SSRI
What are SSRIs?
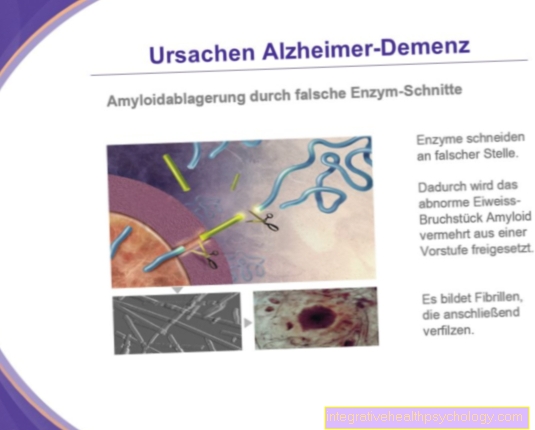
SSRI stands for Selective Serotonin Reuptake Inhibitors. These are drugs that prevent serotonin from being reabsorbed. Serotonin is an endogenous transmitter substance, which is produced from the amino acid tryptophan mainly in the central nervous system and in the gastrointestinal tract.

introduction
As a transmitter, serotonin mediates important functions in the body. A malfunctioning serotonin metabolism has massive effects on health. Mental illnesses such as anxiety disorders, obsessive-compulsive disorders or eating disorders are associated with serotonin dysfunction. But also purely physical symptoms such as migraines, nausea and vomiting can result from an incorrect or non-existent production of serotonin.
Drugs belonging to the group of selective serotonin reuptake inhibitors are used when there is too little serotonin available.
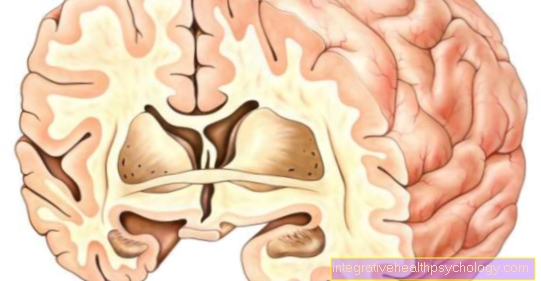
Neurons that produce serotonin consist of a presynapse (pre = before), a postsynapse (post = after) and a synaptic gap between them. The transmission of messenger substances at a synapse always follows the same principle. Tiny transport vesicles filled with the messenger substance (Vesicle) free the corresponding substance. This is then located in the synaptic gap and activates the postsynapse from there so that the signal can spread further. Then the transmitter material from the synaptic gap is taken up again into the presynapse and the process can run again.
However, if there is a deficiency in the transmitter substance, for example a serotonin deficiency, there is not enough messenger substance in the gap and the transmission of the signal is interrupted.
This is exactly where SSRIs attack. In the case of the selective serotonin reuptake inhibitors, as the name suggests, only the reuptake (reuptake) of serotonin is actually inhibited (selectivity).
When are SSRIs used?
SSRIs are primarily used to treat mental disorders. Depression is the top priority here, as this mental illness is based on a serotonin deficiency.
In addition to the therapy of depression, SSRIs are also used for obsessive-compulsive disorders such as compulsory cleaning (pathological cleanliness), compulsory order, compulsory control or other psychological compulsions.
Anxiety disorders can also be treated with SSRIs.
SSRIs are also used in the area of eating disorders. SSRIs are used to treat bulimia, although drugs have a minor role in the treatment of eating disorders compared to other mental illnesses.
How do SSRIs work?
SSRIs develop their effect by inhibiting a serotonin transporter at the presynapse. Under normal circumstances, this transporter would bring the serotonin from the synaptic cleft back into the presynapse, where it would be "packed" again in small transport vesicles and would be released again into the synaptic cleft when the synaptic transmission took place again. If the serotonin transporter is now restricted in its activity, the serotonin cannot get back into the synapse and “lies” in the synaptic gap.
However, since new serotonin is constantly being produced in the presynapse and prepared for release, the next time the transport vesicles are emptied, there is a real “serotonin avalanche” in the gap between the synapses. The accumulation of serotonin is then usually sufficient to ensure synaptic transmission.
At the postsynapse, the target structures of the substance, so-called receptors, are activated by sufficient amounts of serotonin. These receptors are located in the outer wall (membrane) of the postsynapse, penetrate it and are connected to small proteins inside the postsynapse. When serotonin docks to its receptor, its shape changes. This process also “moves” the small proteins inside, the signal is further amplified and continues “like a waterfall”. It can get to the respective target region in the body and develop the desired effect there. Serotonin transporters are not only found at the presynapse but also in some other places in the body such as the blood platelets (thrombocytes), which can lead to undesirable effects when using SSRIs.
