Myelopathy
definition
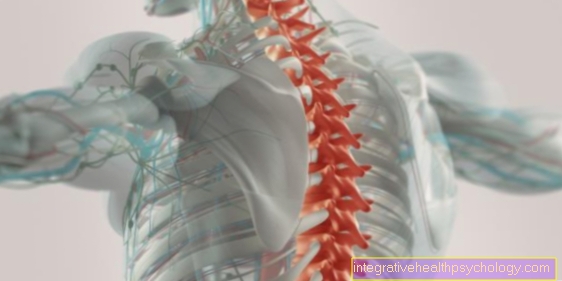
A myelopathy is one Damage to nerve cells of the spinal cord. The medical term is formed from the two ancient Greek words myelon - marrow and pathos - suffering. Depending on the cause of the spinal cord damage, a distinction is made between different forms. The location of the damage to the spinal cord is decisive for the symptoms; whether the spinal cord of the cervical, thoracic or lumbar spine is affected. The damaged section of the spinal cord can no longer perform its normal function and it comes to neurological failures like paralysis or sensory disorders. The diagnosis is made using imaging techniques (such as MRI). Therapy depends on the cause of the myelopathy.

Symptoms
The symptoms of myelopathy can be great diverse be and depend primarily on the region the spinal cord damage. The cause of the myelopathy can also influence the clinical symptoms.
It applies to all forms of myelopathy that the damaged spinal cord sections can no longer perform their function correctly in the nervous system, so that it becomes too neurological failure symptoms comes. On the one hand, these are Sensory disturbances such as tingling pain or numbness. On the other hand, patients complain about disorders of the musculoskeletal system such as Muscle weakness up to paralysis of the muscles. This can affect both the arm and leg muscles. This can lead to gait disorders. In addition to mobility disorders can also Problems with emptying the bowel or bladder (Bladder and rectum disorder) occur. In the case of herniated discs, there is also traditionally severe pain in the affected section of the spine, which can radiate into the arms and / or legs on both sides.
causes
Damage to the spinal cord can be caused by a variety of mechanisms.
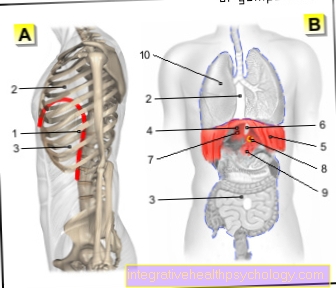
In the Compression myelopathy the pressure on the tissue causes damage to the spinal cord. This pressure can be due to, among other things Tumors such as metastases from spinal or meningeal tumors. Are not uncommon Herniated discs the cause. As the inner core of the intervertebral disc slips into the spinal canal, pressure is exerted on the spinal cord inside. A narrowing of the spinal canal like a Spinal stenosis can also cause compression myelopathy. A rarer cause is that Osteosclerosiswhere there is a narrowing of the spinal canal due to excessive formation of bone tissue.
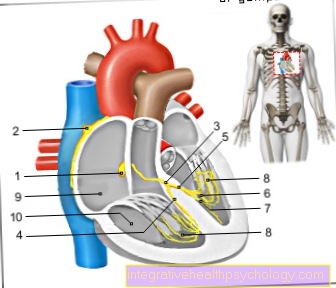
In addition to compression myelopathy, there is also one decreased blood flow damage to the nerve cells in the spinal cord. Circulatory disorders occur with vascular malformations or vascular constrictions (Stenoses). Even with one acute blood loss a shock can lead to an undersupply of the spinal cord. These forms of myelopathy caused by circulatory disorders are also called vascular myelopathy.
The third group is the Radiation myelopathywhich can cause damage to the spinal cord during radiation therapy.
It can go a long way Vertebral fracture cause an injury to the spinal cord.
Spinal stenosis
The spinal canal is a canal formed by the vertebral arches at the back of the spine; the spinal cord runs in it. The stenosis is therefore the narrowing of this canal. This can be caused, for example, by the new bone formation that occurs with increasing age as part of degenerative changes, whereby these osteophytic additions reach into the spinal canal and displace the nerve fibers of the spinal cord.
A typical symptom of spinal stenosis is that after a short distance you have to restrict walking due to pain. Whereas no complaints are given for cycling. This is based on the bent forward posture, which relieves the spinal cord.
Magnetic resonance imaging is performed to establish the diagnosis. Surgical therapy to remove excess bone in the spinal canal so that the spinal cord has more space.
If you are further interested in the topic, then read: Spinal stenosis
diagnosis
The anamnesis already provides indications of an existing myelopathy. It is important to inquire about specific symptoms such as paralysis, sensitivity disorders or pain in the spine. The clinical examination brings further security, as, for example, the reflexes can be conspicuous and the gait pattern is changed.
To confirm the diagnosis, magnetic resonance tomography is used as diagnostic imaging. A spinal angiography is useful for special questions, such as suspicion of vascular myelopathy. Myelography may also be indicated. In this procedure, contrast agent is injected into the spinal canal under X-ray imaging in order to show the spatial conditions of the spinal cord and the emerging nerves.
If you are interested in further diagnostic imaging procedures, please read: MRI of the spine and Myelography
MRI
Magnetic resonance tomography is the most important examination method to determine myelopathy. On the one hand, structures that compress the spinal cord, such as a herniated disc or tumors, can be seen using MRI. Vascular changes can also be shown.
On the other hand, damaged spinal cord regions can be distinguished from healthy nerve tissue in the MRI image. If you have questions about the bony structures, computed tomography can be useful as a supplement in individual cases.
What is a myelopathy signal?
The term myelopathy signal comes from diagnostic imaging. It is mainly used by radiologists to describe magnetic resonance (MRT) examinations. One speaks of a myelopathy signal if there is an indication of damage to the spinal cord (myelon) in the imaging. This can be the case, for example, with edema (accumulation of fluid) or a tumor in the spinal cord. A myelopathy signal is non-specific, i.e. it occurs regardless of the cause of the spinal cord damage.
The spinal cord damage can therefore only be temporary. The patient does not always have severe symptoms. Therefore, in addition to a myelopathy signal, its cause and the patient's complaints are decisive for the therapy. The spinal cord cannot be assessed very well in a conventional X-ray. Even in a CT examination, damage to the spinal cord cannot be ruled out with absolute certainty. Therefore, the MRI examination is the method of choice for diagnosing myelopathy.
Further information is also available at: MRI of the spine
Treatment of myelopathy

