Thrombosis in the leg
Synonyms
Thrombus, blood clot, blood clot
definition
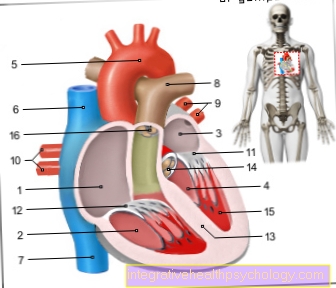
As thrombosis is called a Blood clots, the in the venous system The body creates a blood vessel closes and prevents venous blood outflow at the affected area of the body. Thrombosis occur often in the deep leg and pelvic veins, less often in arm veins.

introduction
Thrombi that develop in the venous vasculature more often affect older people over 60 years of age who are bedridden or immobile due to other diseases. But young people, especially young women, who take oral contraceptives also belong to the risk group for thrombotic diseases.
Read more on the topic: Thrombosis risk of the pill
In addition to pelvic vein thrombosis, thrombosis in deep leg veins is the most common type.
Thrombosis is a medical emergency and requires immediate medical attention to prevent complications such as pulmonary embolism.
Read more on the topic: Pulmonary Embolism What are the Symptoms?
Symptoms
Symptomatically, a thrombosis in the leg is the first to fail strong pain on. Patients characterize this pain as Tension pains, drawing pains and occasionally as Heaviness. At Elevation the affected limb the pain decreases noticeably. Compared to the other leg, the one affected by the thrombosis swollen, strong overheated and has a tight, shiny red to bluish skin. It comes to pressure sensitivity and Movement pain, especially when flexing the soles of the feet. Rare symptoms like fever or an increase in heart rate occurs only in a fraction of the cases.
Read more on the topic: Detect thrombosis
Swelling in the leg
Only 10% of the patients who develop an acute vein thrombosis notice it by the typical symptoms swelling, pain and Blue color. The swelling occurs because blood continues to be supplied to the blocked vessel, but it cannot be passed on.
The aqueous components of the blood then pass from the blood vessel into the surrounding tissue and enter edema creates a watery swelling. The more pronounced the swelling, the more dangerous it becomes. The swelling can progress until it pinches arterial vessels.
causes
Thromboses in the leg are primarily caused by three factors, they are summarized under the name Virchow's triad. These include changes in the inner walls of blood vessels, changes in blood flow and disorders in the composition of the blood.
Vascular walls change in connection with injuries, when scarring and inflammation caused by viruses or bacteria. If the flow behavior of the blood changes, vortices are created. This often happens, for example, as part of a varicose vein disease (Varices) or by slowing the blood flow if the heart is weak.
Read more on the topic: Varicose vein disease
This leads to the formation of small clots, as the individual components of the blood have the opportunity, due to the inadequate flow, to accumulate in "piles" (clots), making the blood flow more difficult and finally closing the vessel completely.
The third main cause of thrombosis, the altered composition of the blood, is caused by an imbalance in blood clotting and the dissolution of blood clots. Normally, the two components are balanced in order to enable a regulated blood flow in intact vessels and, at the same time, rapid blood clotting in the event of vascular injuries. In the context of various diseases, this balance can get out of hand. Particularly noteworthy here is the thrombophilia, a genetically determined tendency to form a particularly large number of blood clots with a high risk potential for heart and circulatory diseases.
In addition to the three main causes, there is a broad spectrum of risk factors that enormously promote the development of thrombosis. Smoking, obesity, insufficient exercise, but also varicose veins and the use of water tablets (diuretics) are among those risk factors.
Read more on the topic Thrombosis causes
These causes can also lead to a pelvic vein thrombosis. This is problematic because of its symptom-free course, which is why it can be discovered too late. Also read the following article in this context: Pelvic vein thrombosis
Risk factors
In addition to risk factors such as obesity, lack of exercise, smoking and taking the pill, there are also various rare ones inheritable Diseases that increase the risk of thrombosis. These occur around 0.1% -5% in the population. They increase the risk of developing a thrombosis by a factor of 3-8 compared to healthy people.