More information about the topic Effect of antidepressants get here.
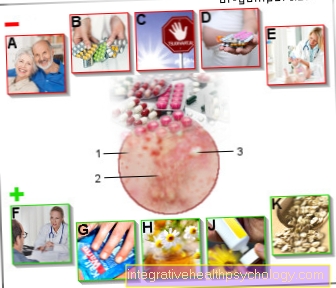
Side effects of SSRIs
In addition to the desired therapeutic effects, SSRIs have a number of unpleasant side effects.
Common symptoms are, for example, dry mouth, abnormal sweating, headache, tremors (tremor) as well as tiredness with simultaneous restlessness and insomnia.
A particularly annoying, undesirable effect of SSRIs is the often existing nausea. Serotonin binds to target structures in the digestive tract and in the vomiting center of the CNS, which stimulate the nausea (emetic) Act. This creates an annoying nausea that is sometimes associated with vomiting, loss of appetite and weight loss.
SSRIs can also have negative effects on potency and libido (pleasure in sexual intercourse).
Another effect that should not be underestimated concerns the bleeding tendency when taking SSRIs. Under physiological ("normal", healthy) conditions, serotonin has an important effect on the blood platelets (thrombocytes) by ensuring that they are stored together. In the event of an injury, many blood platelets “stick” together and thus form a plug that closes the wound and stops bleeding immediately after tissue damage. If a patient takes SSRIs, there is also an unfavorable inhibition of the serotonin transporter, which transports the substance into the blood platelets. If no serotonin arrives in the blood platelets, they can no longer fully aggregate, and the time until hemostasis is increased. Patients under the influence of SSRIs should therefore always pay attention to whether they bleed for an unusually long time.
In women, prolonged or heavy menstruation can indicate increased bleeding times.
Read detailed information on this topic under: Side effects of antidepressants
Serotonin Syndrome
The so-called serotonin syndrome brings particularly bad side effects of SSRIs. Overdosing with SSRIs and an excessive amount of serotonin in the body can lead to severe abdominal pain with fever, high blood pressure, palpitations and general restlessness. Serotonin syndrome can be fatal if untreated if the stress on the circulatory system exceeds tolerable ranges and the body's own regulatory mechanisms fail.
You can find much more information under our topic: Serotonin Syndrome
Weight gain from SSRIs
Weight gain tends to play a subordinate role with SSRIs compared to tricyclic antidepressants. On the contrary, there is usually weight loss due to a reduced feeling of hunger and reduced food intake. So, weight gain from taking SSRIs is not an immediate side effect of the drug.
In order for weight gain to occur, the patient must monitor their food intake. An intake of calories that is increased through consumption leads to the build-up of fat reserves and increases body weight. Patients should have a generally balanced diet and eat natural foods instead of highly processed junk food.
The choice of food also plays a role: protein-rich and fiber-rich products fill you up long-term, just as complex carbohydrates as in whole grain products. In the case of fats, unsaturated fatty acids such as those in fish and nuts should be used.
Physical activity also plays a big role in preventing weight gain. Increased activity increases consumption and metabolic performance and can support active weight control.
You might also be interested in our next article:
- Antidepressants without weight gain
- Causes of Obesity
Influence of SSRIs on libido
Sexual dysfunction is a possible side effect of SSRI therapy. Symptoms include impotence, premature ejaculation, anorgasmia (disorders of orgasm), and decreased or absent libido. How frequent and pronounced these side effects are depends largely on the choice of preparation.
Sexual dysfunction can, but does not have to, occur in every person treated. If the symptoms mentioned occur, switching to another SSRI may be advisable.
You might also be interested in our next article: Cause of erectile dysfunction
Which SSRI active ingredients are there?
Among the SSRIs are some often prescribed active ingredients. These include sertalin, paroxetine, fluoxetine and fluvoxamine.
Fluoxetine and fluvoxamine, marketed as Fluctin® and Fevarin®, have severe side effects and are therefore rarely prescribed when possible. Sertalin has few side effects and a good therapeutic range. Sertalin is sold as Zoloft®.
Zoloft® or its active ingredient, sertalin, is the most powerful SSRI. However, it has comparatively few side effects and also rarely interacts with other drugs. These properties make sertaline a commonly prescribed SSRI. The active ingredient is not only used for depression, but also for borderline syndrome and panic attacks.
Paroxetine is sold as Seroxat®, but the active ingredient causes significantly more side effects than sertaline and influences the effectiveness of some other drugs. For example, if you take paroxetine and hormonal contraceptives at the same time, there is a risk that the contraceptives, such as the birth control pill, will no longer work.
