Causes of Low Blood Pressure
introduction
Low blood pressure (hypotension) means blood pressure below 105/60 mmHg. The normal value for blood pressure is 120/80 mmHg.
Low blood pressure can manifest itself for a variety of reasons. Too low blood pressure (hypotension) can be associated with certain symptoms (e.g. dizziness with circulatory collapse (syncope), visual disturbances, headaches, etc.). It is therefore important for the attending physician to track down the underlying cause in order to be able to raise the blood pressure adequately.

Causes of Hypotension
The causes of low blood pressure can basically be divided into four different categories:
- organic causes (e.g. in diseases of the heart or the vascular system, thyroid or adrenal gland) or due to certain environmental conditions (e.g. stress or underweight)
- congenital constitutional form of low blood pressure (hypotension)
- Shock situations (e.g. allergic or septic shock)
- orthostatic adjustment disorder after changing from lying to standing position
Hypotension is very common in adolescent thin female people. Physical or emotional stress in private or at work can also be the cause of low blood pressure. It is not uncommon for low blood pressure to be temporarily caused by insufficient fluid intake or electrolyte imbalance. Since hypotension can have very different causes, a comprehensive diagnosis should be carried out (examination of the vascular system, imaging of the thyroid gland, drawing of venous blood to determine the electrolytes, etc.). Certain questions should be dealt with in the anamnesis, based on which a possible finding of the cause becomes more likely.
Heart and vascular diseases as a cause of hypotension
Heart diseases such as arrhythmias or heart failure can impair the functioning of the heart and lead to low blood pressure.
Arrhythmias can lead to decreased blood output from the heart and thus to low blood pressure. This reduced sputum output (cardiac output) occurs primarily in the case of circulating excitations in the heart (e.g. reentry tachycardia) or in situations in which the heart is functionally stationary (e.g. ventricular fibrillation). Less blood volume reaches the central and peripheral arterial vessels per time. Since a continuous supply of oxygen to the sensitive neurons of the brain is essential and this can no longer be guaranteed in such a case, typical symptoms such as dizziness, syncope, pallor, etc. can occur.
Even with a weak heart muscle (heart failure), the heart ejects less blood from the main artery (aorta) and the pulmonary trunk. Clinically, this expresses itself identically with a reduced blood output as in certain cardiac arrhythmias.
A so-called aortic arch syndrome can also lead to low blood pressure. Here, there is a narrowing (stenosis) directly in front of the outlet of the arterial vessels (common carotid artery) that supply the brain. In the aortic arch syndrome, the lower extremities are typically still supplied with sufficient blood, while the brain is arterially undersupplied. This leads to typical symptoms of arterial hypotension.
Vein weakness in the context of hypotension
Vascular diseases such as a weak vein wall can lead to hypotension. Due to a disturbance of the muscular or the connective tissue part it can lead to widening of the veins ("varices"). The blood sinks into this and turbulence forms due to the slowed blood flow. The blood literally "stops" and sinks. Varices usually occur in the legs, where the blood consequently sinks. This leads to low blood pressure in the central circulation. An undersupply of the arterial vessels of the brain with a possible circulatory collapse can result.
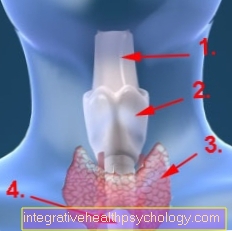
Thyroid and adrenal disorders as causes of hypotension
Along with the adrenal gland, the thyroid is one of the organs that is involved in regulating blood pressure through the release of its hormones.
The two hormones triiodothyronine (T3) and thyroxine (T4), which are formed by the thyroid gland and released into the blood, are of great importance here. These hormones act on different cells and tissues and can influence blood pressure, among other things. You can increase the work of the heart (among other things through an increased activity of the sodium / potassium ATPase) and thus also the blood pressure.
In the case of an underactive thyroid (hypothyroidism), there is a deficiency in these hormones. As a result, hypothyroidism can lead to low blood pressure (hypotension). An autoimmune disease (Hashimoto's thyroiditis, primarily in young women) is very often the cause of an underactive thyroid. Therefore, especially in young women with symptoms of low blood pressure (dizziness, listlessness, tiredness, paleness, visual disturbance with star vision), a thyroid-related genesis should be considered.
Addison's disease
In addition to sex hormones (androgens), mineralocorticoids (especially aldosterone) and glucocorticoids (especially cortisol) are also formed in the adrenal cortex.
Aldosterone and cortisol in particular lead to an increase in arterial blood pressure. In diseases with an underactive function (for example Addison's disease or tumor diseases), hypotension can result.