Depending on the cause of the myelopathy, a distinction is made between various therapy options.
First of all there is the possibility of conservative therapywhich is symptom-oriented. If there is pain, the patient receives Painkiller, whereby the so-called NSAIDs (non-steroidal anti-inflammatory drugs such as ibuprofen, diclofenac) are particularly suitable, as these also have anti-inflammatory and decongestant effects. A muscle-relaxing drug often also relieves the symptoms. In addition there is one physiotherapy treatment for use.
The real one root cause the myelopathy must mostly operational treated so that, for example, in compression myelopathy, the pressure on the spinal cord is removed.
As a general rule, the prognosis of the disease is best if the diagnosis is made early and adequate therapy is initiated. The faster the damage to the affected nerve cells is counteracted, the higher the probability that the corresponding spinal cord section is again regenerate can.
Operational approach
During a surgical intervention on the spine, one tries to relieve the pressure-damaged spinal cord. Various surgical techniques are used here, with a distinction being made between front and rear access. For example, in the area of the cervical spine, access from the front is now more often chosen, with the patient lying supine on the operating table during the operation.
Before the skin incision is made, the position of the vertebra to be operated on is checked using a mobile X-ray device. In order to reach the affected area, the structures on the front of the neck such as muscles, thyroid gland or large blood vessels are pushed aside. You can now remove excess tissue in the area of the spinal canal using special instruments. If the intervertebral disc cannot be preserved, a ceramic or titanium spacer is used. If you fill this placeholder with bone substance, you can connect the two adjoining vertebral bodies with one another and thus achieve good stability.
The procedure is always carried out as an inpatient and under general anesthesia. Depending on the complexity, it takes between one and several hours. Rehabilitation treatment should follow after the inpatient stay in hospital. It takes up to 4 months until the spine is fully resilient again after the operation.
course
The course of a myelopathy can be very different depending on the cause. A basic distinction is made between an acute and a progressive form.
Acute means something that occurs quickly or suddenly sudden development of symptoms manifested. The cause can be, for example Hemorrhage be in the spinal canal after trauma. Furthermore, the Interruption of blood supply lead to acute myelopathy through a heart attack. Sometimes herniated discs also express themselves in the acute form.
Since myelopathy in a disc prolapse but usually progresses slowly, one then speaks of a progressive course. This is also with Tumors the case, which usually grow into the spinal canal over time and slowly displace the spinal cord. This only leads gradually to increasing neurological deficits. Also degenerative changes on the bones that grow into the vertebral canal only lead to symptoms in the course of the disease. This often insidious development of symptoms is what makes the disease so insidious. An early diagnosis and therapy are of decisive importance for the success of healing.
Special features of the different locations
Cervical spine
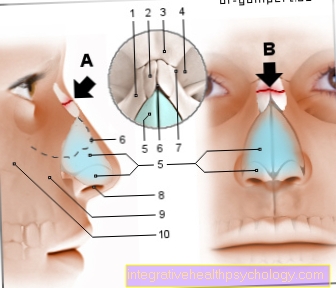
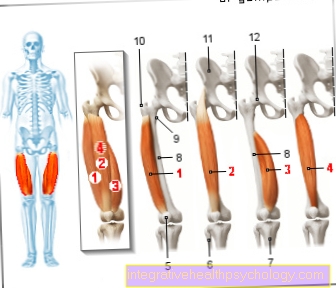
The myelopathy of the cervical spine is known in technical terms as cervical myelopathy. It is the most common form of myelopathy and is often insidious. The cause is usually compression. The spinal cord is damaged by a herniated disc in the neck area. New bone formation also occurs with degenerative joint changes (osteophytic additions). Since the space in the spinal canal is limited, the nerve cell bundles in the spinal cord are also displaced. Symptoms can be both sensory disorders and motor disorders, with arms and legs being affected.
During the clinical examination, the patient complains of abnormal sensations in the arms when the head is passively bent forward. In this case one speaks of a positive Lhermitte sign. Early neurosurgical intervention is the therapy of choice. The faster the diagnosis is made and the patient is given the right therapy, the better the course. In the case of an acute herniated disc, the chances are not bad that the symptoms will at least largely regress.
If you have any further interest in this topic, check out our next article at: Cervical myelopathy
Thoracic spine
The myelopathy in the area of the thoracic spine is in the technical language as thoracic myelopathy designated. The symptoms and the course are similar to those of the cervical spine. The symptoms usually appear gradually. Sensitivity disorders and muscle weakness in the arms and legs occur. This often leads to a Impairment of the gait pattern. Disturbances in emptying the bladder and bowel are also common. If the disease cannot be stopped in its course, it exists dangerthat is a Paraplegic syndrome developed.
The disease is treated depending on the cause. In the case of herniated discs or tumors, surgery is often essential. Overall, however, is thoracic myelopathy significantly less often than the cervical form.
Further information on the subject can be found at:
- Spinal cord
- Spinal stenosis
- disc prolapse
- Nerve pain
- Nerve damage
- Degenerative spinal diseases












.jpg)