Fluoxetine is taken in tablet form as Fluctin®, the drug unfolds its full effect only after it has been exposed to a remodeling reaction in the liver.
Fluvoxamine triggers many side effects, but sexual dysfunction is rarely triggered by this active ingredient.
If you are taking SSRIs and other medications at the same time, you should always ask your doctor about possible interactions. Particular caution is required when taking SSRIs and inhibitors of monoamine oxidase (MAO), since both drugs together have a variety of interactions.
Read more about antidepressants at:
- Cipralex®
- Cipramil®
Citalopram
Another active ingredient in SSRIs, citalopram, is often prescribed. Medicines containing citalopram interact only weakly with other drugs, and the side effects are also minor compared to other active substances. Nevertheless, undesirable effects such as excessive sweating, diarrhea or fatigue often occur. Even small amounts of alcohol in connection with citalopram have hardly any side effects. The effect of citalopram only occurs after one to two weeks, so the drug is particularly suitable for long-term therapy.
Citalopram is used mainly for depression, anxiety disorders and panic attacks. The active ingredient is mostly used as a film-coated tablet, which must be taken once a day. Citalopram requires a prescription and must therefore be prescribed by a doctor.
Like other SSRIs, medication containing citalopram should not be discontinued on one's own initiative, as the dose has to be reduced slowly. Otherwise, sometimes severe withdrawal symptoms can occur.
Are you interested in this topic? Read more about this at:
- Side effects of citalopram
- Citalopram and alcohol
Mirtazapine
Mirtazapine is also used as an active ingredient in antidepressant drugs. However, this active ingredient does not belong to the group of SSRIs, rather it is one Alpha2 receptor blockers.
Alpha2 receptor blockers act on the receptors of the same name. These are located at the presynapse and usually have an inhibitory effect on signal transmission at the synapse. The alpha2 receptors usually prevent the release of messenger substances at the synapse. If this inhibiting mechanism is interrupted, more transmitters are released and the signal is transmitted more intensely. Mirtazapine is one of the newer alpha2-receptor blockers.
Be favorable side effect profile makes it a commonly prescribed ingredient.
unwanted effectsthat occur nevertheless are phenomena like severe tiredness, the Restless legs syndrome, Weight gain and Anemia.
A more serious complication of treatment with mirtazapine is the Agranulocytosis This means a strong to total decrease in the number of granulocytes (granulocytes are white blood cells) in the blood. Effects include fever and constant bacterial infections. Mirtazapine can be given in several forms.
In outpatient settings outside of the clinic, Mirtazapine is prescribed as a film or orodispersible tablet; in the clinic, it can also be used as an infusion verabe broken. In contrast to the SSRIs, mirtazapine already starts after about a week, the patients feel better quickly, which greatly increases the willingness to take the drug regularly.
Interactions with other active ingredients
SSRI and tramadol
Tramadol is a drug used to treat moderate to severe pain. It belongs to the group of opioids and requires a prescription, but does not fall under the Narcotics Act in Germany.
Serious interactions can occur if tramadol and SSRI are taken at the same time. The so-called serotonin syndrome can be triggered by an accumulation of the neurotransmitter serotonin. This is a life-threatening interaction of drugs that increase serotonin levels.
Symptoms include increased blood pressure and pulse rate, sweating, nausea, vomiting, diarrhea, headache, rapid breathing, and dilatation (widening) of the pupils. In addition, internal and physical restlessness can occur, as well as hallucinations, coordination disorders or disorders of consciousness.
In some cases, muscle twitching and seizures may occur. The occurrence of suicidal thoughts in connection with serotonin syndrome is also discussed.
To treat serotonin syndrome, all serotonergic drugs must be discontinued, and symptoms may also need to be treated with medication.
SSRIs and alcohol
Alcohol and SSRIs are generally a very unfavorable combination, as SSRIs can massively increase the effects of alcoholic beverages. Known effects of alcohol consumption such as dizziness, nausea, and insecurity of movement may then become so severe that it can lead to total loss of control or to unconsciousness.
In addition, alcohol should also be avoided in view of the side effects of SSRIs. Since the medication can cause an increased tendency to bleeding anyway and frequent alcohol consumption also has a negative effect on blood clotting, alcohol consumption and simultaneous use of SSRIs can lead to dangerous gastric or intestinal bleeding. This type of bleeding brings symptoms such as vomiting blood or bloody stools. Gastrointestinal bleeding is a potentially life-threatening emergency that requires immediate treatment.
Read more about this Antidepressants and alcohol - are they compatible?
