T lymphocytes
definition
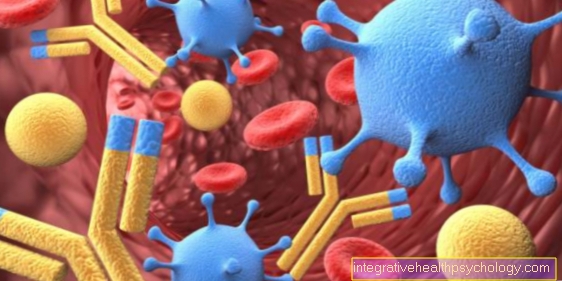
T lymphocytes are cells of the immune system and can be found in the blood, among other things. The blood is composed of the blood cells and the blood plasma. The blood cells are further subdivided into erythrocytes (red blood cells), leukocytes (white blood cells) & thrombocytes (blood platelets). T lymphocytes are part of the white blood cells and can also be subdivided into T killer cells, T helper cells, T memory cells, cytotoxic T cells and regulatory T cells.
The T lymphocytes are also known colloquially as T cells. The letter "T" stands for the maturation site of the T lymphocytes, namely the thymus. It is located in the upper area of the chest and is an important organ for the immune defense. The T lymphocytes are assigned to the adaptive, i.e. the acquired immune system. This means that they need some time to be able to react to pathogens, but as a result they can do this in a more targeted manner and therefore usually more effectively than the innate defense system.

anatomy
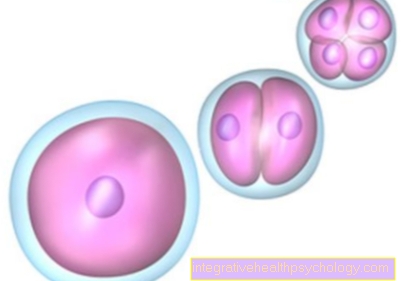
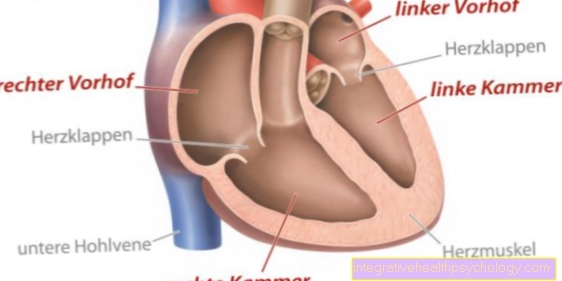
The T lymphocytes are spherical in shape and about 7.5 micrometers in size. They consist of a round, slightly indented cell nucleus surrounded by cytoplasm. In addition, more ribosomes can be found inside the cell.
tasks
The main task of the T lymphocytes is the immune defense. The non-activated T-lymphocytes are distributed over the blood and the lymphatic tissue in the entire organism and control unnatural changes in the body's own cells. Such pathological changes can be caused, for example, by invading pathogens or by mutations in the genetic material. In adults, around 95% of non-activated lymphocytes are located in the thymus, spleen, tonsils and lymph nodes.
If pathogens such as bacteria or viruses enter the body, they are first recognized and bound by other defense cells of the immune system. These include macrophages, B cells, dendritic cells and monocytes. Only the connection between these defense cells and the pathogens trigger an activation of the T lymphocytes. The T-lymphocytes can then finally recognize the pathogen and classify it as foreign. However, each T lymphocyte can only recognize certain pathogens. The identification between the pathogen and the T-lymphocytes takes place via so-called MHC molecules, which are on the surface of pathogens and certain membrane components of the T lymphocytes.If these two surface features fit together according to the lock and key principle, the T lymphocytes are activated and can react accordingly to the pathogens.
However, the various subspecies of T lymphocytes react to the pathogen with different mechanisms, depending on the type of pathological change. The T-killer cell reacts by directly destroying the pathogens, while the T-helper cells attract further immune defense cells by releasing messenger substances, which in turn are responsible for eliminating the pathogens. The regulatory T cells, on the other hand, primarily prevent the pathogens from spreading to other, endogenous cells. By releasing various enzymes, cytotoxic T cells destroy pathogens. The memory T cells do not contribute directly to the elimination of the pathogens, but they still play a decisive role because they store the properties of the specific pathogens. This storage allows a faster and more targeted immune response to occur the next time it is penetrated.
Read more on the subject under: Lymphatic organs
Causes an increase in T lymphocytes
The causes of an increased T-lymphocyte count can be various diseases. If an infection occurs, the lymphocytes multiply via the mechanisms mentioned above and, as a result, increasingly enter the bloodstream. The percentage of T-lymphocytes can then be determined by blood laboratory tests. The normal value of the lymphocytes is between 700 and 2600 lymphocytes per microliter and thus has a proportion of the white blood cells between 17% and 49%. Based on the blood laboratory measurements, conclusions can then be drawn as to whether a bacterial or viral infection is present and to what extent T-lymphocyte formation and release is proceeding properly. Daily rhythm fluctuations are quite natural. The number of lymphocytes is usually slightly higher at noon and in the evening, while the lowest value is available in the morning.
Viral infections (e.g. rubella, glandular fever), certain bacterial infections (e.g. whooping cough, tuberculosis, typhoid), fungal infections (e.g. pneumocystis, candida) and various types of cancer (e.g. leukemia, lymphoma) can increase the T-lymphocyte count. In addition, an increased lymphocyte count can be an indication of an overactive thyroid.
