Post-operative pain therapy
General
Post-op pain is an all-too-natural response in the human body. During an operation, anesthesia ensures that the patient survives the operation painlessly. Now, however, the time after the operation, the time of healing and recovery, should be as pain-free as possible so that the patient can recover from the stresses both physically and mentally. Modern post-operative pain therapies make this possible. Freedom from pain is essential for a perfect and good recovery. The pain-free patient is easier to mobilize and easier to participate in his own healing.

aims
The aim of post- and perioperative pain therapy is to limit the pain after the operation to a tolerable minimum or even to prevent it completely. This should also prevent possible functional restrictions that can result in post-traumatic pain. This also includes stress and chronification. The side effects of postoperative pain therapy should also be kept to a minimum, which must be reasonable. Furthermore, specific characteristics of individual patient groups must be taken into account and the individual course of recovery must be supported.
Read more on the topic: Chronic pain syndrome
Procedure and aspects of postoperative pain therapy
Strictly speaking, postoperative pain therapy begins before the operation, with the choice of the surgical procedure. So-called minimally invasive procedures often cause less pain and complications than conventional surgical techniques.
The positioning of the patient is also important. Careful posture on the operating table, for example, prevents back or neck pain later on. On the other hand, an unfavorable position can provoke unnecessary pain. Painkillers are also administered before the operation, which then allow the patient to be largely pain-free for the first time after the operation.
Choice of anesthesia
The choice of the anesthetic type is also important for the recovery process after the operation. Regional anesthesia is used for minor surgical procedures. The local anesthetic is initially administered close to the nerve once. There is then the possibility of inserting a catheter through which the local anesthetic can be applied post-operatively either continuously using a pump or once to combat pain. The epidural catheter can be cited as an example here. Local anesthetics are local anesthetics which, in addition to providing pain relief, also ensure better blood circulation and thus better wound healing. They are also very well tolerated. Side effects are rare and rather harmless.
Read more on the topic: General anesthesia or conduction anesthesia
Medicinal pain therapy
Very severe post-operative pain is treated with opiates. Opiates are centrally acting pain relievers because they act on the central nervous system. They can be administered both orally and intravenously. In postoperative pain therapy, the intravenous method is preferred.
The disadvantage of opiates is sometimes very unpleasant and strong side effects such as nausea, tiredness, itching and indolence. The side effects are accepted because of the effectiveness.
In addition to the centrally acting analgesics, there are also peripheral analgesics. These include, for example, diclofenac, metamizole and paracetamol, which many people also know from everyday use. These are also used in postoperative pain therapy.
WHO level scheme
The WHO recommends a graduated scheme for drug pain therapy. This tiered scheme is originally derived from a scheme for tumor therapy. The scheme includes three stages of drug treatment. The fourth stage includes invasive pain relief measures.
If pain is insufficiently eliminated in one level, it is escalated to the next level according to the scheme. In addition, needs-based physiotherapeutic methods and co-analgesics in the sense of anticonvulsants, antiemetics, antidepressants, glucocorticoids and other groups of active substances are used at each stage.
The non-opioid analgesics include, on the one hand, non-steroidal anti-inflammatory drugs (NSAIDs) such as ASA, ibuprofen and COX2 inhibitors and, on the other hand, paracetamol, as well as metamizole and their group-related substances. Weak opiates include tramadol, tilidine, and dihydrocodeine, possibly in combination with naloxone. Examples of highly potent opioids are morphine, oxycodone and fentanyl.
- Level 1: In level 1, initially only non-opioid analgesics are used (in combination with adjuvants (increases the effect of the drug) e.g. metamizole, paracetamol, NSAID
- Level 2: Level 2 provides for the use of low-potency opioid analgesics in combination with non-opioid analgesics and / or adjuvant, e.g. Tilidine, Tramadol (+ level 1)
- Step 3: Finally, in step 3, highly potent opioids are combined with non-opiods and / or adjuvant e.g. Morphine, oxycodone, fentanyl, methadone, hydromorphone (+ level 1)
- Stage 4: treatment using invasive techniques? peridural and spinal injection, spinal cord stimulation, ganglion blockade and peripheral local anesthesia
Supportive decongestant therapy, e.g. with Wobenzym have a positive effect on pain perception.
PCA - A special form of post-operative pain therapy
PCA stands for "Patient-controlled analgesia". This form of therapy has been known about since the 1970s. In general, it is any type of pain therapy that allows the patient to determine when to receive a dose of pain medication. So he determines the time intervals himself. The total dose, the maximum of a single dose and the type of drug are of course determined by doctors.
As a rule, in postoperative pain therapy, an opiate is administered intravenously through a so-called pain pump. The patient can then trigger the injection by pressing a button, for example. The advantage here is that the patient can decide on his pain relief within a certain secure framework independently of doctors and nursing staff.
However, there are of course disadvantages. Patients with physical or mental disabilities may not be able to activate the button. There is also a risk of medication abuse or overdosing or underdosing the medication if the pain pump is not programmed correctly.
