Scleroderma
What is Scleroderma?

The word comes from ancient Greek and means "hard skin". Scleroderma is a rare inflammatory rheumatic disease from the group of collagenoses, which can take on mild and severe, life-threatening forms.
The disease affects the small blood vessels and connective tissue.
Here collagen is deposited, which is noticeable as hardened skin foci.
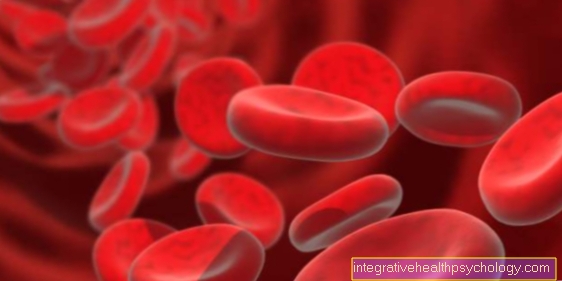
Scleroderma is an autoimmune (Greek cars = self) Disease, which is why specific proteins (Autoantibodies) are detectable in the blood.
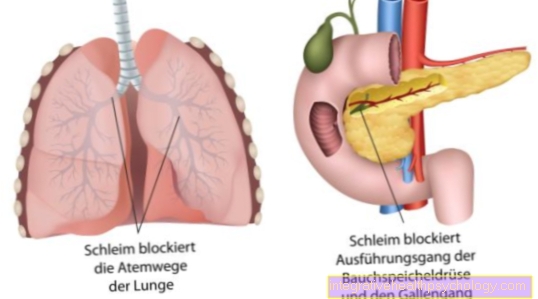
There are different forms of progression, either only affecting the skin (localized scleroderma), while in other forms the internal organs such as the gastrointestinal tract, lungs, kidneys or heart are affected (Systemic scleroderma).
Classification of scleroderma
Localized scleroderma occurs in three forms:
Morphea:
coarse foci that have too little or too much pigment on the inside and are surrounded by reddening on the outside (Erythema), mainly on the trunk
Generalized morphea:
like morphea, but flowing together and wider, the face is free
Linear scleroderma:
Ribbon or groove-shaped foci, mainly localized on the extremities and head
Systemic scleroderma exists in two forms:
Diffuse scleroderma:
distributed all over the body, spreading rapidly, internal organs are affected early on
Limited scleroderma:
initially insufficient blood supply to individual fingers (initial Raynaud's phenomenon), then involvement of the extremities and face, later of the internal organs, often in connection with the so-called CREST syndrome
(C = calcinosis, a calcium deposit in the skin; R = Raynaud's phenomenon, see above; E = (o) esophageal motility disorder, a movement disorder of the esophagus; S = sclerodactyly, a hardening of the skin of the fingers with impaired function of the fingers; T = telangiectasia, a local enlargement of the capillary vessels of the skin)
Causes of Scleroderma
The exact cause of the disease is not yet known.
A familial occurrence has been described in isolated cases.
The increased incidence of systemic scleroderma among coal and gold miners has also been reported.
At the molecular level, so-called HLA antigens of the type DR1, DR2 or DR5 are sometimes increasing. There is also much evidence of a cell-mediated autoimmune reaction, which can damage the inner wall of the blood vessels (Endothelial damage) leads.
Acquired genetic changes are also common.
A causal relationship with the above-mentioned influences and scleroderma has not yet been established.
diagnosis

