Herniated disc of the lumbar spine
introduction
The spine consists of:
- Cervical spine
- Thoracic spine
and - Lumbar spine.
The lumbar spine (short: Lumbar spine) consists of five vertebrae on top of each other, which consist of bones and form a horizontal underside.
The intervertebral disc rests on this, which on the one hand makes the movements that the spine has to carry out with less friction and on the other hand cushions forces that load on the spine (Body shock absorbers).

The intervertebral discs are partially elastic and consist of two parts, the Fiber ring (Annulus fibrosus) and one Gelatinous core (Nucleus pulposus).
The intervertebral disc is delimited exactly between two vertebral bodies and is well secured.
If there is chronic, non-physiological stress on the spine, the pressure on the intervertebral disc can become so great that the ring tears and the liquid core emerges.
In this case, the intervertebral disc tissue (Incident, also called prolapse, med) either backwards (dorsal) or forward (ventral) exit.
As a result, the intervertebral disc has lost its swelling pressure and the shock-absorbing properties let go.
The pushing out of the intervertebral disc between the two vertebral bodies or the nucleus pulposus from the annulus fibrosus is called disc prolapse. As a result, the vertebral bodies are no longer at a safe distance from each other and are approaching each other.
You can also find a lot of general information on our main page: disc prolapse
Is the herniated disc very old or very pronounced (so-called Mass incident) it can be that the vertebral bodies between the intervertebral discs come so close together that the bone ends come into contact and rub against each other when the load is particularly high. Most of the time, it's the trailing edges or the leading edges that meet. As a result arise chronic back pain.
The central part of the vertebral body rarely comes into contact with its adjacent vertebral body. Basically, this only happens when the intervertebral disc has pushed itself completely out of the tightness between the vertebral bodies and the entire vertebral body lies on the lower vertebral body.
The bone contact between the individual vertebral bodies and the friction ultimately causes pain. Mostly with movements of the spine (e.g. during To run, Stooping or Sit), but in extreme cases also at rest.
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
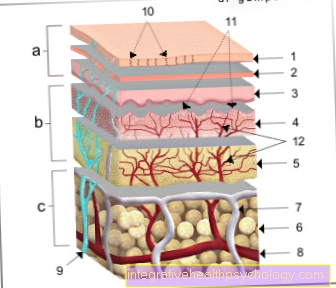
Illustration of a herniated disc

Disc prolapse -
Nucleus pulposus prolapse
A - herniated disc from the left
B - herniated disc from above
C - Healthy disc
a - neck and chest area
b - lumbar region
- Fiber ring -
Annulus fibrosus - Gelatinous core -
Nucleus pulposus
1st + 2nd intervertebral disc
(Intervertebral disc) -
Discus inter vertebralis - Spinal nerve -
Spinal nerve - Spinal cord -
Medula spinalis - Vertebral bodies -
Corpus vertebrae - Spinous process -
Spinous process
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms of a herniated disc of the lumbar spine
The symptoms of a herniated disc of the lumbar spine can vary greatly depending on where the herniated disc is located and whether nerves are pinched by the incident (see also: Herniated disc with nerve damage). If the herniated disc is located in a place where there is no nerve root irritation, the disease can proceed without pain and without neurological deficits (e.g. feelings of numbness). In this case, the herniated disc does not need to be treated.
You can read more detailed information on this here: Back pain or is there a herniated disc without pain?
In many cases, a herniated disc compresses the nerve roots that leave the spinal cord in the lumbar region. This causes severe back pain that occurs very suddenly and "shoots into the back", so to speak. Such a pain attack is triggered, for example, by activities in which you lift something up or bend over. The person concerned immediately takes a relieving posture, as every further movement worsens the pain. Even a sneeze or cough is enough to aggravate the severe back pain. In order to protect the spine, the muscles in the back and particularly in the lumbar vertebrae harden as a reflex. It feels stiff, which is also known as muscle tension or muscle blockage.
