Pseudarthrosis
Synonyms of pseudarthrosis
- False joint
- Nearthrosis
- Nonunion
- Scaphoid pseudarthrosis
definition
A pseudarthrosis is understood after a break (fracture) or degenerative bone changes, lack of healing and the failure of the defective bone parts to grow together with the formation of a false joint.

When does one speak of pseudo-osteoarthritis?
The term pseudarthrosis means something like "wrong joint" and describes a broken bone (fracture) that has not completely healed. Due to the lack of healing, the two ends of the fracture do not grow together and the affected bone shows a discontinuity (interruption).
It usually takes about four to six weeks for a broken bone to heal completely, although this period of time depends heavily on the location and severity of the break. Fractures that have not healed after four to six months are called pseudarthrosis.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- Lumedis - orthopedic surgeons
Kaiserstrasse 14
60311 Frankfurt am Main
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see Lumedis - Orthopedists.
Causes / forms
The causes of pseudarthrosis are often diverse.
An interplay of many factors ultimately leads to delayed healing or a complete failure to heal the fracture.
The most common cause is insufficient blood supply to the bones, which delays or prevents the bone ends from growing together quickly after a fracture or trauma.
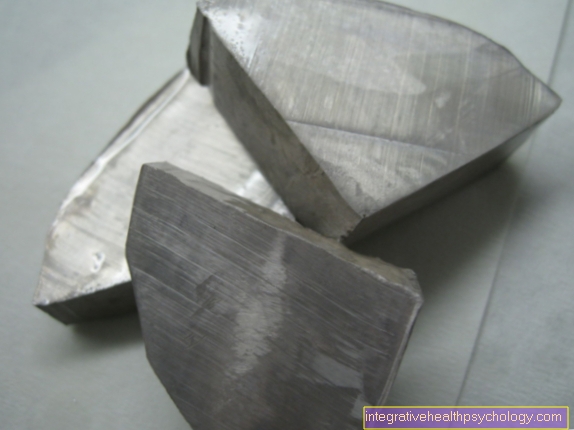
A second common trigger after a fracture and a corresponding surgery in which metallic material is inserted and screwed in to stabilize the bone ends is instabilities.
When the metal (Osteosynthesis material) is either attached incorrectly or, if it loosens again after a short time, rapid healing and the bone from growing together is prevented - a pseudarthrosis occurs.
If the existing bone ends are too far apart and the fracture gap cannot be bridged, this also leads to pseudarthrosis.
Another important point for the development of pseudarthrosis is incorrect behavior after an operation, which usually results in too early and excessive stress on the affected person Joint consists.
Unhealthy lifestyle, such as excessive alcohol consumption, Smoke or poorly adjusted diabetes can also contribute to the development of a pseudarthrosis.
It will different shapes a pseudarthrosis:
at the so-called atrophic pseudarthrosis A bony reaction is completely absent and therefore also a healing prospect.
At a avascular pseudarthrosis In principle, new bone is already formed, but the adequate supply of blood that contributes to healing is missing (lack of blood in the bones).
The third form, the hyperreactive bone formation, there is excessive new bone formation, which admittedly progresses quickly but is severely limited in stability. Although the bone grows together quickly, it is not really resilient and there is always the risk of a new bone fracture.
Bones that become infected after a fracture / broken bone can also develop a pseudarthrosis. The reason also called septic pseudarthrosis The designated process are the invading pathogens that prevent the desired healing process.
What is hypertrophic pseudarthrosis?
Pseudarthroses are divided into hypertrophic (vital) or atrophic (avital) pseudarthroses. This classification refers to the type of scar tissue that is formed by the bone as part of wound healing. Most pseudarthrosis cases are hypertrophic. This means that the bone is well supplied with blood and that healing should actually go well. However, due to insufficient immobilization of the fracture, the fracture cannot fully heal. There is an excessive formation of scar tissue, which forms in an uncontrolled manner around the fracture site. Depending on their radiological appearance, hypertrophic pseudarthroses can be further subdivided into “elephant foot” and “horse foot” pseudarthroses.
What is arthrophic pseudarthrosis?
In the case of atrophic pseudarthrosis, the bone is no longer adequately supplied with blood. As a result, no new bone tissue can form at the fracture site and the fracture does not heal. Infections of the bone, increased bone breakdown (osteolysis) or dead (necrotic) bone material that is still in the fracture gap can cause atrophic pseudoarthrosis.
You can recognize pseudarthrosis by these symptoms
The development of a pseudarthrosis is gradual.
