completely normal gait pattern at an age of 6 to 8 years.
Even with progressive muscular dystrophy, a hereditary muscle disease, the increasing susceptibility of the muscle fibers can lead to tiptoe walking. It is typical here that the children initially develop a normal gait pattern and only then transition into tiptoeing.
Furthermore, various nerve diseases can lead to tip-toe walking.
Clubfoot
The clubfoot is one congenital deformity of the foot, which often occurs on both sides. Because of this misalignment, Tiptoe come. The affected children often learn to walk late and are noticeable because they are unsafe to walk.
Mental disability
Studies have shown that a Tiptoe occurs far more frequently in mentally retarded children than in other children.
One suspicion is that these children have a disturbed sense of balance and walking on their toes helps them to get more accurate information about the balance from the ankle.
Another theory is that children are in their Development lagged are and so initially at a stand of Learning to walk stopped where the Heel gait is not yet mastered.
autism
Autism is a congenital, serious developmental disorder that affects information transmission and processing.
Even in early childhood, those affected are noticeable due to a lack of communication and social interaction skills. In addition to stereotypical behavioral patterns and strikingly good skills in attention, intelligence and memory, difficulties in coordination are characteristic. Toe-toe is observed in up to half of autistic children, whereas adults with autism usually no longer walk toe.
The children affected also move around in a hopping, whirling or stilting gait. Researchers suspect that the children compensate for such a vestibular (the sense of balance) disorder.
Conversely, the increased occurrence of tiptoe walking in autistic children does not mean that the majority of children who occasionally walk on tiptoe are autistic. The habitual form of tiptoeing is much more common, and if the child is not observed to have behavioral problems, there is no reason to suspect that the child may be autistic.
There is one form of autism - Asperger's Syndrome. Asperger's syndrome is characterized by difficult social interaction, such as a lack of or reduced empathy and a lack of understanding of emotional messages such as friends, sadness, anger or anger.
Read more on the topic: Asperger syndrome
Diagnosis

Often times, tiptoe is harmless and only occurs temporarily.
In order to rule out more serious neurological or mental causes, the doctor decides on a more or less complex diagnosis on a case-by-case basis. This depends on the age at which the toe walking occurs, how long it has lasted or what other symptoms have been noticed.
In any case, the doctor takes a close look at the child's gait. He examines the anatomy of the foot, the ankle and the calf. The mobility of the hips and knees should also be tested. It is also important to check the child's sense of balance.
The gait analysis can also be done electronically by capturing reflectors on the skin with many small cameras. An EMG (electromyogram) also measures muscle activity in order to rule out diseases of the nerves or muscles. Here, the foot lifter muscle (Tibialis anterior muscle) checked for its function.
If cerebral palsy, intellectual disability or autism are suspected, appropriate neurological function tests are carried out and mental development is checked.
treatment

Treatment also depends on the cause of the toe walking.
Is the toe walking due to another condition such as a neuromuscular disorder, a clubfoot or in the context of autism, this underlying cause should be treated as best as possible.
If a causal therapy is possible, walking on tiptoe will also work normal gait pattern transform. The forms of therapy mentioned here mainly relate to the idiopathic Toe walking and forms in which the underlying disease cannot be treated as the cause.
physical therapy
Toe-walking almost exclusively affects preschool children. In about 50% of the cases, the problem of walking on your toes resolves itself by the time you start school. The first part of the physiotherapeutic approach is assessing the severity. For this purpose, the feet and legs are examined. Particular attention is paid to the mobility of the upper and lower ankle joints, as well as the other large joints of the lower extremities such as the knees and hips. It is also important to observe the gait pattern closely and evaluate it accordingly. In about a third of those affected, the calf muscles or the Achilles tendon shorten. This can be eliminated through appropriate physiotherapeutic stretching exercises. In addition, the physiological arch of the foot often flattens out and can be rebuilt through physiotherapy.
Children also tend to have a hollow back (Lumbar spine lordosis) fall. The physiotherapeutic measures then serve in the sense of a posture school to build up strength, e.g. the back muscles and to promote mobility. Balance and coordination exercises are also helpful. Regular physiotherapy shows considerable success after just 6 months and can be completed after one to two years.
If, despite conservative measures such as physiotherapy, there has been no success, orthoses, plaster casts or splints are available as an alternative to correcting the foot deformity. If the tiptoe did not grow together in childhood and continues into adulthood, problems with the back, hips and knees usually arise due to the incorrect loading. This in turn results in various starting points for physiotherapy. Above all, strengthening the right muscles to compensate for poor posture is relevant here. In physiotherapy, attention is also paid to getting rid of the learned bad posture and relearning the physiological gait. This process can be very tedious, but in the long term it is the only chance of freedom from symptoms.
Osteopathy
In addition to physiotherapy, osteopathic strategies can also be helpful. Toe walking is often associated with limited mobility in other joints, especially the upper ankle. At best, the osteopath senses this and counteracts it accordingly. Bad posture, e.g. of the back can be treated with the help of osteopathy.
Cognitive disorder
Children who prefer tiptoe often have difficulty finding their balance in normal stance. In this regard, there is a disturbance in the perception of balance. However, this can be trained and optimized with various exercises. Some children tiptoe in situations where they are under high stress, excitement, or fatigue. The toe walk is situational with these children. An attempt can be made here to change the perception of such triggering situations and to find appropriate strategies, e.g. to develop against stress. In some tiptoe-walking children, there is a correlation with other disorders. In some cases the children show weaknesses in concentration or other abnormalities in behavior.
insoles
For tiptoe therapy, there are specially developed insoles, the pyramid insoles Pomarino®. The insoles are individually adapted for each child. The foot is particularly supported by this insert and gets new hold.Overall, the material is very resilient, which is especially important for the heavy load on the forefoot when walking toe. The insoles not only have a direct positive effect on the foot, but also have an indirect effect on the tendons and muscles.
Summary
The idiopathic clubfoot "grows together" in many cases even in childhood without medical intervention. When therapy is necessary and when regular checkups are sufficient, the specialist doctor (usually an orthopedic surgeon) will decide in each case.
Special pyramid inlays are often used in early therapy. These are individually adapted to the foot and are intended to force it into a normal position. A shortened Achilles tendon can also be treated through physiotherapy and certain stretching exercises. This treatment of idiopathic tip-toe gait is completed after approx. 6 to 24 months and has a very good prognosis.
If this does not result in sufficient improvement, an attempt is made to achieve a normal position with the help of orthotics, plasters or splints. The frequently contracted calf muscle can be relaxed by injecting botulinum toxin (Botox). Surgical lengthening of the shortened Achilles tendon, however, is rather rare.
course
The course depends on the underlying disease and its Therapy options from.
With idiopathic Tiptoe In half of all cases, the Gait pattern without treatment.
Remains that Tiptoe Preserved into adulthood, widened forefeet and hollow feet are common.
The consequence of abnormal stress on certain muscle groups and the skeleton can lead to premature wear and tear Misalignment of the hip, knee or ankle. Type III in particular has a high spontaneous healing rate, while types I and II treated in good time also have an excellent prognosis. This is best when treating before the age of 5 occurs, long-term consequences are then not to be expected. Treatment is also very effective beyond that, but it can be more lengthy and complex.







-buschmcke.jpg)