Cause of coronary artery disease
Cause of coronary artery disease
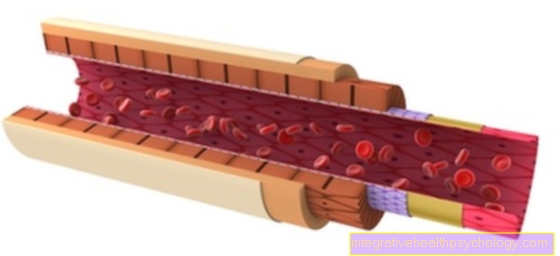
The leading cause of the development of coronary heart disease is atherosclerosis (hardening of the arteries), which is due to a reduced blood flow through the coronary arteries. The degeneration processes taking place in large and medium-sized arterial vessels lead to a narrowing of the vessel cross-section (lumen) and thus to a lower supply of the downstream organs or even a complete lack of blood flow in the associated supply area. Infarcts occur (interruption of vascular nutrition) in the flow area of the vessels and tissue dies; in the case of the coronary arteries, it is heart muscles that go under.

Elevated blood lipids as a cause of coronary artery disease
Coronary artery disease is caused by arteriosclerosis (hardening of the arteries), also known as atherosclerosis. Although it is popularly referred to as calcification, it is less a matter of calcium deposits than deposits of fats and blood components on the inner wall of the arteries. Atherosclerosis usually develops slowly over years and does not cause any symptoms for a long time. If the blood vessel is so blocked that the blood flow is impaired, symptoms occur. Elevated blood lipids play an essential role in the development of arteriosclerosis, which leads to coronary artery disease. Cholesterol, one of the essential components of blood lipids, is an important part of the plaques that develop in arteriosclerosis and increasingly narrow the blood vessels. Nowadays, however, cholesterol is no longer cholesterol, but a distinction is made between two types of cholesterol. The HDL (high density lipoprotein) and the LDL (low density lipoprotein). The LDL is, so to speak, the bad and the HDL the good cholesterol. Therefore, if the cholesterol level in the blood is high, a differentiation should always be made between these two types in order to better assess whether the bad cholesterol is actually too high. Because it is known that high LDL levels are an important risk factor for developing coronary artery disease, there are specific recommendations for lowering blood lipids. Patients who have not yet had coronary artery disease but who exceed a certain LDL value should take measures that contribute to lowering the LDL value. These measures include changing your diet and, if necessary, taking cholesterol-lowering tablets. The more previous illnesses the patient has with elevated blood lipids, the sooner a cholesterol-lowering therapy should be started. Patients who already have coronary artery disease should usually always take cholesterol-lowering drugs. Elevated blood lipids are a major risk factor in the development of coronary artery disease. Therefore, regular blood tests should be carried out, which also include blood lipids. If there are other risk factors for the development of coronary heart disease or if the LDL values are very high, a drug-based cholesterol-lowering therapy should be discussed with the family doctor.
Read more on this topic at: Hypercholesterolemia
Hardening of the arteries
Atherosclerosis (hardening of the arteries) is therefore an important development factor for the reduced oxygen supply to the heart muscle cells and the reduced blood flow to the heart. This condition of undersupply of the heart is known as coronary insufficiency and defines the disease "coronary artery disease":
The coronary arteries (coronary arteries) are no longer able to ensure sufficient flow (perfusion) of the vessels supplying the heart (coronary insufficiency).
High blood pressure as a cause of coronary heart disease
High blood pressure is another major risk factor for the development of arteriosclerosis and thus for the development of coronary heart disease. From one arterial hypertension (High blood pressure) one speaks from a chronic high blood pressure of over 140/90 mmHg. The number of people dying from coronary artery disease increases almost linearly with increases in blood pressure. 10 out of 10,000 people with normal blood pressure values die of coronary artery disease compared with 60 out of 10,000 people with chronic blood pressure values above 180 mmHg. High blood pressure is the most common risk factor for coronary heart disease and therefore urgently needs to be recognized and treated.
You might also be interested in this topic: high blood pressure
Diabetes mellitus as a cause of coronary artery disease
Diabetes mellitus is also an important risk factor for arteriosclerosis. Long-term, uncontrolled diabetes mellitus leads in most cases to pathological changes in the large and small blood vessels. Coronary artery disease is an example of changes in large blood vessels. Calcifications and deposits develop inside the blood vessels. This leads to increasing circulatory disorders. In the case of diabetes, sugar control is a decisive criterion in order to avoid secondary damage such as coronary artery disease as much as possible.
You might also be interested in this topic: Consequences of diabetes
Smoking as a cause of coronary artery disease
Smoking, like high blood pressure, elevated blood lipid levels and diabetes mellitus, is one of the most important risk factors for the development of arteriosclerosis, which in turn can lead to coronary artery disease. The ingredients in cigarette smoke encourage plaque formation. People who smoke are two to five times more likely than non-smokers to die of a heart attack caused by coronary artery disease. If you already have coronary artery disease, quitting smoking can reduce the risk of cardiac complications, such as a heart attack, by up to 50%. Patients who already suffer from coronary artery disease should therefore urgently give up smoking completely. In order to prevent the development of coronary heart disease, however, young healthy people should also give up smoking as completely as possible.
Further information on this topic can be found at: Circulatory disorders caused by smoking
Obesity as a cause of coronary artery disease
Obesity is also an important risk factor for the development of coronary heart disease. Obesity is also a risk factor for numerous other diseases such as diabetes mellitus or high blood pressure. Patients who already have coronary artery disease should aim for a normal weight through diet changes and regular moderate physical activity. But even (still) healthy patients who are overweight should try to lose weight early on and as a preventive measure in order to avoid the numerous, sometimes serious, secondary diseases associated with being overweight.