Causes of a low level of T lymphocytes
A low number of T lymphocytes is often caused by diseases or malfunctions of the immune system. These can be both acquired and congenital. Genetically inherited diseases can weaken the immune system and thus the formation of T lymphocytes. However, the immune deficiency and thus the reduced formation of T lymphocytes can also be caused by acquired infectious diseases (e.g. measles) or cancer. These can specifically attack and destroy the lymphocytes. These include AIDS and tuberculosis, for example. In addition, the medication of immunosuppressants (e.g. glucocorticoids), cortisol, cytostatics and steroids can lead to a decrease. Other causes include chronic liver diseases (e.g. cirrhosis of the liver, hepatitis C), burns, autoimmune diseases, renal insufficiency and iron deficiency anemia.
Leukemia is a particular cause of a reduced number of T lymphocytes. When the disease occurs, this initially causes an increase in T lymphocytes. This is dangerous for the organism, as the high number of lymphocytes may also attack the body's own healthy cells. When treating leukemia with chemotherapy and radiation, attempts are made to reduce the number, which can easily lead to the lymphocytes falling below the normal value.
Cytotoxic T cells
The cytotoxic T cells are a subgroup of the T lymphocytes and thus belong to the acquired immune system. Their task is to identify infected cells within the organism and kill them as quickly as possible. Like the rest of the T lymphocytes, they are formed in the bone marrow, then migrate to the thymus, where they are finally sorted out again and then develop into mature T lymphocytes. The cytotoxic T-lymphocytes are finally released into the bloodstream, where they ultimately interact with various endogenous cells and thereby check their condition. If it is an infected or defective cell, the cytotoxic T-lymphocytes are able to dock onto the MHC molecules of the infected cells via their surface-mounted T-cell receptors and by releasing Perforin (protein) and Granzyme (protease enzyme) kill them.
Anti-human T lymphocyte immunoglobulins
Anti-human T lymphocyte immunoglobulins are antibodies produced in the laboratory that are used to prevent possible transplant rejection or are only used after an organ or stem cells that have already been transplanted have been rejected.
The reason for the administration of anti-human T lymphocyte immunoglobulins is that there are occasional complications with stem cell transplants. The danger is that the transplant can no longer pursue its actual tasks in the foreign body and possibly attacks the recipient body. The T lymphocytes play a role in that they are also introduced into the recipient body through the transplantation. The implanted T lymphocytes now work in two ways. On the one hand, they go about their usual job by attacking the infected cells that are present. On the other hand, they can trigger the so-called “transplant-versus-host reaction”, as the recipient organism may consider them foreign and trigger an immune reaction against them.
A drug designed to prevent or treat these reactions has been researched and found in anti-human T lymphocyte immunoglobulin. This drug is obtained from rabbits.
Read more on the subject under: Transplantation
Activation of T lymphocytes
The activation of the T-lymphocytes takes place via an interaction between the T-cell receptors, which are located on the lymphocytes, with the appropriate antigens of the exogenous or mutated cells. The T-cell receptors can only recognize the antigens if they are presented by so-called antigen-presenting cells.
However, further factors are necessary for a stable bond. These include glycoproteins (CD4 and CD8) on the surface of the T lymphocytes and proteins (MHC1 and MHC2) on the surface of the antigen-presenting cell. It should be noted that the T helper cells only have CD4 receptors, which in turn can only bind to MHC2 molecules. Accordingly, CD8 receptors can only bind MHC1 molecules. The CD8 receptors are mainly found on cytotoxic cells, but can also be found on the T killer cells or the regulatory T lymphocytes. An antigen-independent costimulation is also required for activation. It is initiated by surface proteins and originates from the same antigen-presenting cell.
After the T lymphocytes are finally activated, a cellular response can occur. This consists in the fact that various messenger substances, the interleukins, are released and as a result macrophages, T killer cells or cytotoxic cells are activated. They are then able to eliminate the cells foreign to the body through various cell mechanisms. In addition, the interleukins can stimulate the production of antibodies, so that more can be reacted to the pathogens.
Standard values
The T-lymphocytes in adults usually make up 70% of the total number of lymphocytes in the blood. However, fluctuations between 55% and 85% are also absolutely within the normal range. This means that the normal value is between 390 and 2300 cells per microliter. Small fluctuations are quite natural. For example, the number of lymphocytes can increase due to stress, physical activity or cigarette consumption.
T lymphocytes in cancer
T-lymphocytes can also play a crucial role in cancer. The task of the T-lymphocytes is to recognize and destroy foreign or mutated cells. Cancer is a disease in which the body's own cells multiply in a malignant and uncontrolled manner. The problem with cancer is that the T lymphocytes do not regard the tumor cells as foreign, but as endogenous and are therefore tolerated by the immune system. The T-lymphocytes cannot recognize the mutated cancer cells and therefore cannot fight them. The latest research has now developed so-called CAR-T receptors that can specifically bind to cancer cells. These receptors should ultimately enable the T lymphocytes to recognize the cancer cells.
Read more about this under: Cancer
T lymphocytes in multiple sclerosis
Multiple sclerosis is a disease that affects the nervous system. Multiple sclerosis is caused by an autoimmune disease in which the immune system is improperly regulated. The T cells and the B cells play a role in this. In addition to the T cells, B cells represent other cells of the body's own immune system. In multiple sclerosis, the T and B cells mistakenly attack the cells surrounding the nerve fibers, the myelin sheath. The myelin sheath is responsible for the rapid nerve transmission of information. If they are damaged, the forwarding is worsened or possibly even completely prevented.