The pill
The combination drug from is the riskiest of all the vehement pills estrogen and Progestinbecause of the substance Drospirenone is buried. Studies have shown that it carries the greatest risk of thrombosis. It is statistically interesting that only 3-6 out of 10,000 women are affected.
Smoke increases the risk of thrombosis as well as Obesity and high blood pressure. It may happen that overweight, smoking patients are not prescribed this form of contraception. An alternative to this are other hormone preparations that contain different or fewer progestogens (e.g. micro- or mini-pill).
To fly
Frequent flyers that long flights graduate belong to a special risk group for thrombosis in the legs. By sitting for hours in the plane, the low air pressure and the low humidity Blood flows more slowly in the cabin of an airplane. In addition, when you sit for a long time, the veins in the hollow of the knee kink which slows the blood flow again and encourages thrombosis.
It is advisable if you feel pain in your legs while flying or if you have other symptoms such as swollen legs on the next flight over Support stockings ponder. There is also the option of seeking advice from a doctor before traveling by air, who can prescribe anticoagulant medication if necessary. What you can do yourself is drink enough to maintain his fluid balance and every now and then getting up during the flight and walking up and down the aisle. The activity of the muscles compresses the veins and thrombi have less chance of attaching themselves to the vessel walls.
diagnosis
A detailed one Doctor patient conversation (anamnese) forms the first part of the investigation. Particular questions must be asked about risk factors such as smoking, alcohol consumption, obesity or varicose veins. Furthermore, by means of Ultrasonic the diagnosis can be confirmed. In ultrasound images, the doctor recognizes thrombosis in the leg with theCompression test". If there is a thrombosis, the blocked vein can no longer be compressed at the point where the thrombus is located. It is therefore quite easy for doctors to reliably diagnose thrombosis and initiate appropriate therapy.
D dimers
The increase in the so-called D-dimers and the inflammation parameters can be determined with the blood sample. The inflammation parameters that are of interest here are the increased number of white blood cells and the rate of sedimentation of the blood when it is in a glass. The faster the solid blood components separate from the liquid and settle, the more likely a pathological process is in the body.
A low or negative D-dimer value always excludes the presence of a thrombosis. A high or positive D-Dimer value can raise a suspicion of a thrombosis, but it does not always have to be a thrombosis.
To be absolutely sure, if the D-Dimer value is suspicious, an ultrasound should be performed to confirm the diagnosis.
Read more on this topic at: D dimers
therapy
Thrombosis in the leg indicates a dissolution of blood clots no longer working properly down. Therapeutically, therefore, substances are generally used that restart this mechanism.
Heparin is that Means of choice, it prevents further thrombosis from forming. Recanalization can also be performed to dissolve the thrombosis in the leg. The vein expanded by means of a catheter, so that a regulated blood flow is possible again.
In the drug-based resolution (Lysis) come substances like that Streptokinase, which is obtained from bacteria and is able to dissolve blood clots, is used. In addition, the swelling of the leg through a Compression therapy treated. With elastic bandages in the initial stage and compression stockings after the acute phase, the venous blood flow is promoted and the clot is prevented from detaching.
What to do if there is a thrombosis in the leg
If there is a suspicion of a thrombosis in the leg, a few points should definitely be observed. The sore leg is to move as little as possible, elevate can improve the pain, is also recommended for pressure relief. However, you can use the leg not on hard surfaces Storage, pillows or rolled up blankets can help.
There are thromboses in the leg medical emergencies and require treatment in hospital. Nevertheless, it is important to stay calm and not panic. Either you let yourself be driven to an emergency room or alert you Ambulance service. You shouldn't even drive a car, as the thrombus can loosen and travel with the bloodstream to the heart.
Duration
How long the symptoms of thrombosis last depends on many different factors. A very small thrombosis can be controlled by the mentioned conservative measures. The larger the thrombus, the more severe the symptoms and the more complex the subsequent therapy, the longer the patient is affected. There are also thromboses, which are operated on in special clinics by doctors with a specialization (Trendelenburg operation). These patients usually need a lifetime Anticoagulants take and / or Compression stockings wear.