Also read: Consequences of being overweight
Stress as a cause of coronary artery disease
Chronic stress is not healthy for the body. He is suspected of being a risk factor for numerous physical and mental illnesses. Indeed, stress increases the risk of developing coronary heart disease. There is even a relatively clear dose-effect relationship here. The more stress, the higher the risk of developing coronary heart disease. Overall, sustained high stress leads to a moderate increase in the risk of developing coronary heart disease. However, there is not just this direct interaction between stress and heart disease. A large study examining the influence of stress on the development of coronary artery disease found that stressed people eat less healthily, are less physically active and are more prone to obesity. Obesity itself is an independent risk factor for the development of coronary heart disease.
You might also be interested in the following topic: Consequences of stress
Male sex as a cause of coronary artery disease
Overall, men are 1.5 to 2 times more likely to develop coronary artery disease than women. After the menopause, however, the incidence of the disease increases in women, so that hormonal factors are most likely to be the reason for the more frequent occurrence of coronary artery disease in men. If certain risk factors are present, the risk of women suffering from coronary artery disease can also increase significantly. One study showed that women with diabetes mellitus are twice as likely to develop coronary heart disease as diabetic men. The male sex is therefore a genetic and therefore unchangeable risk factor for the development of coronary heart disease.
Sedentary lifestyle as a cause of coronary artery disease
A lack of exercise is not a real risk factor in its own right for the development of coronary artery disease. However, people who regularly exercise moderate physical exertion are less prone to high blood pressure, often have better blood lipid values, are less likely to develop diabetes mellitus and are less likely to be overweight. Since high blood pressure, obesity, increased blood lipids and diabetes mellitus are all major risk factors for the development of coronary heart disease, a lack of exercise can indirectly promote the development.
Unhealthy diet as a cause of coronary artery disease
An unhealthy diet is not a direct risk factor for developing coronary artery disease. However, a low-fiber, high-fat, high-calorie diet with little intake of fruit and vegetables leads to numerous secondary diseases, which in turn can be a risk factor for the development of heart disease. For example, persistent unhealthy diet often leads to obesity. Obesity is a risk factor for numerous diseases, including coronary artery disease. In addition, a persistent, unbalanced high-fat diet can lead to increased blood lipids (Hypercholesterolemia) to lead. Hypercholesterolemia, in turn, is a major risk factor for the development of coronary artery disease and should be treated in good time. Indirectly, an unhealthy diet definitely influences the cardiovascular system and the development of coronary heart disease.
Read more on the topic: Diet for heart disease
Risk factors
Since the most common cause for coronary artery disease is atherosclerosis, the risk factors for the development of CHD are largely identical to those of atherosclerosis - development (hardening of the arteries):
The following factors increase the risk of developing coronary heart disease:
- increased total cholesterol in the blood
- excessive lipoprotein a level in the blood
- Age: The risk of developing CHD increases from the age of 30 with increasing age in men and after menopause in women.
- Gender: Men before the age of 60 are twice as likely to develop CHD as women; after the age of 60, the risks for both sexes become the same.
- Obesity
- little physical activity
- Diabetes mellitus
- high blood pressure
- Smoke
-
Psychological and social factors:
Studies have shown that stress and low social status are associated with an increased risk of CHD. -
genetic predisposition:
If CHD has already occurred in the family, the risk of cardiovascular events such as CHD, heart attack or sudden cardiac death is higher for family members.
Additional reasons
Further reasons for coronary insufficiency are compression of the coronary arteries due to an enlarged left ventricle (left ventricular hypertrophy), decreased diastolic blood pressure (second value when specifying the blood pressure; it represents the pressure conditions of the venous vascular system) with e.g. a patient with circulatory shock or a shortened diastole, the relaxation phase of the heart in which the coronaries fill with blood.
The oxygen supply to the heart is also reduced if the oxygen content in the blood is low (hypoxemia) as a result of lung diseases or anemia (anemia).
A disproportion between the supply and demand of oxygen can be due not only to the reduced supply but also to an increase in the oxygen demand. If there are heart valve defects (Vitien), heart failure or a heart attack, the wall tension of the heart is increased, which causes an increased need. Does the heart have to work extra, e.g. longstanding high blood pressure (Hypertension), an enlarged heart muscle (myocardial hypertrophy) or an increased cardiac output due to an overactive thyroid gland (hyperthyroidism) or infections, his need for oxygen increases.
The increasing narrowing of the coronary arteries limits the coronary reserve,
i.e. the blood flow to the coronary arteries cannot be increased adequately under stress, so that the oxygen supply situation in the heart occurs.
The length of the narrowing point (stenosis) in the vessel and the location of the stenosis are of decisive importance for the prognosis of coronary heart disease.
Vascular disease
The heart muscle is supplied via the right and left coronary arteries and the circumflex branch, which arises from the left coronary artery. Depending on how many of these three large coronary vessels are closed or narrowed, one speaks of a one-, two- or three-vessel disease. The supply of the Heart muscle is more and more restricted as the number of occluded vessels increases, and especially when the left coronary artery is affected. A second, important supply vessel of the heart arises from it with the ramus circumflexus.
In stable angina pectoris, the wall deposits of the vessels (plaques) that cause the narrowing of the lumen are fixed, i.e. they lie firmly against the arterial wall. However, if these wall supports are torn down, a unstable angina pectoris or a heart attack triggered if the vascular clearing is partially or completely blocked.
Classification
It will 4 degrees of severity of coronary narrowing differentiated according to the reduction of the vessel cross-section:
- Grade I is when the diameter is 35-49% smaller
- Grade II shows a reduction of 50-74% (significant stenosis)
- Grade III means a narrowing of 75-99% (critical stenosis) and at
- Grade IV is a complete occlusion or a 100% reduction in the vessel diameter.