The diagnosis can be made using a laboratory test.
More than 95% of people with scleroderma are Antinuclear Antibodies (ANA) elevated.
These are proteins produced by the body that attack the body's own cell nuclei. If you only test for "ANA“In general this is relatively unspecific.
ANA can also e.g. in the Rheumatoid arthritis be positive.
Therefore, you take a closer look and look for very specific ANAs, for example anti-Scl70, which is increased in systemic scleroderma.
At the CREST syndrome Anti-centromere antibodies can be used for diagnostics as they can be found in 70-90% of patients with the syndrome.
In the blood count, a Anemia exist, as it can lead to iron deficiency in the case of intestinal involvement. If the kidneys are involved, there may be an increased serum creatinine, as well as blood or protein admixture in the urine.
Frequency distribution
The incidence rate is 1-2 people out of 100,000 / year.
Usually the age at the onset of the disease is 40-60 years.
The incidence of the disease in the population is less than 50 in 100,000.
Women are by a factor of 4 more often affected than men.
Symptoms of scleroderma
Scleroderma spreads primarily painlessly.
Occasionally there is muscle and joint pain.
The disease is difficult to diagnose because it is fast, slow, and self-stalling (at morphea) Can give course forms as well as a wide variety of symptom compositions.
Depending on which organs are involved, there are different complaints. Also because the disease is very rare, it is often not considered when unspecific symptoms occur.
The early symptom of systemic scleroderma is primarily a circulatory disorder in the hands (Raynaud's phenomenon), which can precede the disease up to two years.
The tongue can also be shortened. Later, water retention (initial edema) especially come into contact with.
Arms, face and trunk can also be affected. During the so-called induration phase (Induration phase), which lasts for several weeks and is fully developed after one to two years, the water retention recedes and the skin becomes thicker, immovable and hard as a board.
Collagen fibers have deposited in the skin.
Facial expressions are difficult (Mask face), the nose becomes pointed, the mouth wrinkles in a star shape and becomes small (Tobacco pouch mouth). The fingers lose mobility, become thin, stiff (Madonna fingers) and fixed in the claw position.
The involvement of tendon sheaths and ligaments can lead to nerve damage or carpal tunnel syndrome.
In diffuse systemic scleroderma, the process mentioned above takes place within a few weeks.
The limited systemic scleroderma is slower and occurs mainly on the fingers and arms.
In the variant of CREST syndrome, calcinosis, Raynaud's phenomenon, esophageal motility disorder, sclerodactyly and telangiectasia (for an explanation see introduction).
In both forms, the gastrointestinal tract is affected early in 80% of patients. Acid regurgitation (Reflux) and its consequences (Reflux esophagitis) come.
Indigestion, constipation, and bowel sacs (Diverticulum) occur.
The second most common cause of disease in the internal organs is the lungs.
There is a hardening of the connective tissue of the lungs (interstitial pulmonary fibrosis).
Heart and kidney involvement predominantly occur in the diffuse form.
Treatment of scleroderma

Most therapies are not very effective and do little to stop the progression of scleroderma.
High-dose immunosuppressants such as glucocorticoids, methotrexate, ciclospoprine A, azathioprine and chlorambucil could not show any clear benefit.
It is therefore now believed that the disease cannot be caused solely by one's own immune system, as otherwise these drugs would have to have a good effect.
Drugs such as? -Interferon, thymopentin, isoretinoid, N-acetylcysteine or D-penicillamine were also not particularly effective.
Often, severe side effects force you to discontinue the medication.
A therapy with D-penicillamine is tried most often.
Glucocorticoids can also be useful under certain circumstances, e.g. have pulmonary fibrosis, edema, or arthritis.
Rituximab and tocilizumab, which are also used for other autoimmune diseases, occasionally show success in treatment.
Research is currently being carried out on therapies using bone marrow transplantation and blood washing (Apheresis).
Caution is required when measuring the success of the therapy.
Often the transition of the disease into the so-called atrophic phase, in which the water retention recedes, the skin becomes hard and contracts, looks like a regression of the symptoms.
It is above all supportive, general measures that help the patient in particular and have a favorable effect on the symptoms.
Physiotherapy helps prevent contractures. If Raynaud's phenomenon is present, warm hands should be ensured.
Kick wounds (Ulceration) on the hands, they should be well taken care of.
As a preventive measure for ulcerations, e.g. the active ingredient will be bosentan.
If high blood pressure begins as a result of the changes in blood vessels, therapy should be given with an ACE inhibitor.
Phototherapy (PUVA) can soften the foci of sclerosis and ensure better functionality.
Course and prognosis
The course of the disease is difficult to predict and cannot be deduced from the constellation of symptoms.
It can happen that unforeseen very serious courses occur that lead to death within months.
However, the morphea is not life threatening.
Women generally have a better prognosis than men.
In systemic scleroderma, the infestation of the internal organs is decisive.
The limiting form generally has a good prognosis.
However, 10% of patients develop high blood pressure in the pulmonary circulation (pulmonary hypertension), which dramatically increases the death rate in this patient group.
The diffuse form has a rather poor prognosis.
If the kidney is also affected, after ten years only 30% of these patients are still alive, the lungs are hardened (fibrosed) about 50% survive the next 10 years.
In patients without heart, lungs or kidney involvement, the 10-year survival rate is 71%.
history
Descriptions of symptoms that now make us think of the diagnosis of scleroderma can already be found in the writings of Hippocrates (460-370 BC). However, the descriptions were rather imprecise.
Carlo Curzio first precisely formulated the constellation of symptoms in Naples in 1753. For example, he described the hardness of the skin, the tightness around the mouth and the hardness around the neck.
In 1847 Elie Gintrac coined the term "Scleroderma". He considered the disease to be a pure skin disease. It was only William Osler who realized that the internal organs are also involved in the disease process.