A herniated disc in the lumbar spine is heralded in some cases (often with initially milder symptoms). Severe pain in the lower back that lasts longer than a week and may even radiate into the legs can be warning symptoms of an impending herniated disc and should definitely be examined by a doctor (herniated disc symptoms in the leg). The so-called sciatic nerve runs in the area of the lumbar spine. If this important nerve is constricted by the herniated disc, back pain often occurs, which radiates into the buttocks or legs, which is generally also referred to as "lumbago".
Neurological failure symptoms can also occur.
This includes, for example, a tingling sensation in the leg ("pins and needles"), a furry feeling or a feeling of numbness from the herniated disc in the area from hip to foot. While a tingling sensation can indicate minor damage to the nerve, numbness is a sign of a complete failure of the sensory part of the affected nerve.
Please also read: Tingling after a herniated disc
These symptoms must be taken seriously, as it can even lead to paralysis in the leg muscles.
Another symptom of a herniated disc in the lumbar spine can be an altered gait pattern. Depending on whether the incident is between the fourth and fifth lumbar vertebrae or the fifth lumbar vertebrae and the tailbone, the person concerned can no longer stand on the tip of the foot or on the heel.
In the worst and very rare cases, a herniated disc can constrict nerves in such a way that a paraplegic syndrome occurs, in which, for example, neither pain nor touch are felt and the legs become paralyzed. This condition is an acute emergency and must be treated surgically immediately.
The herniated disc in the lumbar spine can also trigger a so-called cauda equina syndrome, which should be recognized urgently and, if left untreated, can lead to permanent paraplegia. We therefore recommend our website for further information: Cauda equina syndrome - do I have paraplegia?
Read more on the topic: Symptoms of a herniated disc in the lumbar spine

You can see the schematic image of an MRI of the lumbar spine.
- Blue: intervertebral disc
- Red: herniated disc (mass prolapse L4 / 5)
- Green: spinal cord
- Yellow: vertebral body with spinous process
Pain in a herniated disc of the lumbar spine
A characteristic symptom of a Herniated disc of the lumbar spine (lumbar spine) are pain.
However, depending on the exact location of the incident, the pain can vary in severity and be pronounced in different places. Typical is a sudden onset, very strong and "shooting" pain in the lower back. If there is a herniated disc of the lumbar spine, pain also often occurs, which radiates into the leg and foot. A herniated disc is a likely cause, especially if the pain radiates to one or both legs.
Pain in a herniated disc of the lumbar spine is caused by compression of the nerve cord that runs in the spine. Often times, due to the compression of the nerves on the lower back, the pain is felt in the legs or feet. The pain can be treated conservatively through exercises and the Taking pain reliever medication.
Through the Operation of a herniated disc in the lumbar spine the nerves are also relieved and freedom from pain can be achieved. Which therapy makes sense in individual cases should be discussed with the attending physician after a detailed diagnosis.
Special features of the lumbar spine
The Lumbar spine (Lumbar spine) has one in contrast to the thoracic spine and the cervical spine Specialty.
The vertebrae are placed particularly steeply to one another. In the normal case, they can counteract forces that are directed forwards or backwards. Such forces are most likely to occur when bending over and tilting the upper body back and forth. Instabilities can arise, especially with movements that are performed very frequently and in a non-physiological manner.
From Herniated discs are most likely the vertebrae LWK (lumbar vertebrae) 4 and 5 (herniated disc L4 / 5) as well as LWK 5 and SWK (sacral vertebrae) 1 (Herniated disc L5 / S1) affected.
In addition to the chronic stress that is too Herniated discs of the lumbar spine congenital deformities of the vertebral bodies can also occur in some rare cases. These misalignments particularly often affect the vertebral arches of the vertebral bodies and encourage the occurrence of one Vortex sliding and Disc deterioration.
In addition to the pain that can occur when opposing vertebral bodies rub against each other, neurological symptoms represent a further risk. The spine not only serves the stability of the body but also forms a kind of tunnel system for it Spinal cord which leads from the head to the lumbar spine through holes (foramina) lying one above the other through the vertebral bodies. If there is a herniated disc, there is therefore the risk that the intervertebral disc that is pushing out will press against the spinal cord, leading to sometimes massive neurological restrictions.