Thus, the symptoms are also delayed.
Furthermore, not all symptoms described have to occur.
The common occurrence represents the full picture of a severe pseudarthrosis. This includes reddening and swelling over the affected joint or the broken bone area, pain that can occur both at rest and when moving.
When moving, the symptoms usually occur earlier.
In the case of advanced pseudarthrosis, pain at rest can also occur.
Is the course of a pseudarthrosis septic, i.e. if pathogens are involved, systemic symptoms such as high fever and a reduction in general health occur.
Since the stability of the bone is sometimes greatly reduced in pseudarthroses, it can also happen that axial deviations of the bone occur, which are also partially visible.
Bone instability is also noticeable in the reduction in strength and in the ability to move the affected bone segment manually.
Pseudarthrosis pain
Pseudarthrosis usually causes severe pain. The pain begins with the disease and does not improve, or only slightly, without appropriate therapy. This form of pain is called chronic.
In addition, the affected extremity is restricted in movement, which means that the patient falls into a relieving position. This relieving posture often leads to severe muscle tension, which causes further pain. Patients who still suffer from pain after a treated fracture should consult a doctor in order to rule out the presence of pseudarthrosis.
Diagnosis
In addition to the physical examination, diagnostic imaging offers the greatest safety value for diagnosing pseudarthrosis.
In most cases, a simple x-ray of the affected area is taken. In the case of a pseudarthrosis, a still existing fracture gap and possibly axis deviations of the bone would be seen.
In addition, cysts can be made visible: the lack of healing causes the bone to react with excessive, undirected bone formation, which can be seen in the form of so-called rubble cysts at the edge in the X-ray image.
If a pseudarthrosis cannot be confirmed in an X-ray image, a magnetic resonance tomography can be performed, which shows an even more detailed representation of the bone and the surrounding soft tissue.
therapy
Since pseudarthrosis is sometimes accompanied by severe pain, it is important to make the patient pain-free.
On the one hand, this can be done with medication (painkillers), on the other hand, also through physical cold or heat therapy.
It is important that the joint or the broken bone section is spared and not stressed.
In most cases, immobilization is achieved by applying a cast. This should be worn permanently for six weeks.
After approx. 4 weeks, a control radiograph should be taken to document whether the fracture gap has reduced and whether the bone formation is now more directed.
If this is not the case, another operation must be performed.
In the case of hyperreactive pseudarthrosis, attempts are made to increase the stability by means of a newly inserted intramedullary nail or a plate fixation.
The area that produces the excess bone must not be removed, otherwise the total bone production can be reduced. In avascular pseudarthrosis, undersupplied bone tissue must be removed and the bone circulation restored and improved by introducing cancellous bone, etc.
If bone formation is severely reduced (atrophic pseudarthrosis), large parts of the cortex of the bone must be removed and filled with cancellous bone in order to stimulate bone formation.
Read more on the subject at:
- proff® pain cream
Shock wave therapy
In some cases, pseudarthrosis does not have to be operated on, but can be treated with extracorporeal shock wave therapy (ESWT). In pseudarthrosis, bone formation at the fracture site is disturbed and the regeneration of the bone can be promoted with the help of shock waves. A device that generates pressure waves is placed over the skin on the affected area. The pressure waves penetrate the body and act on the bones. This treatment principle is mainly known from urology: there it is used to break up kidney and ureter stones.
Find out more about the topic: Shock wave therapy
When does a pseudarthrosis have to be operated?
Whether a pseudarthrosis has to be operated on depends on the findings. In most cases, however, the healing disorder is treated surgically. Above all, atrophic pseudarthroses, in which parts of the bone are no longer adequately supplied with blood, must be operated on so that the bone is made permeable again and does not die. Here it is important that the operation is carried out as soon as possible after the diagnosis of the pseudarthrosis. Infection pseudoarthroses must also be treated with an operation.
Typical locations of pseudarthroses
Pseudo-osteoarthritis in the thigh bone (femur)
Any fracture of the thigh bone (femur) is usually operated on and corrected using osteosynthesis (i.e. with the help of plates, screws or nails). Reduced blood flow or non-union of the infection are possible complications of this surgical procedure. As a result, an atrophic non-union forms and the defective femur cannot heal completely. The treatment of this complication consists of a new operation (revision operation), in which the old implant is removed and the fracture site is thoroughly cleaned. Excess scar tissue or necrotic material is cut out and the fracture site is treated with an intramedullary nail.