What do the guidelines say?
The current "S3 guideline on" Treatment of acute perioperative and postoperative pain "from 2009 was drawn up with regard to the still inadequate care of postoperative pain. It includes numerous studies and meta-studies from previous years and is divided into a general and a special part.
The first deals with aspects such as patient education, pain measurement and documentation, as well as organizational aspects. In the special part of the guideline, the individual procedures of pain therapy and special aspects in the individual surgical areas are discussed.
The focus is not only on systemic pain therapy with non-opiod analgesics and strong and weak opiods. Rather, the value of non-drug procedures is also recorded. Psychotherapeutic and physiotherapeutic methods, but also physical methods (e.g. cold therapy) and “transcutaneous electrical nerve stimulation” (TENS) play an important role. A benefit of acupuncture for acute pain therapy postoperatively, in contrast to the treatment of chronic pain, has not yet been proven. Finally, regional anesthetic procedures in the sense of spinal cord and peripheral regional anesthesia are also discussed.
Read more about:
- Electrical stimulation
- Cryotherapy
- Epidural anesthesia
Preoperative patient training
It is considered useful to provide patients with adequate information about postoperative events prior to surgery. In this way, the patient can deal primarily with the impending pain progression and recovery and actively contribute to the healing process. He is comprehensively trained in the somatic (physical) and psychological possibilities for pain relief and instructed in how to use them.
Placebo effect
Another important aspect of postoperative pain management is the use of the placebo effect. The placebo effect is any positive physical and psychological change that cannot be traced back to an effective treatment, such as a drug, but to a psychological context.
This means that a patient experiences an improvement in their pain without taking an effective medication, for example. This is achieved, for example, by having a patient take a dummy drug knowing that it contains an effective pain reliever. This awareness alone can alleviate the pain.
The placebo effect is only used in addition to active pain therapy. It can optimize the effect of the pain reliever drug, but it cannot replace it.
The opposite of the placebo effect is the nocebo effect. The nocebo effect is all negative physical and psychological reactions that are not directly attributable to the treatment or its side effects. This effect should be avoided in postoperative pain therapy.
Psychological measures of postoperative pain therapy
Pain can be relieved not only by analgesic drugs, but also by psychological procedures and methods. These are increasingly used in modern postoperative pain therapy. This includes behavioral therapy procedures such as distraction strategies or cognitive reassessment.
Other psychological procedures that have an analgesic effect are also used. These include, for example, hypnosis, relaxation exercises and the imagination. The psychological intervention should sometimes begin before the operation. It makes sense to train patients with chronic pain and / or mental illness in dealing with pain before an operation and to give them psychological pretreatment in order to achieve a milder postoperative pain progression.
Read more on the topic:
- Pain memory
- Progressive muscle relaxation
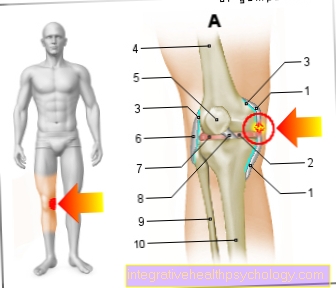
postoperative pain therapy in orthopedics
Orthopedic procedures are often associated with severe pre-existing pain. This is particularly relevant because pre-existing pain is an important risk factor for the development of chronic pain. Adequate peri- and postoperative pain therapy is therefore all the more important here.
Gabapentin can also be administered preoperatively, especially for spinal surgery, while a glucocorticoid can be administered locally intraoperatively for radicular pain.
In the case of interventions on the extremities, local regional procedures are to be preferred over systemic forms of pain therapy. The often easily accessible location of the various nerve plexuses and the general advantages of regional anesthesia often make this possible for peripheral interventions. Should a regional anesthetic procedure still not be feasible, treatment with strong opioids according to level 3 of the WHO level scheme is recommended.
Read more on the topic:
- Brachial plexus anesthesia
- What is a foot block?
- What is a finger pad?
postoperative pain management in children
Contrary to the strongly outdated opinion, newborns cannot yet feel pain, we now know that children perceive pain from the 24th week of pregnancy. From this point onwards, pain in children should be treated.
Postoperative pain therapy in children is essentially based on the same principles and principles as pain therapy in adult patients. Differences can be found especially in the first 12 months of life with regard to the changed distribution, conversion, degradation and excretion (Pharmacokinetics) many drugs. This is especially true for the first few weeks of life.
Many drugs are also not approved in the first months or years of life. However, this should not lead to analgesics being withheld from young patients if they are needed - despite the lack of approval!
Paracetamol is nevertheless the most important analgesic in childhood and is approved for every age group. Ibuprofen is approved from the 3rd month of life. In addition to systemic drug pain therapy, regional pain methods and non-drug treatment concepts should not be neglected in children either.
Read more on the topic: Medicines for children and toddlers - what medicines should I have at home?