In some, slight courses, the patient usually only feels one tingle in left or right leg. In severe cases, the spinal cord can become so compressed that it causes symptoms Paraplegia comes.
Also Symptoms one Incontinence can Signs of a severe herniated disc be. In many places where the intervertebral disc has pushed out and where adjacent vertebral bodies are often tilted on top of each other, a herniated disc also has the consequences an instability.
For the patient, this has the consequence that he can no longer carry out movements so easily and that forces that are to be diverted via the spine load undamped on the entire spine. This in turn results in increased stress and damage to the other vertebral bodies. In many cases, for this reason, when a herniated disc occurs in an adjacent area, another occurs.
To one Herniated disc of the lumbar spine to prevent, should first be any existing Obesity be dismantled.
Furthermore, movement sequences should be optimized under physiotherapeutic supervision. Long periods of sitting or standing should be avoided.
When choosing shoes, you should ensure that you have comfortable but stable shoes. People in sedentary professions should leave the workplace at regular intervals and do movement exercises. These include stretching exercises and stretchingthat should be done at regular intervals. Relaxation exercises the Musculature In the form of massages can help to soften the muscles strained by the deformity.
Diagnosis of a herniated disc of the lumbar spine
The complaints that neurological examinations and ultimately the imaging procedures can help diagnose a herniated disc.
Typical symptoms of a herniated disc of the lumbar spine are severe back pain when exercising (while standing, bending over, sitting).
Kick in severe forms even at rest severe pain. In addition, the specialist asks Numbness or tingling sensations due to the herniated disc in the legs to. If you have a new incontinence you must tell the doctor in charge of this, as this is a severe form of herniated disc of the Lumbar spine can act. In addition, the specialist carries out a neurological examination, with him simple physical exams can find out whether it is a herniated disc or not.
In order to secure the suspicion of "herniated disc lumbar spine" radiological imaging carried out. A X-ray image can indicate an incident due to a decrease in height of the intervertebral disc. For the exact diagnosis are available Computed Tomography (CT) or the MRI examination of the lumbar spine to disposal. They produce sectional images of the Spine on what you can see at what level the herniated disc of the lumbar spine is and in which direction the Intervertebral disc has moved. To the Nerve root In rare cases, being able to make a most accurate assessment becomes a so-called Myelography carried out. Here is a Contrast agent injected into the spinal canal and then an X-ray or CT scan is performed.
This has proven to be the most valuable of all imaging diagnoses MRI of the lumbar spine established. The MRI of the lumbar spine can best represent the extent and potential dangers of a herniated disc of the lumbar spine.
MRI of the lumbar spine for a herniated disc
To one Herniated disc of the lumbar spine In order to be able to diagnose with certainty, diagnostic imaging devices are often used.
A frequently used method for diagnosing a herniated disc is thus Magnetic resonance imaging (MRI of the lumbar spine). The MRI creates images of the entire spine without the use of harmful radiation.
The examination is usually carried out by radiologists and can be carried out in a clinic or a private practice. The creation of the pictures takes about half an hour, depending on the device. In order to check the spine for a herniated disc, the images are usually examined and interpreted from the side.
If there is a herniated disc, typical changes are visible on the MRI. If the rupture of the fibrous cartilage ring of the intervertebral disc can be seen in the images taken during the MRI, the diagnosis of a herniated disc can be made.
It should be noted that an MRI examination cannot take place if there are non-removable metallic objects in the body. Whether an MRI examination is possible in an individual case is usually discussed in advance by the attending physician.
- MRI of the lumbar spine
and - MRI for a herniated disc
Localization of the most common herniated discs in the lumbar spine
Herniated disc L3 / L4
L3 and L4 describe the height of the herniation and is a very common location for a herniated disc. The herniated disc is at the level of the lumbar spine, precisely at the same level as the topmost point of the iliac crest.