Read more on the topic: Compression stockings
As a rule, the therapy is carried out with compression stockings or bandages for at least 3 months. How quickly the patient improves also depends on how healthy or sick they are overall. It is clear that an early movement (called mobilization), adapted to his symptoms, has a positive effect on the course.
If a patient with thrombosis has surgery as the last treatment option, it will result in a longer period in hospital. A distinction is made between a smaller and a larger surgical option. A probe (Catheter) inserted into the corresponding vessel up to the clot under X-ray control. There, the thrombus can be cut into small pieces, so to speak, or it is triggered by a drug that is given through the probe.
The other option that is reluctant to choose is the larger one, which involves cutting open the leg along the vessel and removing the blocked vessel (Thrombectomy). This is the operation that is mainly performed by specialists.
Consequences of a thrombosis in the leg
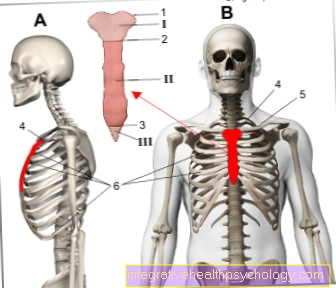
Most feared among the consequences of a thrombosis in the leg is by far that Pulmonary embolism. It occurs when the thrombus loses its adhesion to the vessel wall and with the blood circulation in the lung is transported and there a artery locks.
It happens when that Leg moves becomes, for example when getting up. Kick in the course of a pulmonary embolism Breathing disorders, Chest pain, Racing heart and in the worst case one shock that usually ends fatally. Many patients die from pulmonary embolism. In the case of sudden onset of chest pain and breathing difficulties after or during a thrombosis in the leg, the Emergency call to get voted.
A another complication a thrombosis in the leg consists of recurrence of thrombosis (Thrombosis recurrence). Blood-thinning medication can help.
How dangerous is a thrombosis in the leg?
A thrombosis always requires a visit to the doctor. Even the smallest clots can be dissolved by the body's natural coagulation dissolving system and never cause discomfort. In this case, the person concerned does not notice the thrombosis.
But it is also a fact that a clot gives more platelets a chance to clump together and can get bigger. It can also "migrate", that is, it can get to another part of the body and damage organs there.
Since pulmonary embolism or severe swelling that can kill the leg can develop from deep vein thrombosis, leg vein thrombosis must be classified as dangerous. The earlier you go to the doctor with complaints, the better!
forecast
The prognosis of a thrombosis in the leg is better, the earlier the disease was recognized and treated. The longer the thrombosis in the leg remains untreated, the greater the risk of developing the so-called post-thrombotic symptom. This results in chronic weakness of the veins, which means that varicose veins develop more frequently.
With each varicose vein, however, the risk of developing a new thrombosis (thrombosis recurrence) increases. The longer you postpone treatment for thrombosis, the higher the risk of pulmonary embolism. Pulmonary embolism is much more difficult to treat than thrombosis in the leg and is therefore often fatal.
Read more on this topic: Post-thrombotic syndrome
Length of incapacity for work
Whether a thrombosis results in partial or complete incapacity for work depends on the type of work and the severity of the illness.
In principle, the attending physician should always make a recommendation. Shortly after fibrinolysis (Thrombus dissolution) or surgery, the patient is on sick leave
People who do a job that is unfavorable to anticoagulant (for example stuntmen, hard work, construction work) should not continue their work or be transferred to a different position at the workplace. However, long sitting times should also be avoided. Special information can also Patient training that are targeted by health insurance companies and some hospitals.
Prevent thrombosis
In everyday life you can do a few things yourself to prevent thrombosis in the leg. The most important point here is sufficient exercise. It is particularly important for people with office jobs or people who are on the spot a lot to exercise regularly. Movement that uses the leg muscles, for example going for a walk or walking, is most likely to be recommended.