SSRI and pill
The well-tried SSRI citalopram has no known interactions with oral contraceptives for contraception. Other SSRIs do not indicate that hormonal contraceptives are weakened, as they are usually metabolized by another enzyme in the liver.
In contrast to SSRIs, however, St. John's wort, which is used for mild to moderate depression, can weaken the effect of the pill. This is because St. John's wort affects the enzyme responsible for metabolizing contraceptives and can thus cause a loss of contraceptive effectiveness.
Patients receiving treatment for depression should discuss contraceptive therapy in detail with their gynecologist.
In our next article you will find more information about the interactions of the pill with other active substances: Which drugs affect the effect of the pill?
Issue SSRI
Abrupt withdrawal of SSRIs is general not recommendable. The body is used to fairly constant serotonin levels while taking SSRIs. If a patient suddenly stops taking the drug, falls also the Serotonin content very off quickly.
The reason for this is the short half-life of the drugs. Half-life is the time it takes until exactly half the initial dose of a drug is still in the body. SSRIs often have short half-lives, which means that they are broken down quickly. If the serotonin level falls in a short time, the body has no chance to compensate for the loss of messenger substance through increased production.
The consequences of stopping too quickly include fatigue, indigestion, muscle twitching or dizziness.
But the consequences for them are more serious mental state Of the patients. Since SSRIs are often prescribed to depressed patients, the condition of these patients often deteriorates suddenly.
Depressed people generally have low serotonin levels. If there is now a further decrease in serotonin because the SSRIs have been discontinued and the body could not adapt quickly enough and upregulate serotonin production, this can have far-reaching consequences.
There can be strong mood swings or an extreme deterioration in mood in general. The deeply depressed mood can lead to suicidal thoughts and in the worst case even result in suicide.
SSRIs should be used for this reason not arbitrarily, but only after consultation with the attending physician be dropped off; be discontinued; be deducted; be dismissed. A slow, continuous one is also recommended Reduction in dose, a so-called sneak out the medication.
The body then has time to get used to the decreasing amount of serotonin and to stimulate its own serotonin production.
What is withdrawal syndrome?
Withdrawal syndrome is the term used to describe the symptoms that occur when you stop taking SSRIs. This occurs especially when the drug is suddenly discontinued, especially after long-term therapy with SSRIs. To prevent withdrawal syndrome from occurring, the drug must be tapered for several weeks.
Withdrawal symptoms include indigestion such as diarrhea or constipation, physical discomfort, insomnia, sensory disturbances, dizziness, circulatory problems, sexual dysfunction, and tics. Mood swings, manias and depression can also occur, as well as suicidal thoughts.
SSRIs should therefore always be tapered prophylactically; benzodiazepines also help in acute therapy for withdrawal symptoms.
Alternatives to SSRI
Antidepressants can have serious side effects that require a switch. In addition to SSRIs, the class of antidepressants includes so-called tricyclic antidepressants. Active ingredients in this group include amitriptyline, imipramine, clomipramine and others. However, due to their numerous side effects, they are no longer the first choice in the therapy of depression.
Further alternatives are the selective norepinephrine reuptake inhibitors (SNRI, e.g. reboxetine). Dopamine reuptake inhibitors (DRI, amineptine) are no longer on the market these days.
On the other hand, serotonin norepinephrine reuptake inhibitors (SSNRIs, including venlafaxine and duloxetine) are important. Bupropion, an active ingredient from the class of selective norepinephrine / dopamine reuptake inhibitors, is also considered an alternative to SSRIs.
Another large group are the monoamine oxidase inhibitors, or MAOIs for short. Nonselective MAOIs such as tranylcypromine are important in the treatment of depression. Patients must be on a strict low-tyramine diet, as the consumption of some foods can lead to serious side effects.
Can be taken during pregnancy and breastfeeding?
Women who take SSRIs and are planning a pregnancy should definitely consult their gynecologist and doctor. There are various statements about the safety of SSRIs in pregnancy; compared to other antidepressants, SSRIs are considered to be relatively safe. The medication should only be discontinued in consultation with a specialist.
The breastfed child is exposed to the active substance SSRI through breast milk, but less than the alternative antidepressants. SSRIs are also generally considered to be relatively safe for breastfeeding mothers; here again, a decision should be made on a case-by-case basis. In cases of major depression, the benefit of treatment likely outweighs the drug's disadvantages for the mother and the breast-fed child. Because it has been tried and tested, citalopram is one of the SSRIs of choice for pregnancy and breastfeeding.
Which drugs can be taken during pregnancy or breastfeeding and which should be avoided? Read more about this under:
- Medication during pregnancy
- Medication during breastfeeding