Are you interested in this topic? Read more about this under: Disc herniation of L3 / L4
Herniated disc L4 / L5
Due to natural signs of wear and tear, the area between the fourth and fifth lumbar vertebrae ("L4 and L5") most often leads to a herniated disc. The reason for this is that this area of the lumbar spine is most stressed during physical exertion or during sport. The herniated disc L4 / 5 presses on the nerve that leaves the spinal cord in this area. This leads to severe pain in the outer front thigh and the inner front of the lower leg.
The pain is often triggered by unusual movements or when lifting heavy loads and can be exacerbated by sneezing or coughing. In addition, there may be sensory disturbances in the areas described on the leg, for example it may tingle, feel numb or furry, similar to a leg that has fallen asleep. The so-called identification muscle for a herniated disc L4 / L5 is the quadriceps femoris muscle, the four-headed thigh extensor on the front of the thigh. If the herniated disc presses on the motor nerve fibers to this muscle, the knee joint can no longer be stretched. On the basis of the identification muscle, the justified suspicion for the diagnosis of a herniated disc in the L4 / 5 area can often only be expressed by examining the extension of the knee. Toe lifting is also only possible to a limited extent, which is why it is difficult or impossible for the person affected to walk on the heel while the toes are stretched in the air (heel gait).
Read more on the topic:
- Herniated disc L4 / L5
- L5 syndrome

Disc prolapse -
Nucleus pulposus prolapse
A - herniated disc from the left
B - herniated disc from above
C - Healthy disc
a - neck and chest area
b - lumbar region
- Fiber ring -
Annulus fibrosus - Gelatinous core -
Nucleus pulposus
1st + 2nd intervertebral disc
(Intervertebral disc) -
Discus inter vertebralis - Spinal nerve -
Spinal nerve - Spinal cord -
Medula spinalis - Vertebral bodies -
Corpus vertebrae - Spinous process -
Spinous process
You can find an overview of all Dr-Gumpert images at: medical illustrations
Herniated disc L5 / S1
A Herniated disc L5 / S1 lies between the fifth lumbar vertebra and the first coccyx vertebra. Often an incident in this area is referred to as "sciatica" because of the Sciatic nerve causes severe pain when contracted by the herniated disc. Checking the so-called Lasègue sign is a simple method to be able to make the suspected diagnosis of a narrowing of the sciatic nerve. The person concerned lies on their back and the painful leg is lifted while it is extended in the knee joint. This will the nerve stretched and in the event of a constriction, pain is triggered. The pain of a herniated disc in the range of L5 / S1 can be up to Heel and little toe radiate.
In these areas it can too Sensory disturbances come on the leg, for example, it may tingle, feel numb, or feel furry. The so-called identification muscle for a herniated disc is L5 / S1 Triceps surae muscle, the three-headed calf muscle on the back of the lower leg. If the herniated disc is due to the motor nerve fibers presses on this muscle, the foot can no longer be bent (bent downwards). On the basis of the identification muscle, the well-founded suspicion of a herniated disc in the L5 / S1 area can often only be diagnosed by examining the active and powerful flexion of the foot, since the affected person is no longer or only more difficult walk on your toes can.
therapy
Two types of treatment are possible: the conservative and the surgical treatment method.
In most cases, a conservative method is sufficient to treat the herniated disc of the lumbar spine. Conservative treatments include pain management and training the back muscles.
- Appropriate pain therapy through medication is the most important pillar of treatment for a herniated disc. The doctor prescribes pain relievers, which also have anti-inflammatory effects, since an incident is often associated with a local inflammatory reaction. If oral tablets are not enough, a local injection, i.e. injections into the region of the herniated disc, can relieve the pain with medication for a while. Cortisone can also be mixed into the local syringe to inhibit the inflammatory process.
Read more about this under our topic: Medication for a slipped disc - Warmth stimulates the blood circulation in the skin and loosens the stiff back muscles a little, so that fango or mud packs, red light or warm clothing also help to alleviate the pain.