Pseudoarthritis of the shin (tibia)
In severe and complicated fractures of the shinbone (tibia), impaired blood flow to the bone tissue can lead to pseudarthroses. But hypertrophic pseudarthroses also occur when the affected leg is subjected to incorrect mechanical loading. Very rarely, a pseudarthrosis in the shinbone is congenital, the so-called congential tibia pseudarthrosis. In this disease, the bone metabolism is disturbed and the affected people suffer from pseudarthroses in the shin and fibula in the first years of life. The bones in the lower leg continue to bend and lead to severe malformations.
Pseudarthrosis in the upper arm bone (humerus)
Fractures of the upper arm bone (humerus) can either be treated conventionally (i.e. by resting) or surgically. Problems in therapy, such as a lack of physical restraint, incorrect procedures during osteosynthesis or loosening screws or plates, can lead to the development of pseudarthroses. Patients report persistent pain that has not improved weeks after initial treatment for the fracture. Humeral pseudarthrosis is usually treated surgically: the bone fracture is brought together in a stable manner and fixed using osteosynthesis. Complicated shoulder fractures may need to be treated with a shoulder prosthesis.
Pseudarthrosis in the navicular bone

In medicine, a bone fracture that does not grow back together is called pseudoarthrosis, whereby the two movable bone fragments have a kind of "wrong joint“ (Pseudoarthrosis) form.
The scaphoid bone (Scaphoid bone) belongs to the carpal bones, so a scaphoid fracture makes up three quarters of all carpal fractures and occurs, for example, in the context of a fall on the hyperextended (dorsiflexed) Wrist.
If a scaphoid fracture is overlooked or not adequately treated, pseudoarthrosis can occur. The bone parts no longer grow firmly together and small movements are possible between the fragments. As a result, the wrist collapses with subsequent incorrect loading and osteoarthritis of the hand.
Many sufferers feel only moderate exercise-related pain that is localized on the thumb side of the wrist. A reduction in strength can also occur.
An X-ray in two planes is groundbreaking in the diagnosis of pseudoarthrosis of the scaphoid bone. Since in many cases a pseudoarthrosis is not visible here, another becomes Admission after Stecher made with the hand clenched into a fist and after ulnar (towards the little finger) is held abducted.
A computed tomographic image of the scaphoid bone is made for surgical planning or more precise assessment. It is crucial that the examination is carried out through the longitudinal axis of the navicular bone in order to obtain as precise a statement as possible about the malposition, the size of the defect and the location of the pseudarthrosis.
In the case of older pseudarthroses and an urgent suspicion of insufficient or absent blood flow to the bone parts, magnetic resonance imaging of the hand (MRI of the hand) the appropriate method for assessing blood flow with contrast medium.
Even if the affected person has only slight pain or discomfort from the pseudoarthrosis, the navicular pseudoarthrosis should always be surgically stabilized. The focus here is on avoiding long-term damage such as osteoarthritis resulting from incorrect loading. The operation achieves a bony reunification of the fragments and the restoration of the original navicular shape. Usually the defect has to be filled with functional bone material from the iliac crest or the radius.
If the remaining bone fragment is not adequately supplied with blood vessels (vascularized), the bone block to be transplanted, including the vascular style, is removed using microsurgical technology and transplanted into the navicular bone.
The operation is usually associated with an inpatient hospital stay of about three days, followed by a four to six week plaster immobilization. An osseous development of the navicular bone should then be visible in the X-ray after three months.
Further information is available under our topic: Scaphoid fracture
Pseudoarthrosis on the ribs
After a broken rib (fracture) so-called pseudoarthrosis can occur if the healing process is inadequate. The bone fragments that have not grown together are mobile and thus form a "wrong joint“.
The most common cause of the bone fragments not growing together is inadequate blood flow. Incorrect behavior after a bone fracture or an operation, such as too fast loading and too short a rest period for the patient, can also be the reason for the development of pseudoarthrosis. Risk factors are also:
- an unhealthy lifestyle
- excessive alcohol consumption
- Smoke
- Diabetes mellitus.
The symptoms of pseudoarthrosis, like the disease itself, often appear insidious at first. These include redness, swelling and pain, which mainly occur when coughing or sneezing, and then also when resting. Furthermore, the bone stability can be greatly reduced, this axis deviation can also be visible from the outside.