In Addison's disease, the adrenal cortex is underactive. As described above, blood pressure-increasing hormones such as aldosterone and cortisol are formed here. In the case of hypofunction, these blood pressure-increasing hormone effects do not apply. This can lead to low blood pressure (hypotension).
Do you have any further questions about an underactive thyroid? Read more about this at: Hypothyroidism
Stress as a cause of hypotension
At first, the occurrence of low blood pressure in stressful situations appears to be paradoxical. Normally, stressful situations constrict the arterial vessels (vasoconstriction) in order to increase blood pressure and to meet the increased demands on physical activity.
However, this control loop fails when long periods of stress occur. The vasoconstriction (vasoconstriction) can no longer be maintained and low blood pressure (hypotension) can set in. Therefore, care should be taken to transform the so-called "negative" stress into a "positive" stress. All in all, periods of stress should be limited in time in order to avoid this dysregulation of the vasoconstriction.
Are you suffering from stress? Read more about the signs of stress on the following page: Symptoms of stress
Adolescent age and female gender as causes of hypotension
Young age can in principle also lead to low blood pressure (hypotension). Mostly this is because younger people are very thin in some cases. Especially in adolescence, the body faces the challenge of growing quickly. The young people are very thin (often also due to "social pressure situations"). The blood pressure is usually lower than in adults.
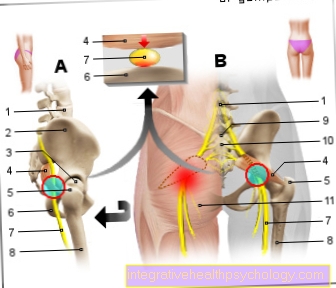
Up to around 20% of all children up to the age of 15 suffer one or more collapses due to poor circulation. In most cases, this is due to orthostatic dysregulation.
The so-called vasovagal syncope is also very common. This leads to a pathological drop in blood pressure and sinking of the blood in the lower extremities after standing up. In this case, the brain is temporarily undersupplied with blood and a circulatory collapse can develop.
The processes of growing up described above with strong body growth combined with often very low blood pressure occur more frequently in women. In this "phase of life", low blood pressure (hypotension) can often be triggered by insufficient fluid intake. The body needs an increased absorption of minerals and nutrients for growth.
Dehydration as a cause of hypotension
A potentially reversible cause of low blood pressure (hypotension) that can be prevented by simple measures is insufficient fluid intake.
Since around 1.5 to 1.8 liters per day is lost through the urine (additional fluid, for example through breathing or sweating), the circulating blood volume in the vascular system must be maintained through sufficient fluid intake.
The average recommended amount of fluid intake of between 2 to 3 liters can be increased significantly through additional exercise (e.g. sport).
Basically, the blood pressure in the vascular system is regulated by the mutual interplay of hydrostatic pressure (the pressure that the blood in the vessel exerts on the vessel wall and potentially wants to push fluid out of the vascular system) and colloid osmotic pressure (proteins of the blood plasma that hold the fluid in the vascular system) .
An imbalance between these two pressures can lead to a change in blood volume and thus blood pressure. For example, a lack of plasma proteins (especially albumin) leads to a loss of water in the vascular system and thus to a drop in blood pressure.
In addition, an increased loss of fluid (for example as a result of injuries with bleeding) can lead to low blood pressure due to fluid loss. Frequent vomiting (vomiting), diarrhea or increased urination in diabetes mellitus also cause increased fluid loss.
Drugs as a cause of hypotension
A sharp drop in blood pressure (hypotension) can in principle also be due to the side effects of medication.
For example, diuretic drugs such as diuretics (for example the frequently used loop diuretic) have a strong blood pressure lowering effect. During therapy with diuretics, therefore, in addition to regular electrolyte control (especially potassium), blood pressure should also be measured.
In general, antihypertensive drugs can also cause hypotension. Particularly in the early phase of antihypertensive therapy, severe hypotension can occur. Check measurements of the blood pressure should be carried out here regularly.
Some psychotropic drugs also have an antihypertensive effect. Particularly noteworthy are tricyclic and tetracyclic antidepressants and certain antipsychotics from the group of phenothiazines.
Genetic predisposition as a cause of hypotension
Constitutional disorders of the target value for blood pressure in the regulating organs can also be considered as a cause.
These are mainly the stretch receptors (baroreceptors) in the carotid sinus of the aorta, the medulla oblongata as the circulatory center in the brain stem and the kidney as the regulator of volume with the central hormone renin. Blood pressure regulation is a complex unit made up of several organic systems, which can be thrown out of balance by innate effects. A genetic setpoint adjustment for the “optimal” blood pressure is basically possible in both directions. In addition to hypotonia, hypertension can also occur due to the patient's condition.














.jpg)





.jpg)