- Another important pillar of conservative treatment is strengthening the back muscles. Physiotherapy exercises relieve the spine. This should start as soon as possible. Massages or special relaxation exercises can also help relax the cramped back muscles.
Read more on the topic: Physiotherapy for a herniated disc - Heavy physical exertion that puts increased stress on the back should not be performed. Carrying heavy loads and working in a stooped position are prohibited.
Read more on the topic: Therapy of a herniated disc of the lumbar spine
After six to eight weeks, the symptoms should have improved. If there is no improvement, the success rate for conservative therapy decreases.
Exercises for a herniated disc of the lumbar spine
If a herniated disc has occurred, exercises can help relieve symptoms and treat the herniated disc.
Exercises that build muscle and thus stabilize the back are particularly important in the case of a herniated disc, as the injury leads to instability of the lumbar spine and a weak back has often promoted the development of the herniated disc.
Next to the Training the back muscles is especially useful in the initial stages of treatment Training the abdominal muscles essential.
The attending physician and physiotherapist can best assess which exercises make sense in an individual case. Since the correct execution of the exercises is relevant for the success of the treatment, it is advisable to carry out the exercise at the beginning with the presence of the therapist.
In addition to exercises that serve to build muscle are also frequent Stretch- and Mobilization exercises integrated into the program and can help restore the function of the spine and the nerves that run through it.
Please also read our extensive topic from the field of physiotherapy: Exercises for a herniated disc and Exercises after a herniated disc of the lumbar spine
Last resort: surgery

If any of the following occurs, the affected person should undergo surgery to herniate the lumbar spine:
- Signs of paralysis
- no response to pain medication
- Rapidly worsening symptoms of the lumbar disc herniation
- Cauda equina syndrome.
Cauda equina syndrome is a real emergency in orthopedics. Here the herniated intervertebral disc clamps off the nerve roots and the spinal cord, causing the following symptoms:
- Bladder incontinence after a herniated disc of the lumbar spine
- Fecal incontinence,
- Numbness in the genitals
and - Anal area (also called breeches anesthesia)
During the operation, the surgeon uses a microscope to remove the parts of the herniated disc and relieve the nerve root. After the operation, the patient remains in the hospital for three to five days. From there it often goes straight to rehab. Back-friendly behavior, stabilizing the back muscles with the help of physiotherapy and optimal pain therapy are the main points of rehabilitation.
Read a lot more information on this topic at: Operation of a herniated disc in the lumbar spine
Duration of a herniated disc in the lumbar spine
The time it takes to heal after a herniated disc depends on the severity of the incident and the treatment.
Just about ten percent of all herniated discs must be treated surgically (through an OP), although not always pain relief through a Disc surgery can be achieved and the pain can return.
The pain after a herniated disc can persist for a very long time. The duration of the healing process can actually only be by the person concerned himself to be influenced. Only those who become active themselves and move a lot can get rid of the pain. Any sporting activity that builds up the back and abdominal muscles is helpful to combat the pain. Regular walks, targeted training at back school, swimming or cycling can influence the duration of back pain by each person affected.
An operation (OP) or painkillers can make movement easier or even make it possible again, but how long the problems and discomfort caused by the herniated disc last is mainly determined by a active sports program after the herniated disc decided. The more stable the Back muscles is, the more stable and healthy the intervertebral discs are.
Read a lot more information on this topic at: Duration of a herniated disc
Can you prevent a herniated lumbar disc?
Provided a few points are observed, a herniated disc of the lumbar spine can be avoided or prevented.
gymnastics and Sports, how swim or cycling, strengthen the Back muscles and so relieve the lumbar spine. Anyone who sits for a long time in their professional life should exercise a lot to compensate. Anyone who is also overweight should reduce their weight, as being overweight is one of the risk factors for a herniated disc in the lumbar spine.
But factors that cannot be influenced, such as genetic quality and spinal accidents, also play a role and cannot always be prevented.