Conservative treatment methods for pseudoarthrosis, such as immobilization using a cast, are difficult to manage in pseudoarthrosis of the ribs. If the person concerned feels pain and restricted mobility, the pseudoarthrosis can be treated surgically. A relatively new, non-invasive procedure is a low-frequency ultrasound treatment that is applied daily over a period of several months and is intended to stimulate bone growth even in older pseudoarthroses. The treating doctor regularly records the success of the treatment with x-rays.
Pseudarthrosis of the clavicle (collarbone)

Fractures of the collarbone (Clavicle) are usually treated conservatively. In the case of the clavicle, this usually means a rucksack bandage, which is left in place for 3 - 4 weeks. Pseudarthrosis can develop in around 2 - 6% of cases. In surgical procedures, the pseudarthrosis rate is even higher (which is mostly due to more complicated fractures that require surgery). 4,000 - 8,000 patients are affected by this clinical picture every year in Germany alone.
As a result, pain and decreased shoulder function are very common complaints. Factors that increase the risk of developing pseudarthrosis of the clavicle are, above all, complicated fractures, infections and inadequate surgical care.
Whether and how a pseudarthrosis of the collarbone needs to be treated depends primarily on whether the patient has any symptoms at all. If the pseudarthrosis is asymptomatic, i.e. it does not cause any complaints of any kind, it can be left untreated or treated conservatively. If this is not the case, surgery is indicated. The broken ends are usually connected to one another by metal plates and screws. Another surgical procedure that can be used is intramedullary fixation, for example the use of a nail located in the bone marrow. If this comes into question, there are some advantages (including cosmetic), such as a smaller surgical scar. In most cases, the implants are finally removed a few months to 2 years after the operation.
Nonetheless, even after a successful operation and good healing of the injury, many patients still complain of symptoms, especially pain when moving the shoulder.
Pseudarthrosis in the foot
The reasons for developing pseudarthrosis on the foot are similar to those of other bones. Inadequate or late treatment of the fracture, as well as too early loading of the injured foot, is a common cause of the development of a false joint.
Especially with the so-called Jones fracture, the probability of developing pseudarthrosis is particularly high; especially if the therapy is conservative, for example with the help of a cast. The Jones fracture is a near-base fracture of the 5th metatarsal, i.e. a fracture at the end of the metatarsal on the outer edge of the foot facing the heel.
Pseudoarthrosis is noticeable through pain when walking and abnormal mobility of the affected bone.
In order for the fracture point to heal completely, it must then be compressed using a screw or tension strap.It may be necessary to bring in bone material from the iliac crest in order to achieve acceptable healing of the fracture. In any case, an injury to the tarsometatarsal joint (the joint between the tarsus and metatarsal bones) must be ruled out by x-ray during treatment.
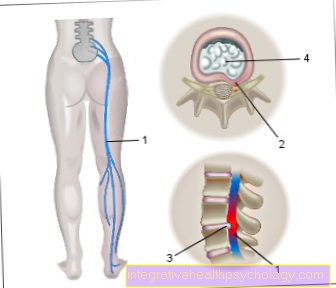
Pseudarthrosis of the lumbar spine
Pseudoarthroses of the spine in general usually arise as part of operations or as a result of fractures of the vertebral bodies. As a result, false joints arise which, unlike real joints, are not covered with cartilage.
Severe pain, especially when moving, as well as increased mobility and instability are the consequence. An operation is usually the only treatment option that allows the two fragments to grow together properly.
Summary
Pseudarthrosis is always spoken of when, after fractures or operations on the bones, the healing process does not take place to the extent that it should, for various reasons.
If there is excessive but undirected new bone formation, one speaks of reactive pseudarthrosis.
If the problem is a lack of blood circulation, one speaks of an avascular pseudarthrosis, and if hardly any bone formation occurs, the clinical picture is called atrophic pseudarthrosis. Undersupply of blood and loose or improperly attached metal (Osteosynthesis materials) are among the most common causes of pseudarthrosis.
The patients usually complain of pain at rest and when moving, and they have swelling and redness over the affected area. Furthermore, there is a functional restriction.
In most cases, an X-ray of the affected area is taken as a diagnosis. It shows the remaining fracture gap as well as excessive bone formation, mostly at the edge. Cysts can also be seen.
After diagnosing pseudarthrosis, the corresponding joint should definitely be immobilized with a cast for six weeks and cooled or warmed by physical therapy.
Medicinal analgesics (pain relievers) help minimize the pain.
Another x-ray is taken after 4 weeks to check bone formation. If this is not sufficient, a new operation is usually necessary, in which new osteosynthesis material and bone-forming cancellous bone are introduced and bone tissue that is not supplied with blood is removed.