Support stockings or compression bandages can also be integrated into everyday life to reduce the risk of thrombosis.
What you should also pay attention to is always drinking enough so that the fluid balance remains balanced. If there are hereditary risks, as in the case of thrombophilia, anticoagulant medicinal products must be used. In addition to heparin, coumarin derivatives such as Marcumar® are also administered.Regular blood tests must be done by the doctor while taking this medication, as heparin and coumarins increase the risk of bleeding.
Read more on the topic: Thrombosis prophylaxis
Move
Exercise is so important because it promotes blood flow and promotes what is known as the muscle pump. As the muscles contract, they exert healthy pressure on the vessels. Therefore, exercise is a good prophylaxis against thrombosis.
During a thrombosis, however, the leg must not be moved too much. It should be stored up and immobilized.
How do you recognize a thrombosis on your leg yourself?
Since deep vein thrombosis is the most common type of thrombosis, its symptoms are mainly described here. In 50% of the cases, the deep vein thrombosis proceeds without symptoms. Unfortunately, only about 10% of all thromboses show a typical triple constellation: The affected leg is swollen, bluish and the patient feels you dull pain.
Further complaints set in Tension- or Heaviness the affected leg is warmer than the healthy one and the veins are more visible on the skin. If the thrombus is in the lungs, patients complain of one Sudden shortness of breath, dizziness or weakness. Sometimes such patients also faint. You breathe faster and harder and have chest pain.
A dreaded complication is the occlusion of all veins in a leg. This can occur, for example, if the thrombosis is not treated for too long (several hours or days). Here the swelling becomes so strong that the arterial vessels (those with the oxygen-rich blood) are also squeezed off and the leg no longer receives enough oxygen. The leg is then at risk of dying and therefore an emergency operation should be carried out very quickly to clear the blocked vessels
pregnancy
pregnancy and the puerperium are factors that greatly increase the risk of developing a thrombosis in the leg. Actually are thrombotic diseases the leading cause of death during pregnancy and shortly after the birth.
This results from the hormonal change of the body during pregnancy. Pregnancy hormones like that progesterone expand the veins so that the blood can flow slowly, thus promoting thrombosis. Women with High risk pregnancies, those bed rest are particularly at risk, as there is also no daily exercise. With increasing Growth of the baby is gradually becoming one greater pressure on the veins exercised in the abdomen. Thus, the risk of blood clots is also increased there due to the slowed blood circulation.
During one normal pregnancy the woman should always be careful to get enough exercise. If you sit for a long time, you should go through it every now and then get up and walk around or go for a walk. Compression stockings and possibly treatment with heparin also help prevent thrombosis in the leg during pregnancy. However, heparin is only administered if there is really a very high risk of thrombosis, as there are as few as possible during pregnancy Medication should take in order not to harm the unborn child.
Symptoms in Pregnancy
During childbirth, the body tries to clot as much as possible because it wants to prevent high blood loss. That is why the woman giving birth should be monitored and sensitive to, especially after the birth process sudden new pain in the limbs. The symptoms are the same as in (leg vein) thrombosis or pulmonary embolism.
After operations
Postoperatively, i.e. after an operation especially the elderly longer to bed rest Committed. immobility promotes however the emergence of Thrombosis, especially from thrombosis in the legs. With the risk of thrombosis, of course, the risk of dangerous secondary diseases such as pulmonary embolism also increases.
Between the Difficulty of the operation and the Risk of thrombosis exists a context. High-risk operations, such as hip operations or the surgical procedure after one Multiple trauma (Multiple injury) carry an increased risk of venous thrombosis in the leg while General surgical operations only one moderate risk for thrombosis.
In order to prevent thrombosis in the leg and its consequences, it is important that patients as early as possible and under professional guidance mobilized from bed become. Wearing thrombosis stockings and that Injecting heparin also support thrombosis prophylaxis. When treating with heparin as an injection, blood parameters must be monitored, as the medication may otherwise increase the risk of bleeding.